ORIGINAL RESEARCH
Characteristics of benzodiazepine use and dependence: primary health care
Vanessa Pereira SilvaI; Nadja Cristiane Lappann Botti II; Valéria Conceição de OliveiraIII; Eliete Albano
de Azevedo GuimarãesIV
INurse. Professor at the University of the State of Minas Gerais.
Divinópolis, Minas Gerais, Brazil. Email:
vanessanurse22@yahoo.com.br
IIPhD in nursing. Professor at the Federal University of São João Del Rei -
Dona Lindu Campus. Divinópolis, Minas Gerais, Brazil. E-mail:
nadjaclb@terra.com.br
IIIPhD in nursing. Professor at the Federal University of São João Del Rei -
Dona Lindu Campus. Divinópolis, Minas Gerais, Brazil. Email: valeria.oli.enf@gmail.com
IV.
PhD in health sciences. Professor at the Federal University of São João Del
Rei - Dona Lindu Campus. Divinópolis, Minas Gerais, Brazil. Email: elietealbano@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.8783
ABSTRACT
Objective:
to analyze benzodiazepine users' socio-demographic characteristics, use
history and dependence. Method: in this cross-sectional
study of an intentional sample of 219 benzodiazepine users enrolled with
four family health teams in the western Minas Gerais State, data was
collected between January and May 2013 by applying an adapted
questionnaire. Epidata 3.1 and EPINFO 6.04 software were used for data
tabulation and descriptive analysis. Results: most of the
benzodiazepine users were female, and 53 to 60 years old. Clonazepam was
the benzodiazepine most commonly used, and 181 individuals (82.6%) were
found to be chemically dependent on benzodiazepines. Conclusion: factors such as the positive image, low cost
and swapping of benzodiazepines, medicalization of personal, social, family
and professional problems, and treatment inadequacies contributed to
benzodiazepine dependence.
Keywords: Benzodiazepines; primary care; substance dependence; mental health.
INTRODUCTION
Primary healthcare (PHC) aims to enable the first access of people to the
health system, including those who demand attention in mental health1. This care is facilitated by the possibility of access of
users and vice versa, since family health (FH) teams work with a defined
area and rely on the work of community health agents. Due to these
characteristics, it is part of the daily life of FH professionals to handle
all the time users in mental distress situation, as well as with other
elements of their contexts of life2.
People suffering with mental conditions in general present a significant
reduction in quality of life, with lower productivity, higher morbidity and
mortality, and higher rates of comorbidity. Parts of these enormous direct
and indirect social costs can be aggravated because this is a group with
undiagnosed, understated and often inappropriately handled disorders3.
Among the psychiatric disorders that affect the population currently, great
mood and anxiety disorders are the most common and are identified more
frequently in units of AP. For the treatment of mood and anxiety disorders
it is common in units of the family health strategy (FHS) prescribing
benzodiazepines (BZD), which are among the most prescribed psychotropics,
characterized as anxiolytics, sedatives, hypnotics, anticonvulsants,
anesthetics and muscle relaxant and supporting anesthetics3.
When correctly indicated, BZD shows useful for presenting fast onset of
action, few side effects and good safety margin4.
However, the big problem of the misuse and indiscriminate use of BZD arises
from the time there is the medicalization of life or personal, socio-family
and professional problems; the continuous use of these medications can
cause the phenomenon of tolerance, being increasingly higher doses
necessary to maintain the desired therapeutic effects5.
Thus, chemical dependence becomes a worrying and common phenomenon in
primary healthcare units (UAPS). And, often, dependent users are reluctant
to withdraw gradually the medication, stating changes in the pattern of
sleep and rest such as insomnia and anxiety6.7. Based on the
above considerations, this study sought to characterize sociodemographic
aspects, history of use and dependency of benzodiazepines among users in
primary healthcare.
LITERATURE REVIEW
BDZs are drugs with anxiolytic activity that began to be used in the 60's.
Chlordiazepoxide was the first BDZ released on the market (1960), 5 years
after the discovery of its anxiolytic, hypnotics and myorelaxant effects.
Because they present high therapeutic efficacy, BDZs presented low
intoxication risk and dependence, factors that led to the rapid acceptance
of medical professionals to its prescription7.
However, later identified the first cases of abuse, in addition to
development of tolerance, dependence and withdrawal syndrome by chronic
users of BDZ8.9.
To give theoretical support to the study, there were used criteria
established by the Diagnostic and Statistical Manual of Mental Disorders
(DSM IV) which is a guideline for mental health professionals, with
definitions of different categories of mental disorders and criteria to
diagnose them, according to the American Association of Psychiatry ( American Psychiatric Association -APA)10.
Thus, it was set the term of substance dependence such as the
presence of a cluster of cognitive, behavioral and physiological symptoms
indicating that an individual continues to use a substance even if this
causes significant problems. Which leads to a pattern of auto repeated
administration that results in tolerance, withdrawal and compulsive use of
the substance.
Tolerance and withdrawal symptoms may be associated with a greater risk of
immediate clinical problems and with higher relapse rate11. The
definition of specifiers according
to DSM IV were also used for physiological dependence of substance which is
when dependence is accompanied by evidence of tolerance and withdrawal and
without physiological dependence which is when there is no evidence of
tolerance or withdrawal, however there are compulsive symptoms.
METHODOLOGY
Descriptive and cross-sectional study performed in a medium-sized
municipality of the Western region of the State of Minas Gerais. The
intentional sample was composed of BZD users of both genders, aged over 18
years old enrolled in the municipal pharmacy of four reference FH teams of
Western Minas Gerais, who received drugs in the last 12 months, according
to what regulates the Ordinance n° 34412. The registered
population of the four FHS makes the total of 10,050 inhabitants.
The list of BZD medicines dispensed by the pharmacy, in the APS of that
municipality, includes Diazepam 10mg, Clonazepam 2mg and Clonazepam
2.5mg/mL Alprazolam 0.5 mg and Nitrazepam 5.0mg dismissed upon notification
of prescription B, in accordance with the legislation that approves the
technical regulation on substances and medicinal products subject to
special control12.
There are, registered in the pharmacy of reference of the four municipal
units of FH, 295 users of BDZ. Out of these, 76 users were excluded from
the survey because they do not wish to participate, or due to death or
change of address. Therefore, the sample comprised 219 users who have
agreed to participate in the research.
The data were collected through the application of an adapted questionnaire6 plus issues related to diagnostic criteria for dependence on
substances10. The questionnaire was applied by home
visit by the researcher in charge of the project, from January to May,
2013.
The data were entered into EPIDATA 3.01 program and analyzed in theStatístical Pacckage for the Social Sciences (SPSS ®) 17.0 software. Descriptive analysis of the data, the issues have been
categorized as demographic profile, profile of health condition and
characteristics of chemical dependence.
In this study, the dependence was set to a default of wrong use of Adaptive
benzodiazepines, manifested by three or more criteria, occurred in the last
12 months.
In addition to the tolerance criteria (criterion 1) and abstinence
(criterion 2) for identification of physiological dependence, were
the criteria of compulsive symptoms to chemical dependence without
physiological dependence that are: Presence of frequent consumption
and in greater quantity for a longer period than intended (criterion 3).
Persistent desire or unsuccessful efforts to reduce or stop using the
medication (criterion 4). If too much time is spent to obtain BZD
(criterion 5). If important activities are abandoned or reduced due to the
use of BZD (criterion 6) and if there are reports of any health problems
due to the use of BZD (criterion 7).
Given the resolution No. 466/2012 of the National Council on ethics in
research with Human Beings-CONEP, which deals with the rules on research
involving human beings, was elaborated an informed consent form containing
the objectives and purpose of the research, the voluntary participation and
maintaining the anonymity of the subjects. The project was approved by the
Municipal Health Secretariat and by the Committee of ethics in research
(CEP) at the Federal University of São João Del Rei (UFSJ), through CAE
09751212.5.0000.5545.
RESULTS AND DISCUSSION
Characterization of the Subjects
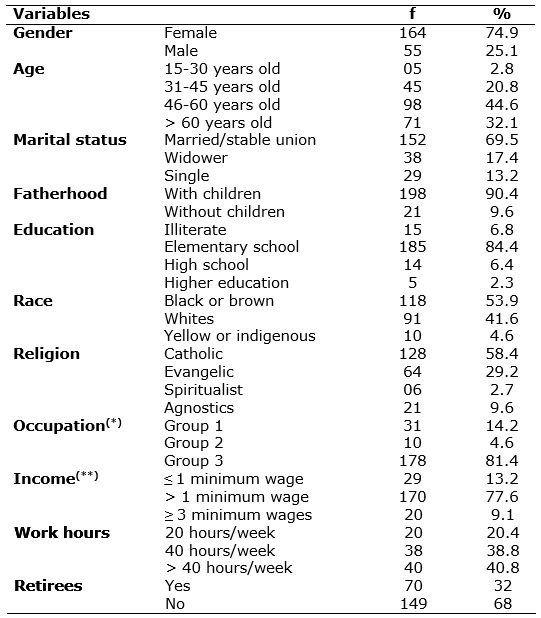
Among the 219 subjects included in the survey, it was found that 98 (44.6%)
individuals are aged 46 to 60 years old and 71 (32.1%) in the group above
60 years old. The average age was 53.6 ± 12.2 years old. When it comes to
gender, 164 individuals (74.9%) were female and 55 (25.1%) male. In
examining the marital status, it was observed that more than half of
respondents were married or were in a stable relationship 152 (69.5%). See
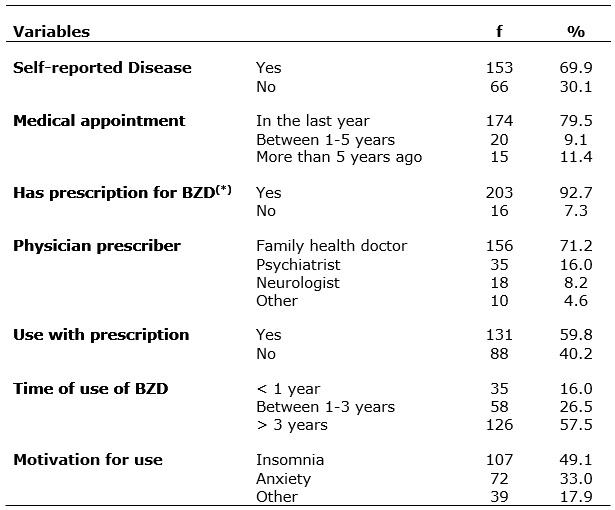
Table 1
TABLE 1: Socio-demographic characteristics of the registered users in the municipal pharmacy Municipality of West region of Minas Gerais, 2013. (N=219)
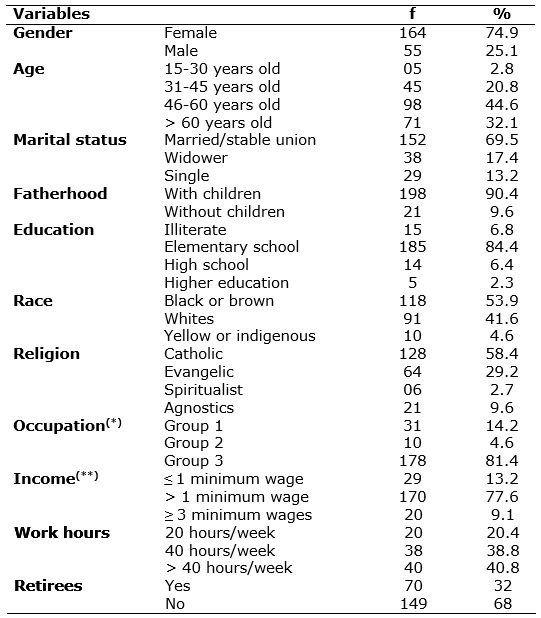
(*) Group 1: Workers in service areas, trade vendors in shops and markets. Group 2: Agricultural workers, forestry, hunting and fishing. Group 3: Workers in the production of industrial goods and services
(**) Minimum wage value: R$ 678.00 Reais.
Most of them 198 (90.4%) had children, and 144 (70.9%) reported having
three or more children. There has been a low level of schooling of the BZD
users, and only 185 (84.4%) have elementary school; and 118 (53.9%)
declared to be black or brown. Catholic religion was prevalent 128 (58.4%).
As for household income, stood out 170 (77.6%) who declared to receive one
to two minimum wages and 29 (13.2%) with income of less than the minimum
wage, as shown in Table 1.
The results showed that most of the BZD users are female, between the ages
of 50 to 69 years, with low education and income, corroborating other
studies13-17. On APS using BZD presents a dysfunctional pattern
repetitive, in which women-housewives, married, with three children or
more, lower educational level and therefore with less information, less
income, role of caregiver and family conflicts-are subject to greater use
of medicines causing dependence, potentially with organic and mental side
effects is important.
The largest use of BZD was reported by women who reported not be acting in
the job market. Previous study identified similar results, users
who do not have a job showed higher prevalence of mental suffering 15. However, another study points out that professionals who
have a job, who are exposed to factors such as stress in the occupational
environment, poor remuneration, lack of motivation and long journeys to
work, also use BZD18.
Studies claim that beyond gender, cultural and social issues, the
representative image of women in advertising of pharmaceutical industry,
ends up being decisive and interferes with the clinical approach to making
medical professionals to become more susceptible to the diagnosis of
diseases such as anxiety and depression in female gender13,19-22
. Besides, there are studies with women in the menopausal period, which
estimates a significant prevalence of depression and anxiety in patients;
36.8 and 53.7%, respectively, since some of the signs and symptoms of this
phase such as insomnia, irritability are being treated with BZD 23-25.
Health conditions of the subjects
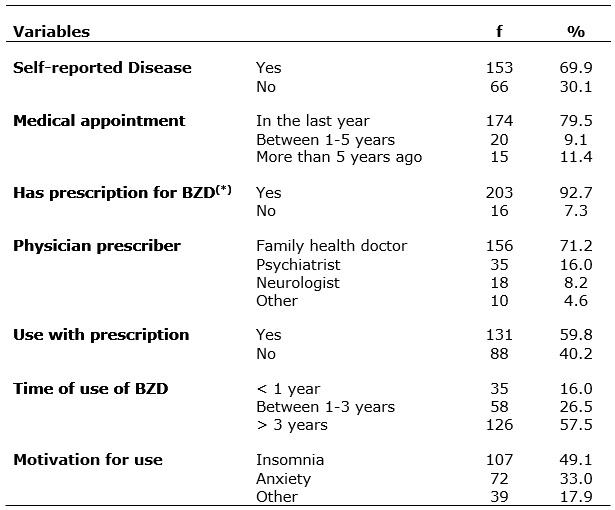
On the characterization of health conditions, it was observed that 153
(69.9%) subjects reported having disease. Among the diseases mentioned we
highlight hypertension 68 (44.4%), 32 (20.5%), diabetes, hypertension and
diabetes 25 (16.3%) and other diseases such as depression, heart diseases
and musculoskeletal disorders - 28 (18.3%). It was also found that 79.5%
respondents had a medical appointment last year; 92.7% reported owning the
prescription with prescribing BZD, being the general practitioner/FH doctor
the professional who prescribed the most (71.2% of prescriptions).
About the use of the BZD, 131 individuals (59.8%) reported using according
to the prescription. The time of prolonged use has been observed since, 126
(57.5%) subjects reported being using BZD for over three years. The main
reason to use this study was insomnia reported by 107 individuals (49.1%),
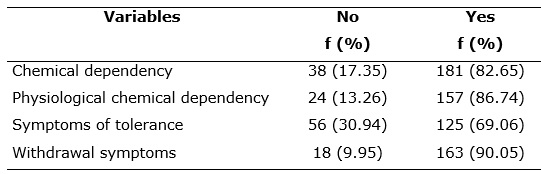
followed due to anxiety with 72 individuals (33.0%) as shown in Table 2.
TABLE 2: Characteristics of health conditions of registered users at the municipal pharmacy. Municipality of West region of Minas Gerais, 2013 (N = 219)
(*) BZD = benzodiazepine
Several studies indicate the Diazepam as the most prescribed
psych medicines, however, in this research, the most widely used BZD was
Clonazepam, followed by users of Diazepam17-19. A research
carried out in Brazil has shown that, in 2004, Clonazepam was the sixth
among the 10 best-selling drugs, taking the second position in 2008 20. Bromazepam, Nitrazepam and Alprazolam are also used by
users, however, outnumbered. There was no report of using Midazolam,
Lorazepam and Flurazepam.
Among the factors that comprise the misuse of BZD, prolonged treatment as
one of the most often reported, corroborating other authors 13, 15, 17. The daily dose and the time of use of the
BZD are factors for determining a dependence framework. The use of up to 3
months presents a low risk. Between 3 and 12 months of use, the risk
increases between 10% to 15%, and for more than 12 months the risk is 25%
to 40%20.
The results of this study showed that most users used the medication for
more than three years and continuously, with reports of some customers who
have already used it for over 30 years.
The motivation to use was reported mainly for insomnia and anxiety problems
(for example, symptoms of panic, stressful situations, such as family
squabbles, work-related issues), or escape from the family or personal
problems; there have been also situations involving grief or pain. Many
users have reported the use of BZD mostly for depression treatment and not
as an adjuvant, which demonstrates ignorance on the part of the clients in
relation to the consumption of BZD and the professionals about the
prescriptions26.
The use of BZD on clients that self-reported morbidities was described in
other studies4, 6, 24, 27-29, and brings concerns about the
possibility of drug interactions. Especially among hypertensive and
elderly, for damages caused using central depressor effect BZD and
orthostatic hypotension common to antihypertensive drugs, increasing the
risk of falls among users particularly among elderly18.29. In
addition, there is a study15 that shows that BZDs are being used
as an important feature in the treatment of hypertension, aiming to control
a user's emotional state, thus avoiding peaks of elevation of blood
pressure.
The use of BZD has several factors as influence, such as the positive image
of anxiolytic, going through the fact that it is easy to the doctors to
prescribe them, self-medication, until the popularity among peers, through
the loan and/or indication among family or friends. In this study, it was
observed that most of the BZD prescriptions was performed by general
practitioners/FH doctors, which confirms other studies15, 26-31.
This fact may be related to the search; however, studies show that medical
specialties as Neurology and Psychiatry restrict and prescribe less BZD for
better know its effects30-33.
Prescription of BZD by general practitioners/FH doctors can be related to
their unpreparedness for prescribing BZD, ignorance of the percentage of
dependents of BZD, the gravity of this use and side effects of drugs. Other
factors may also be involved such as: medical consultation only to get one
more BZD prescription without specialized monitoring, lack of time for a
detailed guidance or indication of other therapeutic practices 30-32.
On the high consumption of BZD between users, appointments of doctors who
are not experts, there is a study that questions that fact and points out
that it would be ideal if the prescription was given by a neurologist or
psychiatrist, for the absence of these professionals may compromise the
quality of prescription33. In addition, the mentioned study
claims that the prescription by other professionals contributes to a
possible mistake in the diagnosis and unnecessary use of central action
medications, and favors the irrational use and unmonitored use of
antidepressant drugs and psychotropic substances in general, which can lead
to Iatrogenesis and even death.
However, this issue is contrary to the guidelines established for the APS
that prioritizes prevention and promotion at primary level, as well as the
interdisciplinary team work, based on a network of psychosocial care,
focusing on individual/family and their needs and that interacts with other
sectors of society.
Study shows that users of BZD go more to FH units for medical appointments,
once the BZD prescription is generally standardized and in general it is
good for 2 months12,31. However, it should be noted that many
users attend the medical consultation only for revalidation or to obtain a
new prescription, primary source of BZD supply by individuals who use
abusively this type of drug.
Use of BZD and dependence
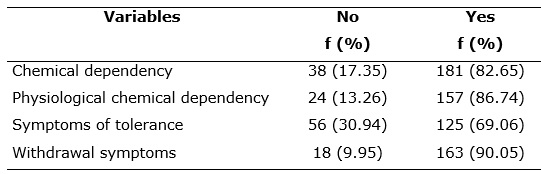
In the analysis of consumption of BZD by registered users in the pharmacy,
according to diagnostic criteria for chemical dependence, 181 (82.65%)
subjects are considered addicts. Of these, 157 (86.7%) have physiological
chemical dependence. It was also verified that among the chemical
dependents, 125 (69.0%) presented signs of tolerance (criterion 1) and 163
(90.0%) withdrawal symptoms (criterion 2).
In examining the criteria for compulsive symptoms, it was found that the
criterion 3 affects 152 (69.4%), criterion 4 was informed by 145 (66.2%)
and 120 (54.8%) reported that they do not have difficulty in getting the
medication (criterion 5). About criterion 6, 160 (73.1%) reported not
having ceased to carry out important activities and 198 (90.4%) stated that
they had no problem when using BZD (criterion 7) see table 3.
TABLE 3: The use of benzodiazepines according to diagnostic criteria for chemical dependency, according to the DSM IV. Minas Gerais - 2013. (N = 219)
In this study, it was found that most users failed in suspending the use of
the BZD, what characterizes this medication dependence. Therefore, the
suspension of treatment could lead to the installation of the undesirable
symptoms of withdrawal syndrome or another acute manifestation of the
disease.
The failure of the attempt of stopping the use of BZD can be related to
difficulty in distinguishing symptoms of withdrawal of the reappearance of
symptoms from anxiety10.
When asked whether the use of BZD caused or worsened health problems, most
denied such a result. However, the few users who reported having any side
effects when using BZD reported the feeling of dry mouth, which led
to high amount of water intake, feel dizzy, headache and drowsiness. Such
symptoms observed match what is expected and notified in the package
inserts of pharmacologically active drugs.
CONCLUSION
This study presented the sociodemographic aspects, history of use and
dependency of benzodiazepines among users in primary healthcare. The
results revealed that the profile of users of BZD, present women aged
between 50 and 69 years, vulnerable to addiction, with low education and
income, without employment links, with a history of chronic diseases. In
addition, he noted that these drug dependent women are being medicated with
BZD for the treatment of menopausal symptoms, depression and blood pressure
control.
Saying that the prescription should be made by psychiatrists or
neurologists is contradictory to proposal of the FHS which should solve the
problems in most cases of mild mental disorders. Discussion of cases are
needed, considering risk and vulnerability. In addition, the support of
Family Health Support Center, consisting of a multidisciplinary team, needs
to promote work processes in conjunction with APS professionals, thereby
enhancing the completeness of care through expanded clinic, and assisting
in strengthening the capacity for analysis of health problems and health
needs for appropriate interventions.
The limitation of this study refers to the location where the research was
conducted, family health teams located in neighborhoods considered
economically or socially disadvantaged, which may have contributed to the
characteristics, i.e. the profile of the sample studied. The contribution
lies in the field of public health policies, because it points to necessary
changes in prescribing, dispensing and use of benzodiazepines in primary
health care.
REFERENCES
1. Ministry of Health (Brazil). Secretariat for healthcare. Department of
basic attention. Mental health. (Basic attention notebooks, No 34).
Brasília (DF): Ministry of Health; 2013.
2.Ramos LS, Beck CLC, Freitas NQ, Dissen CM, Fernandes MNS, Colomé ICS,
Mental health Commission; strategies in the search for spaces in the basic
attention. Nurs. Journ. UERJ. 2013; 21 (esp. 1): 581-6.
3.Forsan MA. The indiscriminate use of benzodiazepines: a critical analysis
of the practices of prescription, dispensation and prolonged use. Federal
University of Minas Gerais. Medical School. Center for education on public
health. General fields, monograph.
4.Naldo DCC, Filho SB, Lopes LC, Lopes FC, Bergamasch CC, Del fiol FS.
Prescription of benzodiazepines for adults and seniors of a mental health
clinic. Scien. Collective health, 2016;21(4).1267-76.
5.Ferrari CKB, Brito LF, Oliveira, CC, Moraes EV, Toledo OR. David FL. Gaps
in prescription and dispensation of psychotropic drugs: a public health
problem. Basic Pharm. Scien. Journal 2013; vol 34(1):109-16.
6.Santos RC. Profile of users of psychoactive drugs served by the family
health strategy of the urban area of the municipality of Presidente
Juscelino [monograph]. Belo Horizonte (MG): Federal University of Minas
Gerais; 2009.
7.Santos HC, Ribeiro RR, Ferrarini M, Fernandes JPS. Possible drug
interactions with psychotropic drugs found in patients from the East zone
of São Paulo. Basic Pharmacy Applied Science Journal 2009; 30 (3):285-9.
8.O'Brien CP. Benzodiazepine Use, abuse, and dependence. Journal of
Clinical Psychiatry. 2005; 66 (suppl2): 28-33.
9.Silva JA. History of benzodiazepines. In: Bernik MA, editor.
Benzodiazepines, four decades of experience. São Paulo:1999. p. 15-28
10. The American Psychological Association. Diagnostic and Statistical
Manual of mental disorders DSM-IV-TRTM. Artmed. 2000.
11. Secretary of State for Health (MG). Guideline on Mental Healthcare.
Marta Elizabeth de Souza. Belo Horizonte (MG): SES; 2006.
12. Ministry of Health (Brazil). The national health surveillance agency.
Ordinance No. 344, of May 12, 1998. Approving the technical regulation on
substances and medicinal products subject to special control. Brazilian
Official Gazette, Brasília, December 31, 1998. [quoted in Dec 2012]. 15].
Available at: http://www.anvisa.gov.br/legis/portarias/344_98.htm.
13.Souza ARL, Opaleye ES, Noto AR. Contexts and patterns of misuse of
benzodiazepines among women. Scienc. public health [serial on the
Internet]. 2013 [quoted in Jan, 26, 2016]; 18 (4): 1131-40.
14.Alvarenga JM, Filho AIL, Firmo JOA, Lima-Costa MF, Uchoa, E. Prevalence
and sociodemographic characteristics associated with benzodiazepines use
among community dwelling older adults: the Bambuí Health and Aging Study
(BHAS). Brazilian Journal for psychiatry 2008; 30(1).
15.Firmino KF, Abreu MH, Perini E, Magalhães SM. Factors associated with
benzodiazepine prescription by local health services in Coronel Fabriciano,
Minas Gerais State, Brazil. Cad Saude Publica 2011; 27(6):1223-32.
16.Estrela KSR, Loyola CMD. Administration of medication to use when needed
and the care of psychiatric nursing. Brazilian Journal for nurses 2014; 67
(4): 563-7.
17.PCPT Filho, Almeida AGP, Pinheiro MLP. Self-medication in elderly: a
public health problem. Nursing Journal UERJ.2013;21(2).197-201.
18.Mendonça RT, Carvalho ACD, Vieira EM, Adorno CF. Medicalization of
elderly women and interaction with consumption of tranquilizers. Health and
Society. 2008; 17(2):95-106.
19.Nordon DG, Akamine K, Novo NF, Hübner C von K. features of use of
benzodiazepines for women who sought treatment in primary care. Rio Gde do
Sul Psychiat. Journal. 2009; 31 (3):152-8.
20.Monteiro VFF. Profile of anxiolytic drugs distributed in the municipal
pharmacy of the municipality of Campos dos Goytacazes – RJ in the year
2008. [monograph]. Campos of Goytacazes (RJ): Campos Medical School; 2008.
21.Graeff FG; Guimarães FS. Fundamentals of psychopharmacology. São Paulo:
Editora Atheneu; 1999.
22.Mendonça RT, Carvalho ACDd, Vieira EM, Adorno RdCF. Medicalization of
elderly women and interaction with consumption of tranquilizers. Health and
Society. 2008; 17(2):95-106.
23.Polisseni AF, Araújo DAC, Polisseni FM, Mourão CA, Polisseni J,
Fernandes ES Depression and anxiety in menopausal women: associated
factors. Braz Ginecol Obstet 31 (1): 28-34.
24.Fang SY, Chen CY, Chang IS, Wu ECH, Chang CM, Lin KM. Predictors of the
incidence and discontinuation of long-term use of benzodiazepines: a
population-based study. Drug Alcohol Depend. 2009; 104(1):140-6.
25.Hermosa AB, Mejía RC. Memopausia y estereotipos de género: importância
del abordaje desde la educación para la salud. Nursing Journal UFSM 2014;
22 (2):182-6.
26.Nordon DG, Hubner CK. Prescription of benzodiazepines by general
practitioners. Diang Treatment 2009; 14 (2):66-9.
27.Facury APM. Mental health in the family health strategy Dr. Roberto
Andrés: Entre Rios de Minas. Belo Horizonte(MG): Editora UFMG;2010.
28.Santos HC, Ribeiro RR, Ferrarini M, Fernandes JPS. Possible drug
interactions with psychotropic drugs found in patients from the East zone
of São Paulo. Basic Pharmacy Applied Science Journal 2009; 30 (3):285-9.
29.Ramos LR, Tavares NUL, Bertoldi AD, Farias MR, Oliveira MA, Luiza VL,
Pizzol TDs, Arrais PSD, Mengue SS. Polypharmacy and polimorbity in elderly
in Brazil: a challenge to public health. Public Health Journal; 2016.
50(Suppl.2).
30.Orlandi P, Noto AR. Misuse of benzodiazepines: a study with key
informants in the city of São Paulo. Lat. Am. Journal for Nurses. 2005;
13:896-902.
31.Auchewski L, Andreatini R, GJF, Lacerda, RB. Evaluation of the medical
advice about side effects of benzodiazepines. Brazilian Psychiatry Journal
26(1): 24-31.
32.Anthierens S, Pasteels I, Habraken H, Steinberg P, Declercq T,
Christiaens T. Barriers to nonpharmacologic treatments for stress, anxiety,
and insomnia: family physicians' attitudes toward benzodiazepine
prescribing. Can Fam Physician. 2010; 56 (11):398-406.
33.Ferrari CKB, Brito LF, Oliveira CC, Moraes, EV, Toledo OR, David FL,
Gaps in prescription and dispensing of psychotropic drugs: a public health
problem. Basic Pharm. Scien. Journal 2013; 34 (1): 109-16.