ORIGINAL RESEARCH
Euthanasia and dysthanasia: doctors' and nurses' perceptions in a town in southern Minas Gerais
Meire Marques GuimarãesI; Marina Andrade Ferreira de CarvalhoII; Ivandira Anselmo Ribeiro SimõesIII; Rogério Silva LimaIV
I
Nursing student of the 8th period at the Nursing School
Wenceslau Braz. Itajubá, Minas Gerais, Brazil. E-mail: meire_marquesg@hotmail.com
II
Nursing student of the 6th period at the Nursing School
Wenceslau Braz. Itajubá, Minas Gerais, Brazil. E-mail: andrade_mah@hotmail.com
III
Nurse, Master in Bioethics by the University of Vale do Sapucaí. Professor
at the Nursing School Wenceslau Braz. Itajubá, Minas Gerais, Brazil.
E-mail:
ivandiranselmors@ hotmail.com
IV
Nurse, Master in Nursing by the Federal University of Alfenas. Professor at
the Federal University of Alfenas. Alfenas, Minas Gerais, Brazil. E-mail:
rogério.lima@unifal-mg.edu.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.9545
ABSTRACT
Objective: to understand doctors' and nurses' perceptions of euthanasia and dysthanasia. Method: in this exploratory, qualitative study of a snowball sample of 10 doctors and 10 nurses at two hospitals in southern Minas Gerais, data were collected in 2012 and 2013 by semi-structured interviews with two open questions. The interviews were recorded and analyzed using Collective Subject Discourse. Results: interviewees were observed to perceive the topic as complex and little discussed in academic circles. Conclusion: the boundaries between dysthanasia and orthothanasia are not precise in daily professional routine.
Keywords: Euthanasia; dysthanasia; doctors; nurses.
INTRODUCTION
Euthanasia is not only related to death but also of human dignity. Even today, it is not accepted by the Brazilian State, defined its practice as a crime. In this sense, euthanasia is a controversial issue, full of conflicts of fundamental values and principles that govern life and human dignity. Among health professionals, euthanasia is also taken as a singular complexity theme that is in daily professional actions, such as in situations related to consent to carry out euthanasia and the issue of incurability1.
It is known that the increase of suffering without the restoration of health often leads to waste of resources and generates a distress and disruption situation to the family, professionals and especially to patients2. Given the complexity of this phenomenon, based on the implications for the health work practice, more studies dedicated to exploring the issue of euthanasia and dysthanasia and their interrelationship to the ethical aspects of the actors involved in care the patient in the process of dying are necessary. Therefore, this study aimed to understand the perceptions of nurses and doctors of the hospital area on euthanasia and dysthanasia.
LITERATURE REVIEW
Euthanasia is understood as the use of means to seek for the death without suffering for an incurable ill person3. Euthanasia is understood as an assisted suicide by a decision coming from the patient4. Disthanasia, in turn, means a slow, anxious and with much suffering death, that is an unreasonable prolongation of life at any cost, when the time of death arrives5.
In this respect, dysthanasia practice cannot discern therapeutic interventions of those useless interventions. On the other hand and based on a biological perspective trying to control and medicalize all stages of the lifecycle, the emphasis should be aimed at the protection of human life seeing as a dignified death but also an inalienable right5.
It is noticed that some professionals feel guilty and have difficulties in treatment associated with the technological apparatus because they often do not accept the end of life. It is important to highlight the development of scientific technology has enabled the extension of life. However, not always die surrounded by high-technology is what the patient most needs at the time of his death.
Therefore, conditions to encourage the humanization are necessary, such as the understanding of the family, the support of friends and solidarity of health professionals. The several technological resources should provide a dignified death for the patient without pain and in peace. It is up to health professionals to understand the needs of the patient to be able to help him have a smooth passage6,7.
METHODOLOGY
This is a cross-sectional and descriptive study using the qualitative approach developed in 2012 in two general hospitals in a city in southern Minas Gerais. The study participants were 10 doctors and 10 nurses selected by purposive sampling criterion of Snowball type.
Data collection was performed using a semi-structured interview guide with two questions focused on the perceptions of the participants about euthanasia and dysthanasia. The interviews were recorded and transcribed in full. For data analysis, the Collective Subject Discourse method (CSD) was used, based on the Theory of Social Representations. Social representations inscribed in social psychology area aim to understand how the individual-society relationship occurs in the construction of knowledge and reality from the membership of the social, history and cultural area8.
The DSC method is a technique to reveal the thinking of the community through an understanding of current significances in the common sense of the social actors. Therefore, through this technique, it is sought the description of the collective thinking to subsidize its interpretation9.
By the tabulation of qualitative data of the speeches through testimonies, this methodological resource promotes understanding of social constructs not in the form of graphs and tables, but in a direct way, through the discourses9.
For the construction of the DSC, it was opted to use three methodological approaches: the key expressions (ECh), the central ideas (ICs), and the DSC itself. The ECh are excerpts of the verbal material of each statement in its entirety. The ICs describe the meaning synthetically in the depositions. The DSC is configured as the testimony of the group interviewed and placed in the first person singular, composed of the ECh and ICs, like the speech of a single individual9.
The study has preserved the ethical principles and was approved by the Ethics and Research Committee (CEP) of the Nursing Wenceslau Braz School (EEWB) under Nº 766/2011. Doctors have been identified by the letter D and nurses by the letter N, followed by the Arabic numeral to ensure privacy and anonymity.
RESULTS AND DISCUSSION
There were 6 (60%) doctors surveyed of the male gender, with a mean age of 32 years old among the respondents. The predominant religion was Catholic - 7 (70%). There were 7 (70%) doctors highlighted as postgraduates and 3 (30%) being enrolled in graduate school. The average professional activity time was seven years. As for nurses, 100% of respondents were female, with a mean age of 23 years old; 9 (90%) were Catholic; 9 (90%) were enrolled in graduate school; the average professional activity time was four years.
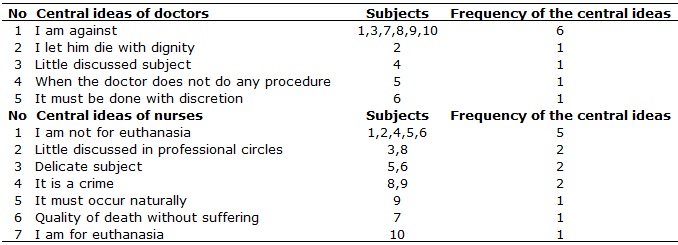
The discourse of the medical participants allowed the identification of the following IC: I am against; Let him die with dignity; Little discussed the subject; When the doctor does not do any procedure, and it must be done with discretion . In the nurses' speech, the ICs were: I am not for euthanasia; Little discussed in professional circles; Delicate subject; It is a crime; It must occur naturally; Quality of death without suffering and I am for euthanasia . See Table 1.
TABLE 1:
Central ideas, subjects and frequency of the central ideas of the topic:
Perception of doctors and nurses about euthanasia. Minas Gerais, 2012.
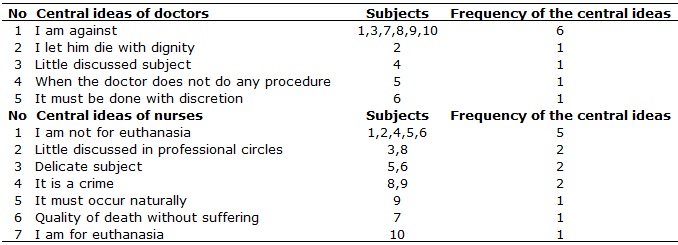
Euthanasia subject analysis allowed observing that the IC I am against euthanasia was the most frequent. Here is the testimony;
I do not agree to cause the death of the patient; we must seek to provide a good time for the patient. It is murder; it is prohibited by Brazilian law [...] I am Catholic, and I am against causing the death of another person (DSC1)
The expressed by the doctors in the DSC above meets the political and prominent religious discourse in Brazil since the country is predominantly Christian and religious beliefs are a major influence on the practice and acceptance of euthanasia9. In the same way, the DSC emerging from the IC Let him die with dignity advocates for life and of death with its natural course. Perhaps, this can be understood when examining the history of the medical profession, since the aggregate knowledge by professionals always developed to preserve life, thereby interventions that interrupt is difficult to be treated by doctors, even in the face of the impossible therapeutic10.
So it is difficult to answer, but we should not rush to help, but let the patient die with dignity (DSC2)
On the other side of the IC Little discussed, the following speech emerged:
Euthanasia is a method that needs to be better discussed in the country because sometimes it can alleviate the suffering, very selected situations, so I think that people should opine about it (DSC3)
Doctors do not agree with the practice of euthanasia since Hippocratic times. It is estimated that this behavior will remain to be a crime (punishable by incarceration from 2 to 4 years). However, it is observed that the professional practice and living with conflict situations on the dying process have led practitioners to question the training that the school has provided to them to deal with this issue. It does not seem clear and consistent for medical what interventions incur euthanasia and from at what time the therapeutic determine dysthanasia. Perhaps, there is the need for this issue to be further discussed in medical schools. The mitigating measures are those consistent with the fundamental principles of law, reasonableness, and proportionality2,11.
Regarding nurses, the IC that most prevailed were I am not for euthanasia:
I believe that euthanasia should not be practiced, and it has not happened in the environment where I work, by the workers profile, the multidisciplinary team that there act. I am not for euthanasia. (DSC4)
Also for most of the nurses, the idea of the practice of euthanasia seems unacceptable. It is believed that besides the contextual and common medical profession reasons, for nursing, the profession has since its inception a beneficent and religious nature that permeates today the social imaginary, thereby causing death would obviously an unacceptable practice12.
In the speech of the nurses, it was also found the IC Little discussed in the professional circles, where euthanasia is a complex issue that will always lead to new discussions and many questions. Thus, it is necessary the development of new research which intends to its detailed study in different contexts1. The following speech is highlighted:
Euthanasia is really little discussed in the workplace, even when the patient is terminally ill with a serious illness or not having any prognosis [...] There was a limit without any resource. It is a matter that should be discussed even ... (DSC5)
This dilemma shows that the phenomenon of death is debatable being a sensitive issue involving many situations13. In this regard, the IC, Delicate subject, derived from the speech:
It is a delicate subject. It involves not only the patient and the repercussions for the family, but the professional ethics of those involved [medical, nursing]. It is an extremely delicate matter, which involves life, death and also feelings, whether from the person or his families. (DSC6)
It is observed that, unlike the medical discourse, nurses expand the view on the subject considering the family and subjective aspects.
As for dysthanasia in the medical discourse, it was possible to identify the following IC: I am against it; It should be discussed, I have to do it; To promote the well being of the patient; It is selfish to take the patient´s right to opine, and We have to do the best within our limitations . For nurses, the ICs that most prevalent were: There is dysthanasia; It is quite complicated; It is an ethical issue, and I am against dysthanasia. See Table 2.
TABLE 2:
Central ideas, subjects and frequency of the central ideas of the topic:
Perception of doctors and nurses about dysthanasia. Minas Gerais, 2012.
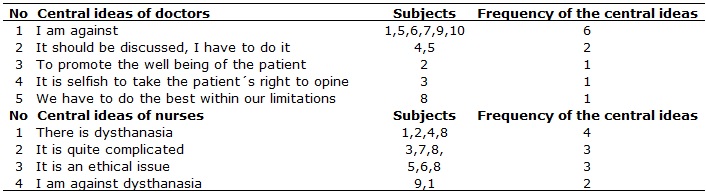
Doctors are against dysthanasia as the DSC:
Dysthanasia is a procedure that I totally disagree; I think that the goal of the medical and nursing staff, who are watching the patient do not have to extend the suffering of anyone. So, when you realize that the patient has no prognosis, and the more you intervene, you will achieve maximum extend a few days or a few weeks in his life without maintaining a minimum quality of life. This is not feasible, for example, you take an elderly patient with a chronic disease [...], with the use of vasoactive drugs, it will only prolong the suffering of both the patient and the family, so I am against dysthanasia (DSC7)
It is understood that human existence is singular and unique, and the way to treat its end, it should also be considered in the same context of uniqueness. However, the positioning on the terminal illness of life involves some situations of other social issues such as family, culture, religion, the patient and also the health professional. It is known that nowadays, people hardly die at home, but often surrounded by a technological structure in an intensive care unit8. Resolution Nº 1,805/2006 and the paragraph of Article 41 of CEM/2009 regulate the practice of orthothanasia and reprove the dysthanasia. It is noteworthy that the CEM was updated in 2010 including the ethical principles of palliative care in Article 412.
This may denote a social movement of rapprochement to the process of dying. This movement, maybe able to reframe death and re-insert it in the debate in academic and professional means meeting the professional, doctors and nurses aspirations. In this respect, in the medical discourse, the next IC can be identified, It should be more discussed, I have to do:
However, I think it has to be something very well discussed and well specified because it is difficult for you to decide which patient I will invest, or which patient I will not invest. So, I think it should be discussed further with the Ministry of Health to guide better clinicians regarding when to invest and when not to invest. Dysthanasia is something I am required to do, because if I do not do it, I go to jail (DSC8)
With the scientific and technological developments in health care, the improvement of technical and scientific conditions for the treatment and processing of patient care about the end of life determine a complex reality that requires professional positioning for palliative care to improve the quality of life of patients and their families12.
In this understanding, it is observed that the IC To promote the well being of the patient groups the perception of doctors in this regard:
The least that the doctor can do is to promote the welfare, acting and giving the minimum conditions to the patient, quality of life, comfort on pain, hydration, electrolyte balance, so you can do it without waiting for the natural evolution of the patient ( DSC9)
Professionals realizing the suffering and pain of others seek a way to evaluate it to provide comfort to patients and their families. However, the knowledge gained by health professionals is not sufficient to reduce all the suffering, and it is limited, often in physical care, forgetting the comprehensive care12.
This can be seen in the speech of nurses about dysthanasia, in which they state that dysthanasia occurs. It is noteworthy that at the time when they cannot achieve the goals of medical therapy, which is to preserve health or alleviating suffering, seems to come to cease useless measures and intensify efforts to assuage the discomfort of dying14.
I believe that when all forms are exhausted [of recovery] and he has not even cure, only care remains, and the staff insists on prolonging life with suffering, with drugs, even though he has no therapeutic possibility (DSC10)
The time between getting sick and dying in the last century was short, and today, this time, lasted, getting the person dying for a long time, thanks to the achievements of science and technology. However, in the hospital environment, there is the lack of means for discussions in this regard, death is considered negative, and there is some lack of preparation by health professionals6 to address this reality6,7,10,12-15.
As the doctors, there is a frustration of nursing professionals facing the death of the patient, because, during his undergraduate, the focus was to save lives at any cost. When this is not possible, these professionals are faced with the lack of preparation while experiencing various conflicts. Thus, they experience the process of dying as a loss, suffering, and distress when they should receive psychological counseling, accessible to all to learn to deal with these feelings15.
CONCLUSION
This research allowed understanding the perceptions of doctors and nurses regarding euthanasia and dysthanasia. It was possible to see that the issue is complex and requires more research to look into the issue, especially when realizing that both doctors and nurses pointed euthanasia and dysthanasia as little problems discussed in the school and professional environment.
It is suggested that the questions in the process of dying, including palliative care, are the subject of study and discussion among professionals working in the care and training of doctors and nurses. This can also be favored by the inclusion in the curriculum of a specific subject that favors the spaces for dialogue and construction of knowledge regarding the Thanatology.
REFERENCES
1.Bueno AAB, Fassarella CS. Euthanasia: discussing the relativity of bioethics. Rev Rede Cuid Saúde. 2011;5: 1-10.
2.Ribeiro KV, Soares MCS, Gonçalves CC, Medeiros IRN, Silva Gl, Euthanasia in terminal patient: medical and nurses concepts. Revista Enfermagem em Foco. Brasília, DF: Cofen. 2011;2: 28-32.
3.Santos JLG. Professional ethics: health professionals´ behavior facing life and death. Rev intensiva. 2008;3: 17-22.
4.Teixeira AT. Legal aspects of death and dying. In: Santos SF. Palliative care: discussing life, death and dying. São Paulo: Atheneu; 2009. p. 361-71.
5.Pessini L. Dysthanasia: Certain Bioethical reflections from the Brazilian reality. In: Santos SF. Palliative care: discussing life, death and dying. São Paulo: Atheneu; 2009. p. 319-45.
6.Batista RS, Schramm FR. Euthanasia: the paths of death and autonomy. Ciên saúde coletiva. 2008;9: 31-41.
7.Timby BK. Death and dying. In: Timby BK. Fundamental concepts and skills in nursing care. 6ª ed. Porto Alegre: Artmed; 2001.
8.Moscovici S. The social representation of psychoanalysis. Rio de Janeiro: Zahar; 1978.
9.Lefreve F, Lefreve AM. Research social organization: a quantitative and qualitative approach. Brasília (DF): Líber Livro; 2010.
10.Tittanegro GR. Bioethics and the end of life: physiological reflections on death. In: Malagutti W, organizer. Bioethics and nursing: controversies, challenges and achievements. Rio de Janeiro: Rubio; 2007. p.195-203.
11.Conselho Federal de Medicina [internet]. Brasília (DF); 2012. [cited on January 13, 2013]. Available on: http://portal.cfm.org.br/index.php?option=com_content&view=article&id=23148%3Amedicos-discutem-r&catid=3%3Aportal&Itemid=1
12.Silva JV. Bioethics: multidimensional view. In: Silva JV da; Simões IAR, organizers. The meanings of good death and dignified death. São Paulo: Iátria; 2010. cap. 13, p. 159-67.
13.Bushatsku T, Sarinho ESC, Lima LS, Faria JH, Baibich-Faria TM, Palliative care in patients without therapeutic possibility: a challenge for the health occupation and caregivers. Rev Bioethikos. 2011;5: 309-16.
14.Menezes MB, Selli L, Alves JS. Dysthanasia: Perception of nursing professionals. Rev Latino-Am de Enfermagem. 2009;17: 443-8.
15.Santos JLD, Bueno SMV. The death and nursing professionals issues. Rev enferm. UERJ. 2010;18: 484-7.