ORIGINAL RESEARCH
Social and professional profile of family healthcare team members
Eliane de Fátima Almeida LimaI; Ana Inês SousaII; Cândida Caniçali PrimoIII; Franciele Marabotti Costa LeiteIV; Maria Helena Nascimento de SouzaV; Ethel Eleonor Nóia MacielVI
I
RN. Master of Nursing. Assistant Professor at Federal University of
Espírito Santo. Brazil. E-mail: elianelima66@gmail.com
II
RN. PhD from the National Public Healthcare School. Associate Professor,
Anna Nery Nursing School, Federal University of Rio de Janeiro. Brazil.
E-mail: anaines@pr5.ufrj.br
III
Nurse. Master of Collective Health. Assistant Professor at Federal
University of Espírito Santo. Brazil. E-mail: candidaprimo@gmail.com
IV
RN. Master of Collective Health. Assistant Professor at Federal University
of Espírito Santo. Brazil. E-mail: emaildafran@ig.com.br
V
RN. PhD in Nursing. Adjunct Professor, Anna Nery Nursing School, Federal
University of Rio de Janeiro. Brazil. E-mail: mhnsouza@yahoo.com.br
VI
RN. PhD in Collective Health. Associate Professor, Federal University of
Espírito Santo. Brazil. E-mail: ethel.maciel@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.9405
ABSTRACT
Objective: to identify the profile of Family Health Strategy personnel in the municipality of Serra, Espirito Santo State. Method: this descriptive, transverse study used a structured form to interview 205 health workers in 2013. Results: most of them, regardless of category, were female and had an employment relationship with the municipal health department. Many physicians and nurses held a specialization diploma, were hired by public competitive process, and had prior experience. Most ancillary staff and community health works resided in the municipality where they worked, and had completed secondary schooling. Most of this category, however, had no prior experience in the field. Conclusion: profiling of health personnel, their qualifications and work process is important to adjusting this model of healthcare and to guaranteeing quality care.
Keywords: Primary health care; family health; human resources; nursing.
INTRODUCTION
Primary health care (PHC) in Brazil defines the family health strategy (FHS) as the structuring model of municipal healthcare systems seeking to rearrange the health care provided by the Unified Health System (SUS, as per its acronym in Portuguese). It offers to their users more access and quality of care, streamlining the use of other levels of care and improving results in healthcare indicators where it is implemented1.
This model has a substitutive character to the traditional servicing practices, for a new working process, having as principle universalization, comprehensiveness, decentralization, and popular participation. In this model, the teams must act with actions aimed at promoting health care, prevention, recovery, rehabilitation, and community health maintenance2.
Professionals must be capable of planning, organizing, developing, and evaluating actions that meet the needs of the community, in coordination with several sectors involved in promoting health care3. In this proposal the professional is accountable for comprehensive and continuous care to all family members of the population, in each one of the phases of their lifespan, not restricted to one of the health problems biologically present, but with the commitment that involves individual actions while they are healthy4.
The success of the implementation of any proposal in the healthcare system depends particularly on the profile of those involved, especially on human resources, since the profile of healthcare professionals must meet the requirements necessary to work with this new healthcare model5.
Therefore, in every government level, there is a growing consensus among SUS managers and workers that qualification, performance, and management of human resources deeply affect the quality of the services provided and the users' level of satisfaction5,6.
It is noteworthy that understanding the professional profile and working conditions of these workers can support working process readjustment programs aimed at improving services for the population and, consequently, guaranteeing quality care that meets their needs, and implementing public health care policies. In this context, the objective of this study was to identify the profile of professionals from the FHS in the city of Serra, Espírito Santo, Brazil.
LITERATURE REVIEW
The first definition of PHC was proposed at the International Conference on Primary Health Care, in Alma-Ata. Since then, primary health care has been increasingly becoming a major forum for discussion in the health care context, whether in the international or national arena. This is happening because it has been pinpointed as an important strategy for reducing inequalities in healthcare services, as well as the first element of a continuous health care process with services included in the community, providing actions for promoting, preventing, and rehabilitating individuals who access these services7.
Currently in Brazil, the main strategy of PHC is the FHS8,9. Serving as the strategy for structuring healthcare municipal systems, the FHS has been attempting to rearrange SUS primary care model, offering to its users more access to services and quality of care, streamlining the use of other levels of care, and improving healthcare indicators wherever they are. The teams must develop actions aimed at promoting, preventing, recovering, rehabilitating, and maintaining health care in the community1.
Investment on primary care policies allowed changing several healthcare indicators, reaching coverage goals, and revising the morbimortality profile of the population. Such a finding shows improvement of the health conditions of the Brazilian population. As a result, in the last few decades this has been demonstrating a significant increase in coverage with positive effects, such as a decrease in child mortality and probably mortality in the remaining age group, besides a reduction in unnecessary hospitalizations10.
However, despite all the investment and improvements made in the healthcare sector, there are some challenges yet to be met for strengthening primary care, including: investment in human resource training; professional qualification with continuously established education policies; fair remuneration; investment in service infrastructure, equipment, and technologies needed for quality care; funding and redistribution of more equitable resources; coalitions; changes in political power; and, particularly, support and popular participation7.
This new working care process model must take a specific form, providing differentiated training, qualification, and profile for FHS professionals, since the emphasis on care is not directed towards technical procedures, but rather on the team/community/family and team/team interrelationship. The working process in the FHS currently requires new skills, competences, and approaches from its professionals in order to overcome difficulties as they carry out their tasks, and benefits the implementation of strategic actions with more impacting effects in their territories11.
METHODOLOGY
This cross-sectional and descriptive study, using a quantitative approach, was carried out in FHS units in the city of Serra, Espírito Santo. The city of Serra is located in the Brazilian southeastern region. It has an area of 553.5 km2 and is considered the largest city in the metropolitan region of Grande Vitória. This region comprises five districts: Serra, Carapina, Nova Almeida, Queimado, and Calogi.
The population of this study was made up of 32 physicians, 32 nurses, 116 community health agents, and 25 nursing aides who worked in the FHS. The study inclusion criteria considered the following conditions: belonging to the same family health unit for more than one year and not being on vacation or on leave during data collection. Data were collected from August to September 2013, when the study was carried out in primary health care units that followed the FHS model. Interviews were conducted applying a structured form, including the following information: age, gender, level of education, area of specialization, service time, type and number of employment bond, length of experience in the FHS, and professional qualification.
The results were presented by means of graphs and tables using Microsoft Office Excel (version 2010). The research proposal was approved by the Research Ethics Committee of Anna Nery School of Nursing, at the Federal University of Rio de Janeiro, under protocol number 315.266.
RESULTS AND DISCUSSION
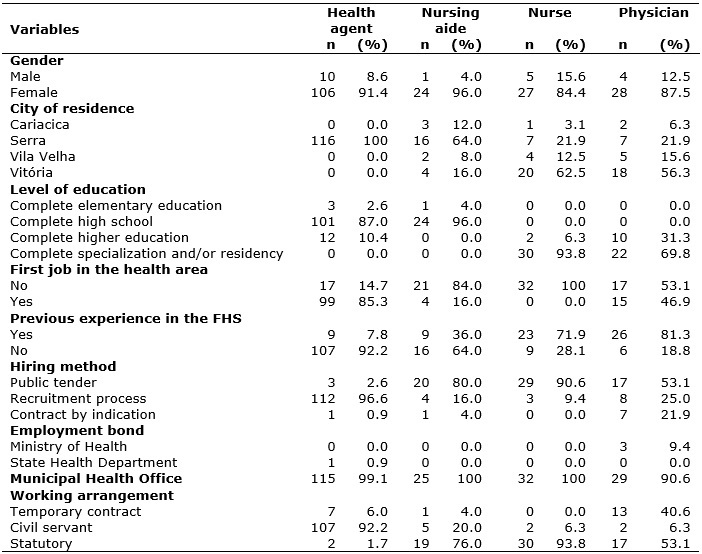
The researchers conducted 205 interviews with FHS professionals. Socio-demographic and professional characteristics of FHS workers from the city of Serra are shown in Table 1.
TABLE 1:
Sociodemographic and professional profile of Family Health Strategy
professionals. Serra-ES, 2013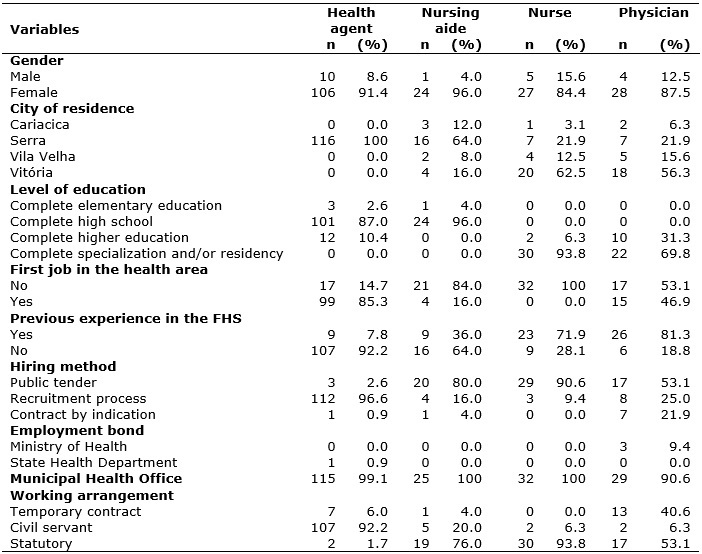
Most community health agents were women (91.4%), with a mean age of 37.4 years, living in the city of Serra (100%), who had finished high school (87%), were hired in the FHS through a recruitment process (96.6%), with this being their first job in the health care area (85.3%) and 92.2% did not have previous experience in the health care sector. They had an employment bond with the Municipal Health Office (99.1%) and their working arrangement was as public service employees (92.2%). See Table 1.
Among nursing aides, women also predominated (96.0%), with a mean age of 43.6, living in the city of Serra (64.0%), having finished high school (96%), and who were hired in the FHS through public tender (80.0%). For 84.0% this was not their first job in the healthcare system, however, 64.0% did not have previous experience. They had an employment bond with the Municipal Health Office (100.0%), and their working arrangement was the statutory regime (76%). See Table 1.
The nurses were predominantly female (84.4%), with a mean age of 41.2 years, living in the city of Vitória (62.5%), having completed a specialization degree and/or an internship program (93.8%). They were hired in the FHS though public tender (90.6%), 71.9% had previously worked in the FHS, and for 100% this was not their first job in the health sector. They had an employment bond with the Municipal Health Office (100%), and their working arrangement was the statutory regime (93.8%), according to Table 1.
The physicians were also predominantly female (87.5%), with a mean age of 38.8 years, living in the city of Vitória (56.3%), having completed a specialization degree and/or an internship program (53.1%). They were hired in the FHS through public tender (53.1%), 81.3% had previous experience, however, for 46.9% it was not their first job in the healthcare system. They had an employment bond with the Municipal Health Office (90.6%), and their working arrangement was the statutory regime (53.1%), but 40.6% held temporary contracts, according to Table 1.
In relation to healthcare workers, regardless of the professional category, the female gender predominated. The feminization found among FHS professionals is consistent with the literature, which reveals a tendency towards feminization of the career in the healthcare sector and, as a consequence, in the family healthcare professional staff12, which can be confirmed in Brazilian studies13,14.
Regarding the age of the professionals, a study conducted in Goiana found that workers had a mean age of 38 years15, and another study also confirmed these results and found a mean age of 34.74 years for nurses and 36.88 for physicians16. On the other hand, the study showed that 62.6% of the professionals were less than 30 years of age13 .
The high prevalence of professionals with a graduate degree revealed a trend towards seeking better qualification enrolling in specialization courses in the healthcare area, which can be confirmed by other studies. For instance, in a study conducted with nurses from the west region of the state of Goiás, 53.1% of the nurses had a specialization degree for working in the FHS, which demonstrates their concern with qualification 15. Furthermore, a study on the FHS, in the state of Paraíba, pointed out that 80% of the nurses had a specialization and 20% held master's degree, and 100% were hired for the job through public tender 17.
Most of the community health agents (56%) completed high school; 22% of them held technical training, all nursing aides had a technical level, 50% of the physicians had a residency, and 99% of the nurses had a specialization18.
A study conducted in Montes Claros, Minas Gerais14, showed that among those with a graduate degree the nursing category represented 51.9% and the medical, 19.0%, with no statistical difference among the groups. Women corresponded to 83.5% of the graduates (p = 0.05), and 47.1% of those with a graduate degree took multiprofessional residency courses in family health care14. Furthermore, studies carried out with physicians and nurses of the FHS in the city of São Paulo found that 43% of the nurses with a specialization and that public health care area was predominant; however, 73% of the physicians did not hold medical residency or specialization16.
Another study confirmed the profile found in the results, since physicians and nurses were mostly women (65.9%), with a mean age of 34.7 years, all having a graduate degree in family health care with a mean of 7.5 years since they were graduated19.
As for working conditions, this research found that most of the workers, regardless of the professional category, were employed by the municipality and hired through a recruitment process or public tender. Similarly, another study found that 100% of the physicians and nurses were admitted through public tender16.
A study conducted in Londrina showed that the service contract for the FHS professionals in the city was carried out through public-sector or statutory employment regime. More than half of the nurses (57.3%) worked under public-sector employment regime and 50% of the physicians had public-sector employment, and the other half were integrated through a statutory regime4.
Another study brought to light interesting data on how professionals were hired in the FHS, in which great part of the community health agents and nursing aides were hired through public tender, however, all nurses and most physicians were hired by other means, such as an invitation or simply occupying the position available18.
In a study conducted with physicians and nurses in Mato Grosso, 90.5% of the professionals were linked to the municipalities; however, 65.2% held precarious employment arrangements, and this was one of the factors that was making the implementation of the FHS difficult, causing discontentment among professionals who preferred a stable employment bond20.
As for the length of experience in primary healthcare units, approximately 60% of the physicians (mean time of 9.1 years) and only 37% of the nurses (mean time of 5.8 years) held more than five years. The vast majority of the nurses (80.9%) and more than half of the physicians (56.1%) held more than two years working with family health, which makes a mean of 2.4 and 2.0 years, respectively4.
A study in the city of São Paulo found that 66% of the nurses and 69% of the physicians were working in the FHS for less than two years and 34% and 54% of the nurses and physicians, respectively, had another employment bond 16.
Regarding length of service, the community health agents had been working for a mean of 6.19 years in the FHS, nursing aides for 6 years, nurses for 5.65 years, and physicians for 3.87 years.
As for monthly wage, 47.41% of the community health agents received between BRL 840 and BRL 940, whereas 84% of the nursing aides earned between BRL 1,300 and less than BRL 2,000, and 68.8% of professionals with higher education (physicians and nurses) received salaries higher than BRL 6,000.
It is important to emphasize that the gross income disclosed by 46.3% of the physicians varied from 25 to 35 minimum wages, whereas the gross income disclosed by 78.4% of the nurses varied between 5 and 15 minimum wages monthly, revealing a significant difference in income between both professional categories20.
Evaluating satisfaction with their remuneration, the study found that it was considered reasonable for physicians (66.7%), nurses (66.7%), and community health agents (39%), but low for the vast majority of nursing aides (66.7%)14.
CONCLUSION
This study described the profile of FHS team professionals from the city of Serra, Espírito Santo. The results certainly contribute to shed a light on professionals with secondary and higher education who provide service and assist the population, especially when there is a lack of studies on the subject, as in the case of community health agents.
The study highlighted that health professionals, regardless their category, are mostly women, and have an employment bond with the Municipal Health Office.
The results revealed that most physicians and nurses live in the city of Vitória, have full specialization or residency, were admitted to the FHS through a public tender, hold previous experience in FHS, and an employment bond under statutory regime. In relation to nursing aides and community agents, the vast majority lives in the city of Serra and completed high school. Among community health agents, most were hired by the FHS through a recruitment process, are public employees, hold their first job in the healthcare area, and have no previous experience in the FHS. On the other hand, nursing aides were hired by the FHS through a public tender, are under statutory regime, and this was not the first job in the healthcare system. Most do not have previous experience in the FHS.
It is noteworthy that the professional profile must be focused on forms of action, capabilities, initiative and skills, especially planning the actions in programs to be developed and in their respective implementation and evaluation.
REFERENCES
1.Ministério da Saúde (Br). Secretaria de Assistência a Saúde. Saúde da Família: Uma estratégia para a reorientação do modelo assistencial. Brasília (DF): Ministério da Saúde; 1994.
2.Ministérios da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Guia prático do Programa de Saúde da Família. Brasília (DF): Ministério da Saúde; 2001.
3.Organização Pan-Americana da Saúde. Avaliação de tendências e prioridades sobre recursos humanos de saúde. Brasília (DF): Organização Pan-Americana da Saúde; 2002.
4.Ferrari RAP, Thomson Z, Melchior R. Estratégia da saúde da família: perfil dos médicos e enfermeiros, Londrina, Paraná. Ciências Biológicas e da Saúde. 2005;26:101-8.
5.Cotta RMM, Pereira RJ, Maia TM, Marques ES, Franceschini SCC. Aprehensión y conocimiento de las directrices del Sistema Único de Salud (SUS): un reto en la consolidación de la política de salud brasileña. Rev. Agathos – Atención Sociosanitaria y Bienestar. 2004; 3:16-23.
6.Araújo MBS, Rocha PM. Trabalho em equipe: um desafio para a consolidação da estratégia de saúde da família. Ciênc. saúde coletiva. 2007;12:455-464.
7.Ministérios da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. A melhoria contínua da qualidade na atenção primária à saúde: conceitos, métodos e diretrizes. Brasília (DF): Ministério da Saúde; 2010.
8.Goulart FAA. Experiências em Saúde da família: cada caso é um caso? (Tese Doutorado). Rio de Janeiro: Escola Nacional de Saúde Pública/Fiocruz; 2002.
9.Ministérios da Saúde (Br). Conselho Nacional de Secretários de Saúde. Sistema Único de Saúde Conselho Nacional de Secretários de Saúde. Brasília (DF): CONASS; 2011.
10.Victora CG. Barreto ML, Leal MC, Monteiro CA, Schmidt MI, Paim J, et al. Condições de saúde e inovações nas políticas de saúde no Brasil: o caminho a percorrer. Saúde no Brasil. 2011;6: 90-103.
11.Oliveira MMC. Presença e extensão dos atributos da Atenção Primária à Saúde entre os serviços de Atenção Primária em Porto Alegre: uma análise agregada. (Dissertação Mestrado). Porto Alegre: Universidade Federal do Rio Grande do Sul. Faculdade de Medicina; 2007.
12.Pinto ESG, Menezes RMP, Villa TCS. Situação de trabalho dos profissionais da Estratégia Saúde da Família em Ceará-Mirim. Rev. esc. enferm. USP [online]. 2010 [cited on 2015 Mar 23]; 44:657-64. Available from: http://www.scielo.br/pdf/reeusp/v44n3/15.pdf
13.Oliveira WMA, Bezerra ALQ. Autoavaliação da Estratégia Saúde da Família por Enfermeiros. Rev enferm UERJ. 2011; 19:20-5.
14.Costa SM, Prado MCM, Andrade TN, Araújo EPP, Silva Junior EW, Gomes Filho ZC, et al. Perfil do Profissional de Nível Superior nas Equipes da Estratégia Saúde da Família em Montes Claros, Minas Gerais, Brasil. Rev Bras Med Fam Comunidade [online]. 2015 [cited on 2013 Oct 15]; 8: 90-6, 2013. Available from: http://www.rbmfc.org.br/rbmfc/article/view/530
15.Santana FR, Santana FR, Anjos GV, Campos TV, Lima PCT, Lopes MM, et al. Ações de saúde na estratégia saúde da família no município goiano na perspectiva da integralidade. Rev. Eletr. Enf. [Internet]. 2013 [cited on 2015 Aug 10]; 15: 422-9. Available from: http://www.fen.ufg.br/revista/v15/n2/pdf/v15n2a15.pdf
16.Lopes EZ, Bousquat AEM. Fixação de enfermeiras e médicos na Estratégia Saúde da Família, município de Praia Grande, São Paulo, Brasil. Rev bras med fam comunidade. 2011;6: 118-24.
17.Rocha ACD, Sousa CPC, Queiroz D, Pedraza DF Atenção básica à saúde: avaliação de estrutura e processo. RAS. 2012;14:71-9.
18.Cotta RMM, Schott M, Azeredo CM, Franceschini SCC, Priore SE, Dias G. Organização do Trabalho e Perfil dos Profissionais do Programa Saúde da Família: Um desafio na reestruturação da Atenção Básica em Saúde. Epidemiologia e Serviços de Saúde. 2006; 15: 7-18.
19.Maia LDG, Cana JPRC, Lopes CFMM, Rodrigues-Neto JF. Utilização do Sistema de Informação da Atenção Básica (SIAB) para o Planejamento das Ações pelas Equipes da Estratégia de Saúde da Família do Município de Montes Claros (MG). Revista Baiana de Saúde Publica. 2010; 34: 359-70.
20.Canesqui AM, Spinelli MAS. Saúde da família no Estado de Mato Grosso, Brasil: perfis e julgamentos dos médicos e enfermeiros. Cad. Saúde Pública. 2006; 22: 1881-92.