ORIGINAL RESEARCH
Profile of leprosy patients at a reference center in a Brazilian state
Ana Débora Assis MouraI; Eliane Regina de Oliveira AlbuquerqueII; Emilia Soares ChavesIII; Adriano Rodrigues de SouzaIV; Guldemar Gomes de LimaV; Cristianne Soares ChavesVI
I
Nurse. PhD student in Public Health. Master in Nursing. Employee of the
Health Secretariat of the State of Ceará. Fortaleza, Ceará, Brazil. E-mail: anadeboraam@hotmail.com
II
Nurse. Graduated from the Integrated Faculty of Grande Fortaleza. Brazil.
E-mail: anadeboraam@hotmail.com
III
Nurse. PhD in Nursing. Nurse. Adjunct Professor, University of
Luso-Afro-Brazilian Integration. Fortaleza, Ceará, Brazil. E-mail: emilia@unilab.edu.br
IV
Nurse. Lecturer at the University of Fortaleza. Brazil. E-mail: adrianorsouza@gmail.com
V
Nurse. Specialist in Family Health at the School of Public Health of Ceará.
Fortaleza, Ceará, Brazil. Brazil. E-mail: guldemar@hotmail.com
VI
Nurse. PhD student in Public Health. Employee of the Health Secretariat of
the State of Ceará. Brazil. E-mail:
cristiannechaves@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.27774
ABSTRACT
Objective : to describe the profile of leprosy patients in a Dermatology Referral Center. Methods: this is a descriptive research with 469 medical records in Fortaleza, Ceará, Brazil. Thestudy was approved by Ethics Committee (nº68 / 2011). Results: leprosy was most incident among males than in females; the Borderline clinical form predominated; the predominant age ranged from 37 to 53 years; patients without primary education predominated; 63.8% had an income between zero and two minimum wages; most were retired; as regards to the degree of physical disability, 66.7% had Degree 0, 21.5% Degree 1, and 11.8% Degree 2; and as for the final physical disability, 62.7% had Degree 0; 9.8% Degree 1 and 4.3% Degree 2. Conclusions: it is expected the development of actions for the training of health professionals seeking an early diagnosis, treatment and follow-up of cases, as well as enlighten the public to prevent the onset of disabilities.
Keywords : Leprosy; profile; health; assistance.
INTRODUCTION
Leprosy is a disease surrounded by stigma and prejudice that leaves physical or emotional marks on individuals and is associated with low family income, malnutrition, low educational level, poor health conditions, among others1.
The poverty in which many people live means insufficient economic conditions to have their desires fulfilled and to value their lives. The lack of resources can negatively influence the living conditions and the development of diseases of an individual, besides being a factor that will influence the choice, evaluation and adherence to a proposed treatment 2.
Besides individual conditions, the risk of becoming ill is related to poor living conditions, poor health care and socioeconomic factors such as accelerated population growth and the large migration from rural to urban areas uncoupled with proper monitoring of urban structure for assuring the quality of life of these populations3.
Leprosy occurs in several countries around the world, affecting men and women in different age groups and different socioeconomic conditions. The difference between the sexes has decreased in the last years. The disease affects the women's full reproductive capacity and labor performance, but the incidence among the male population is still superior4.
For some authors, future complications are implied by the fact that the disease is highly disabling. Thus, early diagnosis and appropriate treatment may prevent the installation of physical disabilities, which represent one of the aspects that prevent individuals from exercising daily work and social activities and worsens their precarious living conditions 5.
According to data from the Brazilian Ministry of Health, the prevalence rate for leprosy has dropped by 68% in the last ten years, from 4.52/10,000 inhabitants in 2003 to 1.42/10,000 inhabitants in 2013. The overall detection rate of the disease was 12.14/100,000 inhabitants in 2014, corresponding to 24,612 new cases. Among the population under 15 years of age, 1,793 new cases were recorded. As a result, Brazil remains with two wicked titles: the only country in the world that has failed to eliminate the disease, and the country that has more new cases of the disease each year6.
Several factors such as delayed diagnosis, control of communicants, abandonment of therapy, reduced level of clarification, poor living conditions, poor health care and prejudice can influence the control of leprosy and high incidence rates affecting all regions of the country 7.
Another important aspect to be taken into consideration is that lack of information results in the little search and even abandonment of treatment on the part of customers, once leprosy is an infectious disease like any other and requires specific care, but with the peculiarity of being attached to prejudice and social stigma8.
Leprosy is an easily diagnosed, treated, and curable disease. The disease is a priority in public health care in the view of the Ministry of Health. The diagnosis is primarily clinical, with identification of signs and symptoms, preferably in basic care through the family health strategy (FHS). The commitment of Brazil with the international goals of eliminating the disease is expected9.
As benefits of this study, therefore, it is expected that health professionals know the profile of leprosy patients of a municipality which is a reference for the State of Ceará, and in this way, may reflect on their profile. In addition, the study aims to enable professionals to develop health actions for early diagnosis and treatment and consequent prevention of sequelae.
Thus, this study aimed to describe the epidemiological profile of leprosy patients diagnosed at a Dermatology Reference Center in a municipality in the State of Ceará, Brazil.
LITERATURE REVIEW
Leprosy is a chronic, infectious and contagious disease with slow evolution. The etiologic agent is Mycobacterium leprae, which mainly attacks the skin and peripheral nerves. Man is considered the main host of this agent and infection happens through the upper airways 10.
Transmission occurs through direct contact between non-treated affected patients with susceptible individuals. Most people are in contact with the bacillus every day, from which this disease has high infectivity. Because only a small minority of these people develop the disease, due to deficiency of the immune system that cannot fight the infection, the disease has low pathogenicity11.
The World Health Organization (WHO) has classified leprosy into two types, according to the bacilloscopic index, namely, paucibacillary (less than 2) and multibacillary (greater than or equal to 2). It has also established clinical criteria; paucibacillary cases would correspond to up to five cutaneous lesions and/or one nerve trunk affected whereas multibacillary cases would correspond to more than five cutaneous lesions and/or more than one nerve trunk affected. When bacilloscopic examination is available, patients with positive results are considered multibacillary regardless of the number of lesions12.
The loss of tactile, thermal and painful sensitivity corresponds to the main symptom of the disease. This happens because of intracellular agents harbored within cutaneous cells that block the conduction of nerve impulses, affecting mainly the innervations of the extremities13 .
Leprosy is a curable disease. However, because the incubation period varies from 2 to 7 years, some degree of physical incapacity or deformities may already be installed when the disease is diagnosed5.
Treatment is done through the use of polychemotherapy (MDT) during 6 to 9 months in the case of the paucibacillary group. For multibacillary patients, treatment requires a longer period, which can last from 12 to 18 months12.
With regard to health care, it is known that men are less favored with respect to access to these services. This generates, in the majority, mistrust, doubts, and low credibility attributed to diagnosis and treatment. Such conduct blurs the problem and often leads men to excessive consumption of alcoholic beverages, which would explain the gaps in the control and treatment of the disease14.
The appearance of the disease in men threatens the role of the male figure. Revolt, anxiety, restlessness, distrust, anger, fear and indifference are common reactions. As for women, they are concerned with disabling injuries and visible deformities that the disease can cause, and which may jeopardize their role within the family or at work15.
Scholars have demonstrated that the inability to manage household chores and child care are reasons that lead leprosy female patients to be abandoned by their partners or spouses, resulting in great emotional wear and feeling of worthlessness for domestic management16.
METHODOLOGY
The present article is a descriptive research with quantitative approach. The study was developed in 2012 in a Dermatology Reference Center that provides assistance and monitors patients from the entire State of Ceará undergoing leprosy treatment. This center is a public institution of secondary level linked to the Health Secretariat of the State of Ceará (SESA).
The study population consisted of 607 patients with leprosy diagnosed at the Reference Center in 2010 according to medical records. The sample consisted of 469 records of that year, which contained information pertinent to the study and which were within the pre-established period. We excluded 112 medical records that were incomplete and 26 medical records of patients who were not on file. Therefore, the study was carried out with 469 medical records.
Data collection was done by means of evaluation of the documentation, documentary research in database (medical records). These data were collected from the medical records of patients who underwent treatment at the Dermatological Center in 2010.
After data collection, the information was organized into twosoftwares, theStatistical Package for the Social Sciences (SPSS) and Excel 2007, where tables were created to provide a broad and overall view, giving determination and trustworthiness to the numbers found, for subsequent discussion and interpretation of results. These programs also provided support for the descriptive and statistical analysis of data collected. The variables surveyed included those referring to the profile of patients: gender, race, age, schooling, family income, occupation; clinical forms of leprosy; treatment; and degree of disability.
The following criterion was observed for assessment of disability: Level 0 - sensitivity preserved in the eyes, hands and feet; Level 1 - reduction of sensitivity in the eye(s), hand(s) and/or on foot (feet); Degree 2 - multiple impairment in the eye(s); hand(s) and/or foot (feet) with traumatic injuries and/or presence of claw(s) and/or bone resorption.
Prior to data collection, the study was submitted to the Research Ethics Committee and received favourable Opinion under nº 068/2011.
RESULTS AND DISCUSSION
The profile of patients, based on clinical forms and socio-demographic data, is analyzed below.
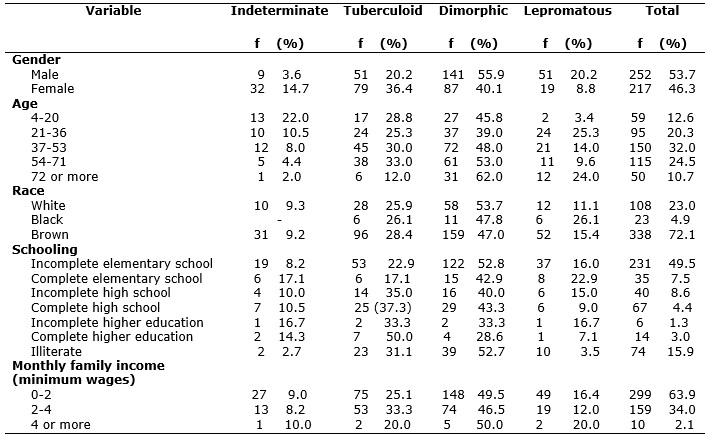
Regarding sex, leprosy affected more men than women. Male patients represented 252 (53.73%) of the total sample (469), while the female patients corresponded to 217 (46.27%). See Table 1
TABLE 1:
Distribution of individuals according to clinical form of leprosy and
gender, age, race, level of education and income. Fortaleza-CE, 2012.
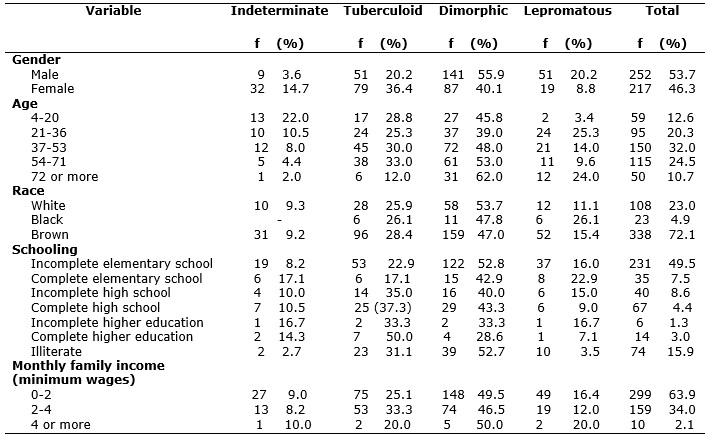
There are variations between detection rates in the sexes, with a predominance of higher rates in men. Studies in the Municipality of São Luís/MA and in Belém/PA4,17 have found similar results to those found in this study. However, there are exceptions in other cities and regions of Brazil, such as in Governador Valadares/MG and Campos dos Goytacazes/RJ, where 55.3% and 50.8%, respectively, of the patients affected by leprosy are women18.
The predominant clinical form in both sexes was the Dimorphic, with 141 (55.95%) cases among men and 87 (40.09%) among women, followed by the Tuberculoid with 51 (20.24%) and 79 (36.41%) cases, the Lepromatous with 51 (20.24%) and 19 (8.75%) cases, and the Indeterminate with 9 (3.57%) and 32 (14.75%) cases. The clinical forms considered to be the most serious and contaminant of this pathology, i.e. the Dimorphic and the Lepromatous, were recorded in this study as the forms that most affect males, specifically 76.19% of these patients.
A study carried out from July 2007 to July 2008 in the municipality of São José do Rio Preto/SP found frequencies of clinical forms in men and women, respectively, as follows: Dimorphic (50%; 34.2%), Lepromatous (30.8%, 16.7%), Tuberculoid (16.3%, 22.5%) and Indeterminate (2.9%, 26.7%). The Dimorphic form was predominant, affecting 41.5% of a sample of 359 patients, which is similar to the results found in the present study 19.
When comparing the sequence in which the clinical forms occurs in the genders, this study showed a difference between the Tuberculoid and Lepromatous forms. This is significant in comparison to other municipalities, as the Tuberculoid form is considered a non-contagious form of the disease.
Regarding the age group, the group of 37 to 53 years prevailed, with 150 (32%) patients. As it happened with genders, the Dimorphic clinical form predominated, affecting 72 (48%) patients. In the case of patients aged 72 years or older, the Indetermined form was the least prominent form, identified in only 1 (2%) individual. See Table 1. Based on all medical records studied, patients had an average age of 46 years and a Variation Coefficient of 42.15%, which shows the extensive dispersion of the ages.
In this study, with the exception of the elderly, the disease had the lower incidence in the age group of 4-20 years, representing 59 (12.6%) cases.
As for race, three types occurred: white, black and brown. It was observed that the brown color predominated with 338 (72.1%) subjects, followed by the white, with 108 (23%) subjects, and the black, with only 23 (4.9%), as shown in Table 1.
A study on the epidemiological profile of leprosy in a Brazilian municipality carried out from 2000 to 2006 found that in the race/color evaluation, brown-skinned people were the majority, with 33.4% of the cases, followed by whites with 29.8 %, and the black race representing the lowest proportion, with 20 subjects. These data are similar to those presented in the present study.
As for schooling, patients who had not finished elementary school - 231 (49.5%) - represented almost half of the whole sample, followed by illiterate patients -74 (15.8%) - and patients who had completed high school - 67 (14.3%) - and higher education - 14 (3%). See Table 1.
The low level of schooling in the case of the majority of the analyzed patients may reflect in less professional possibilities of employment and consequent low wages and unfavorable socioeconomic conditions.
Regarding monthly family income, the majority - 299 (63.8%) - had family income between zero and two minimum wages, followed by 159 (34%) patients with income between two and four minimum wages, and only 10 (2.1%) with income greater than or equal to four minimum wages. From the foregoing, the presence of leprosy among less favored economic social classes is confirmed.
Caution is needed when stating that leprosy is a disease typically linked with poverty, but we can say that people with low socioeconomic status who have unsatisfactory food and housing are at greater risk of acquiring communicable diseases compared to people with good quality of life 21.
As for occupation of the patients, there was a predominance - 85 (18.12%) - of retirees; 73 (15.57%) worked in domestic services; 57 (12.2%) were students; 24 (5.12%) worked in agriculture; and 20 (4.26%) in trade. See Table 2. Information on occupation was not available in 210 medical records.
TABLE 2:
Distribution of individuals according to clinical form of leprosy and
occupation. Fortaleza-CE, 2012.
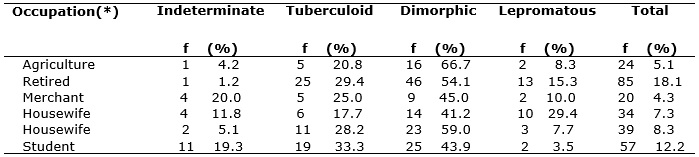
(*) Information on occupation was missing in 210 medical records.
Regarding treatment, results led to the conclusion that the most used in this study was the multibacillary, for 299 (63.8%) patients; this was also the most indicated treatment in leprosy of the Dimorphic form for 206 (68.9%) patients. The paucibacillary treatment was applied in 170 (36.3%) cases, being mostly used in Tuberculoid leprosy, in 117 (68.8%) cases. See Table 3.
TABLE 3:
Distribution of individuals according to clinical form of leprosy,
treatment and degree of disability. Fortaleza-CE, 2012.
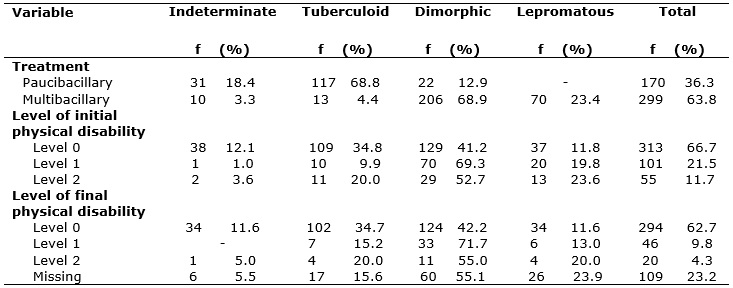
Regarding the degree of physical disability detected at the diagnosis of the disease, the data revealed that all the patients had been evaluated for degree of initial physical disability. Of these, 313 (66.7%) presented Level 0; 101 (21.5%) Level 1; and 55 (11.8%) Level 2. In turn, the level of final physical disability, that is, after completion of the therapeutic regimen, 294 (62.7%) presented Level 0; 46 (9.8%) Level 1; 20 (4.3%) Level 2; and 109 (23.2%) did not make the test. See Table 3. According to information in the medical records, the absence of patients in the final physical evaluation was due to a variety of reasons, among them non-attendance, abandonment of treatment, transference and death.
In this study, the high rates of cases with physical disability at the beginning and the end of treatment seem to show that leprosy diagnoses still occur late, contributing to prevalence of complications of this disease. Physical disabilities and deformities are among the main grievances caused by the disease. They may cause or endorse prejudice, as well as contribute to social exclusion and interfere with daily activities and work22.
When patients initiate the therapeutic regimen without any type of disability and when they stick to the guidelines of health professionals throughout the treatment, even if they are subject to clinical evolution of the disease, to immunological response to bacillus and to medication use, they are less likely to develop deformities and physical disabilities 23.
The decentralization of health actions in primary care allows greater access to the population. The change in the care model brought about a new paradigm related to the substitution of a model based on medical specialties by a model centered on health surveillance, with emphasis on individuals and families. Integral assistance to leprosy patients requires the organization of multidisciplinary teams in medium and high complexity primary care, so that they may provide care to each case within its needs and under the principles of equity and comprehensiveness24.
As for patients' origin, it was noticed that 41 (8.9%) live in the Metropolitan Region, 363 (77.3%) live in Fortaleza, and only 65 (13.8%) live in the country side of the State of Ceará. I another study carried out in the city of Fortaleza/CE, the majority of patients came from the capital and from municipalities of the Metropolitan Region, representing 82% of registered cases25.
CONCLUSION
The male gender was more affected by leprosy than the female, especially by the most severe forms, and the mean age indicated economically active patients. The Dimorphic form of leprosy was the most incident.
Brown skinned people were majority in the sample, confirming the strong miscegenation of the population in the state of Ceará.
The low level of education observed in the majority of the cases was consistent with the predominance of occupations in service sectors whose tasks do not require qualification and result in low profitability.
The high percentage of physical disabilities at the beginning and at the end of the treatment indicates that encouragement to earlier diagnosis and improvement of the quality of health care are necessary.
The majority of patients came from peripheral regions of the city, where clusters of people live under precarious housing conditions associated with poor socioeconomic and cultural profile. A differentiated look is needed toward these places, as they consolidate characteristics of continuous outbreaks of disease transmission.
It is necessary to train health professionals for early diagnosis, treatment and follow-up of cases in basic health units, as well as to clarify the population about signs and symptoms of this disease and about the need to seek therapeutic treatment in order to prevent the appearance of disabilities.
The absence of statistical tests of association between variables represents a limitation of the study, as this prevents the identification of certain important characteristics as variables that could contribute to the incidence of leprosy cases in the State of Ceará.
REFERENCES
1.Nunes JM, Oliveira ENV Cunha NF. Hanseníase: conhecimentos e mudanças na vida das pessoas atingidas. Ciênc Saúde Coletiva. 2011; 16 (suppl 1): 1311-8.
2.Imbiriba EB, Hurtado-Guerrero JC, Garnelo L, Levino A, Cunha M G, Pedrosa V. Perfil epidemiológico da hanseníase em menores de quinze anos de idade, Manaus (AM), 1998-2005. Rev Saude Publica. 2008; 42 (6): 1021-6.
3.Alencar CHM, Barbosa JC, Ramos Júnior AN, Alencar MJF , Pontes RJS, Castro CGJ,et al Hanseníase no município de Fortaleza, CE, Brasil: aspectos epidemiológicos e operacionais em menores de 15 anos (1995 - 2006). Rev Bras Enferm. 2008; 61 (esp.): 694-700.
4.Castro SMS, Watanabe HAW. Isolamento compulsório de portadores de hanseníase: memória de idosos. História, Ciências, Saúde. 2009; 16 (2): 449-87.
5.Duarte MTC, Ayres JÁ, Simonetti JP. Consulta de enfermagem: estratégia de cuidado ao portador de hanseníase em atenção primária. Texto Contexto - Enferm. 2009; 18 (1): 100-7.
6.Fundação Oswaldo Cruz. Hanseníase: Brasil é o único país que não conseguiu eliminar sua propagação. 2015 [citado em 03 abril 2016]. Disponível em: http://portal.fiocruz.br/pt-br/content/hanseniase-reducao-de-casos-nao-sera-suficiente-para-que-o-pais-elimine-doenca-ate-o-fim-de .
7.Amaral EP, Lana FCF. Análise espacial da hanseníase na microrregião de Almenara, MG, Brasil. Rev Bras Enferm. 2008; 61: 701-7.
8.Opromolla PA, Laurenti R. Controle da hanseníase no estado de São Paulo: análise histórica. Rev Saude Publica. 2011; 45 (1): 195-203.
9.Aquino CMF, Rocha EPAA, Guerra MCG, Coriolano MWL, Vasconcelos EMR, Alencar EN. Peregrinação (Via Crucis) até o diagnóstico da hanseníase. Rev enferm UERJ. 2015; 23 (2): 185-90.
10.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Doenças infecciosas e parasitárias: guia de bolso. 8ª ed. Brasília(DF): Editora MS; 2010.
11.Mendonça VA, Melo GEBA , Teixeiera AL. Imunologia da hanseníase. An Bras Dermatologia. 2008; 83: 343-50.
12.Lastória JC, Abreu MAMM. Hanseníase: diagnóstico e tratamento. Diagn Tratamento. 2012; 17(4):173-9.
13.Morais JP, Torritezi K, Silva TAAS, Martin YC. Visão da população do Município de São Paulo quanto à ocorrência da hanseníase e seu comportamento para a prevenção. Rev Ciênc Saúde. 2009; 27 (3): 201-5.
14.Bittencourt LP, Carmo AC, Leão AMM, Clos AC. Estigma: percepções sociais reveladas por pessoas acometidas por hanseníase. Rev enferm UERJ. 2010; 18 (2): 185-90.
15.Pereira EVE, Machado HAS, Ramos CHM, Nogueira LT, Lima LAN. Perfil epidemiológico da hanseníase no município de Teresina, no período de 2001-2008. An Bras Dermatologia. 2011; 86 (2): 235-40.
16.Martins PV, Caponi S. Hanseníase, exclusão e preconceito: histórias de vida de mulheres em Santa Catarina. Ciênc Saúde Coletiva. 2010; 15 (supl.): 1047-54.
17.Chaves HM, Cunha M, Mariano G, Macedo M, Batista KNM, Xavier MB, et al. Avaliação clinico-epidemiologica em pacientes multibacilares em uma unidade de referencia em hansenologia da Amazonia. Hansenologia Internationalis. 2008; 8 (33): 9-16.
18.Batista ES. Perfil sócio-demográfico e clínico-epidemiológico dos pacientes diagnosticados com hanseníase em Campos dos Goytacazes, RJ. Rev Bras Clin Médica. 2011; 9 (2): 101-6.
19.Arantes CK, Garcia MLR, Filipe MS, Nardi SMT, Paschoal VDA. Avaliação dos serviços de saúde em relação ao diagnóstico precoce da hanseníase. Epidemiol Serv Saúde. 2010; 19 (2): 155-64.
20.Miranzi SSC, Pereira LHM, Nunes AA. Perfil epidemiológico da hanseníase em um município brasileiro, no período de 2000 a 2006. Rev Soc Bras Med Tropical. 2010; 43 (1): 62-7.
21.Montenegro RMN, Molina MDC, Moreira M, Zandonade E. Avaliação nutricional e alimentar de pacientes portadores de hanseníase tratados em unidades de saúde da Grande Vitória, Estado do Espírito Santo. Rev Soc Bras Med Tropical. 2011; 44 (2): 228-31.
22.Lana FCF, Carvalho APM, Davi RFL. Perfil epidemiológico da hanseníase na microrregião de Araçuaí e sua relação com ações de controle. Esc Anna Nery. 2011; 15 (1): 62-7.
23.Rodini FCB, Gonçalves M, Barros ARSB, Mazzer N, Elui VMC, Fonseca MCR. Prevenção de incapacidade na hanseníase com apoio em um manual de autocuidado para pacientes. Fisioterapia e Pesquisa. 2010; 17,(2): 157-66.
24.Lopes FN, Lana FCF. Participação popular no controle da hanseníase: um desafio para o serviço de saúde. Rev enferm UERJ. 2015; 23(2): 235-40.
25.Gomes CCD, Pontes MAA, Gonçalves HS, Penna GO. Perfil clínico-epidemiológico dos pacientes diagnosticados com hanseníase em um centro de referência na região nordeste do Brasil. An Bras Dermatologia. 2005; 80 (3): 283-8.