Note: Minimum wage at the time of research R$ 622.00 ($ 2.10).
ORIGINAL RESEARCH
Epidemiological profile of children with cerebral palsy receiving care at outpatient clinics
Viviane Mamede Vasconcelos CavalcanteI, Mariana Cavalcante MartinsII, Mônica Oliveira Batista OriáIII, Lorena Barbosa XimenesIV, Mirna Albuquerque Frota V, Zuila Maria Figueirêdo CarvalhoVI
I
Nurse. Adjunct Professor, Federal University of Ceará. Brazil. E-mail: vivienfermagem@hotmail.com
II
Nurse. Adjunct Professor, Federal University of Ceará. Brazil. E-mail:
marianaenfermagem@hotmail.com
III
Nurse. Associate Professor Federal University of Ceará. Brazil. E-mail: monica.oria@ufc.br
IV
Nurse. Associate Professor IV. Federal University of Ceara. Brazil. E-mail: lorena@ufc.br
V
Nurse. Coordinator of the Graduate Program in Collective Health, University
of Fortaleza. Brazil. E-mail: mirnafrota@unifor.br
VI
Nurse. Full Professor, Federal University of Ceará. Brazil. E-mail: zmfca@fortalnet.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.8780
ABSTRACT
Objective: to describe the profile of parents and children with cerebral palsy receiving care at outpatient clinics in Fortaleza, Ceará. Method: in this quantitative study, a questionnaire on socio-economic, demographic and clinical data of children with CP was applied to 122 parents, from October 2012 to January 2013. Exploratory data analysis was performed using SPSS version 20.0. Results: it was found that 88 (72.1%) of the children presented with spastic CP; neonatal anoxia was the main cause (64; 52.5%); 47 (38.5%) were diagnosed in the first month of life; and 92 (75.4%), in addition to motor impairment, displayed other disorders, such as speech problems. Conclusions: the data revealed that the children with CP had unique characteristics that required multidisciplinary care, on an interdisciplinary approach, because the earliest possible intervention is necessary to improve their performance in performing activities of daily living.
Keywords: Cerebral Palsy; health profile; nursing.
INTRODUCTION
Cerebral Palsy (CP), a chronic, nonprogressive, childhood encephalopathy is a predominantly sensorimotor dysfunction involving muscle tone, posture and voluntary movement disorders that occurs in the pre-, peri- or postnatal period and affects the central nervous system in the phase of structural and functional maturation1,2.
CP is defined as a group of disorders of the central nervous system that affects children, without progressive character and that clinically presents motor disorders, that is, changes in movement, posture, balance and coordination, with a variable presence of involuntary movements. The most accepted definition in the view of specialists dates back to 1964 when cerebral palsy (CP) was characterized as a permanent disturbance of movement and posture as a consequence of the non-progressive defect or lesion of the brain at the beginning of life that does not vary with time 3.
Every year in the European Union, around 10,000 children are diagnosed with CP, a condition that can take many forms, as most children have their health and welfare affected4.
Nursing plays a key role in the care of this clientele; this service ranges from the early detection of the disturbance during childcare consultations to support and guidance of families with CP children, as well as acting as a component of the multiprofessional team in the context of early encouragement, which is essential for this clientele.
A thorough investigation of all family and domicile aspects is important to know the reality that CP children live and consequently collaborate to a targeted multiprofessional care, especially that of the nursing team, with the goal improving its performance.
There is no way to provide quality care to children in such peculiar situation without knowledge of the characteristics and the reality of life in which they are inserted. Thus, the objective of this study was to describe the profile of parents and children with cerebral palsy assisted in outpatient clinics in Fortaleza, Ceará.
LITERATURE REVIEW
Early identification of CP and developmental delay is an important goal for rehabilitation professionals because interventions in early childhood can minimize common motor deficiencies and disabilities in this population 5.
In order to describe the functionalities and disabilities related to health conditions as interactive and evolutionary processes, the Pan American Health Organization (PAHO) has published the International Classification of Functionality (ICF) which describes functionality and disability related to health conditions, identifying what a person has or not conditions to perform as an activity of daily life6.
The ICF classifies functionality and disability processes of an individual, which result from the interaction between the health condition and personal and environmental factors, into three categories, namely, body structure and function, activity and participation. These are interdependent and influenced by the context. According to this model, the environment in which the individual acts can work as a facilitator or as a barrier to their functional and social performance and should therefore be considered in the therapeutic process1,7.
In CP children, the home environment should be consistently evaluated in order to identify the necessary modifications to promote the participation and independence of these children in daily activities8. Indeed, knowledge of the environment in which the child is inserted facilitates the follow-up by health professional, since the rehabilitation process takes place according to the reality of each child.
In order to avoid the progression of disabilities in CP children, it is essential to implement early intervention services to habilitate and guide parents and make them aware of the special needs of their children, facilitating their development. The intervention needs to happen as soon as possible when brain plasticity is high, capable of receiving normal sensations and integrating them into growth2.
The process of rehabilitation and treatment of CP children depends on the commitment of family members and professionals responsible for early intervention and stimulation programs, besides the use of pharmacological and even surgical therapy, a process that demands time, costs and availability.
METHODOLOGY
This is a descriptive study with quantitative approach developed with 122 parents of CP children assisted at two outpatient and rehabilitation health institutions in Fortaleza, CE, from October 2012 to January 2013.
The target population of the study involved parents of CP children who were attended at the places established for data collection. The search for the informants occurred through consultation of medical records, as well as through collaboration of professionals who provided assistance to these children. The following inclusion criteria were adopted to select the sample: parents of children with a confirmed medical diagnosis of CP and in the age group of four to twelve years, since this is the recommended age for the application of the quality of life scale applied in the present study – which is a translated and validated scale - and parents regularly assisted at their respective outpatient clinics during the collection period. Parents with any cognitive impairment that prevented them from answering the questionnaires were excluded.
Data collection was performed daily, during the day shift, with the parents of the children who were in the waiting room of the outpatient clinics, while their children were in consultation. Data were collected with the help of four nursing students who were trained to participate in the study. We used a form developed by the researchers to obtain socioeconomic, demographic and clinical information.
For analysis of the information, a database was prepared in an electronic spreadsheet for descriptive and inferential analyses, using the program Excel 2003, and the information collected was exported and organized into the Program Statistical Package for the Social Sciences (SPSS Inc. Chicago, United States) version 20.0. Exploratory analysis of data consisted of descriptive statistical tests and absolute and relative frequencies, means (M) and standard deviations (SD).
The ethical precepts of Resolution 466/2012 were considered9 and the study was approved by the Research Ethics Committee (COMEPE) of the institution, under Opinion nº 197/11.
RESULTS AND DISCUSSION
Sociodemographic characterization of the sample
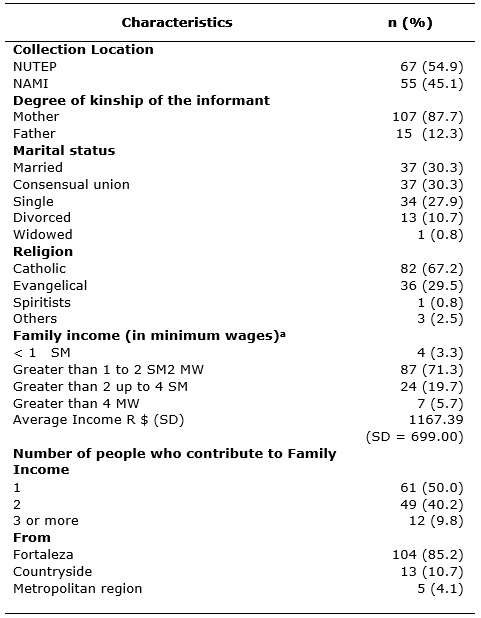
From a total population of 146 parents of children aged four to 12 years, 122 participated in the study. Twenty-four parents did not participate in the study due to health problems of their children, frequent hospitalizations, difficulty faced by the parents to move with the children and frequent dropout of treatment because of slow evolution. The sociodemographic characteristics of the participant parents are shown in Table 1.
TABLE 1:
Sociodemographic characteristics of the informants of children with
cerebral palsy (n = 122). Fortaleza, CE, Brazil, 2013.
Note:
Minimum wage at the time of research R$ 622.00 ($ 2.10).
The profile of informant mothers deserves to be highlighted. They were the majority, 107 (87.7%) of a total of 122. While the fathers had their jobs, these mothers were mostly housewives. They were responsible for taking the children to the hospital. Similar profiles have been found in other studies with CP children. In order for a CP child to be able to carry out daily activities in an effective and safe way, the constant help of a caregiver is necessary11.
As for the religion of the informants, the Catholic religion was predominant, corresponding to 82 families (67.2%), while there were 36 (29.5%) families belonging to the evangelical religion. Religiousness has implications in the phenomena related to health and illness, and it as acts as a promoter of emotional, instrumental and informative support 12.
The per capita income of 87 families (71.3%) was low, with a predominance of income between one and two minimum wages. This income was generated by only one person in the family in the case of 61 families (50%). This income profile is similar to that found by Frota et al.13, when the salary was R$ 622. In view of this financial reality, it can be seen that the support sources and social networks can be considered a means of promoting health, the financial aspect is an element of social vulnerability and when it is limited, becomes an important source of worry and anguish14,15.
Parents of children with cerebral palsy have a higher level of stress than parents with children without disabilities, which reinforces the need for family support16. It has been reported that mothers present a greater level of suffering, due to the impacts that the continuous care entails for their lives17. The main social support networks are usually composed by professionals from institutions for treatment of children with special needs, family members and religious institutions. Nurses can provide support and identify needs and possible support networks, directing the family in the search for help18-20.
The choice of two outpatient clinics in the city of Fortaleza, CE, allowed a representative sample of this clientele, since 104 informants came from the capital (85.2%), and 13 from the countryside (10.7 %) of the state of Ceará and five from the metropolitan region 5 (4.1). This indicates a profile of people born and educated in the countryside of the State who have a cultural and social background which is appropriate to obtain a differentiated view of the reality of the lives of the informants.
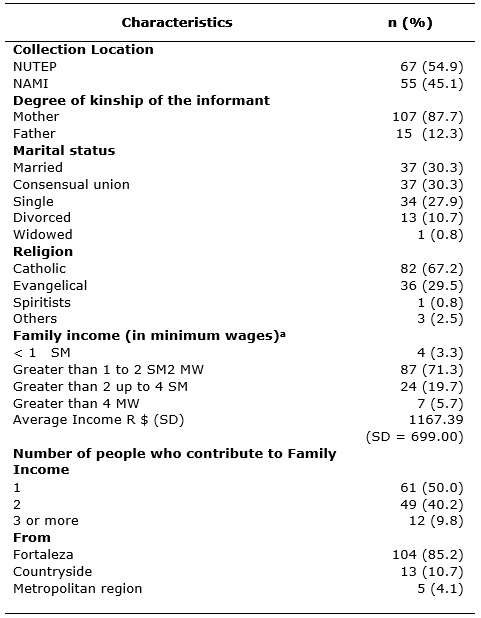
Table 2 shows that the mean age of the fathers was 37.2 years (SD = 8.7), they had a mean of 10.6 years of schooling (SD = 3.3) and the majority 80 (65.6%) was employed at the time of data collection. In the case of mothers, the mean age was 34.6 years (SD = 7.8), they had more years of schooling than fathers, with a mean of 11.2 years (SD = 3.2), equivalent to Complete Elementary school. This profile of low schooling is common in the Brazilian population, as shown by Morales' studies21, in which 50% of the sample of CP children in the south of the country had incomplete elementary education.
TABLE 2:
Sociodemographic characteristics of mothers and fathers of children with
cerebral palsy (n = 122). Fortaleza, CE, Brazil, 2013.
In relation to the characteristics of the domicile where the children assisted at the data collection sites lived, the data revealed that most of them lived in good conditions; all 122 (100%) lived in brick houses, most lived in houses with ceramic flooring 73 ( 59.8%), with electric power 100 (122)and basic sanitation 83 (68%). The houses were considered spacious, since 88 (72.1%) had more than three rooms and hosted mostly three to four people 69 (56.6%).
The homes of the CP children presented good hygiene conditions. This data is important considering that a clean house interferes with the improvement of health of this kind of patients considering that the clinical situation of children make them stay home most of the time. Hygiene in the home environment has a great positive impact on them13.
Clinical characteristics of the CP children
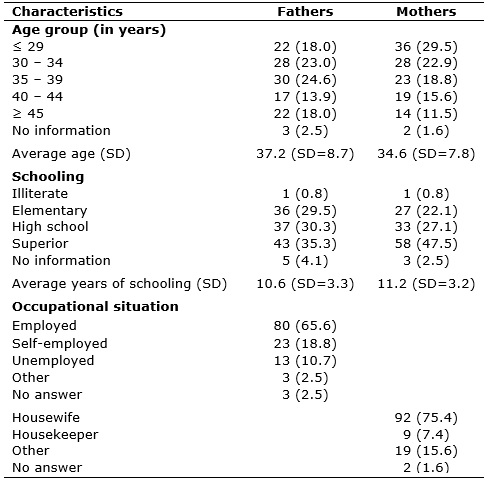
Table 3 presents the clinical characteristics of the CP children. Equal percentage distribution was observed between the male and female gender (p = 0.836). The age range of CP children met the requirements of the scale, varying from four to 12 years, with predominance of the age group of six to eight years 57 (46.7%), both in relation to the male 30 (49.2% ), and female 27 (44.3%).
TABLE 3:
Clinical characteristics of children with cerebral palsy (n = 122).
Fortaleza, CE, Brazil, 2013
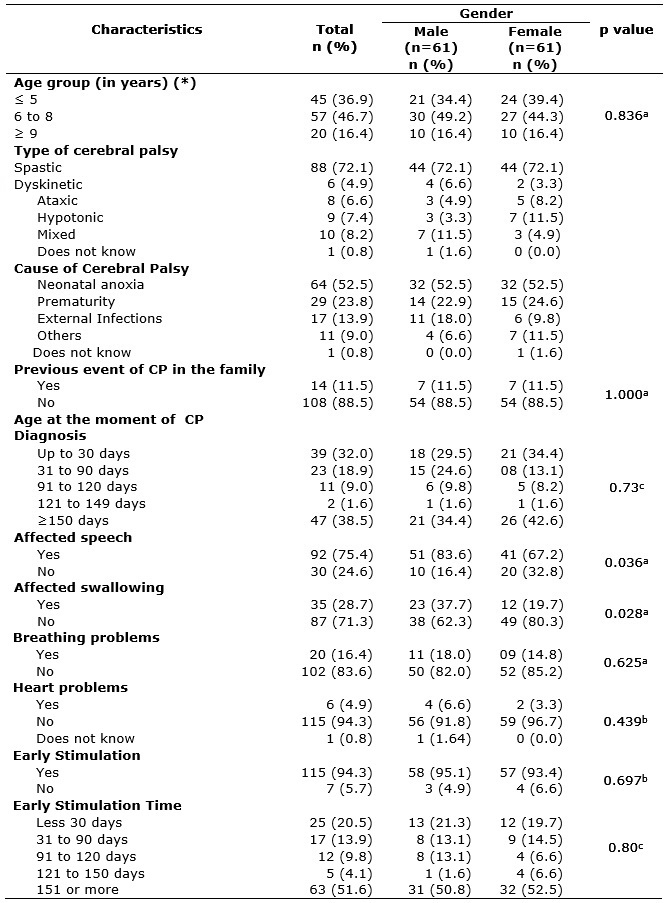
Note:
Pearson's chi-square test; Fisher's exact chi-square test; cTest Chi-square
of Trend.
When CP is diagnosed, the patient receives a classification that varies according to their clinical characteristics. In the population studied, spastic CP predominated 88 (72.1%), being equally distributed among male 44 (72.1%) and female 44 (72.1%) children. In spastic forms of CP, the child presents hypertonia, in which there is resistance to rapid muscle stretching, and can be classified according to varied degrees of limb involvement, which was not assessed in the present study. Spastic children present hypertonia, in which there is resistance to rapid muscle stretching, and may be sub-classified according to varied degrees of limb involvement2.
Data revealed that the main cause of CP was neonatal anoxia 64 (52.5%), with no differences between genders; the second cause was prematurity 29 (23.8%), and the third external infections 17 (13.9%),the later predominant in males 11 (18%), besides other causes which were not revealed in this study 11 (9%). It is also observed that CP was not frequent in the family of these children, since only 14 (11.5%) had a family history of CP, and 108 (88.5%) had no other cases of CP in the family, thus rejecting the possibility of an hereditary factor involved in the pathology. These data agree with Lima and Fonseca2 when they say that the most common cause of CP is neonatal asphyxia, and other causes are prematurity and CNS infections, but no report of etiological factors related to heredity.
It was also verified that the predominant age at which CP was diagnosed was 150 days of life, corresponding to five months of age 47 (38.5%), although there are considerable numbers of children diagnosed with less than one month of life (39.32%), there was no trend of proportional increase in gender and age at diagnosis (p = 0.73). Early diagnosis of CP is relevant for prompt professional intervention, favoring a better prognosis 13. The children in the resent study were diagnosed at different ages, ranging from birth to more than six months of age, with predominance of diagnosis in the age group over six months.
In addition to motor impairment, some of the children presented other health problems caused by CP, such as: speech problems 92 (75.4%), and less frequent but not less important, swallowing problems 35 (28. 7%). There were statistically significant proportional differences by sex regarding speech problems (p = 0.036) and swallowing (p = 0.028).
Lack of coordination between the motor actions necessary for swallowing can have serious consequences such as vomiting during feeding, nasopharyngeal regurgitation, malnutrition, growth retardation, suspicion of aspiration, occurrence of cough during feeding and repetitive pneumonias22. Dysphagia is associated with an increased risk of aspiration pneumonia, dehydration and malnutrition, which may increase morbidity and mortality in affected patients23.
The abovementioned events explain the fear and apprehension of families regarding the risk of bronchial aspiration of the child, besides the diversity and complexity of oral and gastrostomy feeding. Multiprofessional assistance in the management of this family need is very important. Speech therapy with the role of diagnostic evaluation of swallowing-related aspects24-26 is very important. Nursing, in turn, is relevant to the technique of offering the diet; nutrition as to the quality and quantity of the diet to be offered, in addition to the support of other professionals in outpatient and home care. It is evident that the responsibility to care of CP patients must be shared among professionals.
In the literature, convulsions, spasticity, changes in postural tonus and daily activities are reported as the main difficulties in the care of CP children, with parents being the main responsible for this care.
As evidenced in the study of Wong, Bartlett, Chiarello26 who presented quantitative data showing that the degree of CP involvement is directly proportional to cardiac problems manifested; 6 (4.9%) of the children presented this disease in the present study. Other result of the study was to the presence of respiratory problems with a higher percentage 20 (16.4%) than cardiopathies.
The fact that the CP children have difficult locomotion as main sequel, monitoring from a multiprofessional and interdisciplinary team that develop activities of early stimulation is necessary. All the children in this study 122 (100%) had been under this assistance, 25 (20.5%) of them for at least 30 days, and most of the children 63 (51.6%) were under early stimulation for 151 days or more. This data show the commitment of the parents with the rehabilitation process of their children.
As a way to avoid the progression of disabilities in CP children, it is of utmost importance that early intervention services be provided as well as guidance be given to parents so that they can be made aware of the special needs of their children, facilitating the development. Intervention needs to be early in order to reach as quickly as possible an immature brain capable of receiving normal sensations and integrate these sensations into growth2. The scores found revealed that most of the children underwent early stimulation during the data collection period.
An example that shows that stimulation promotes health benefits to the child was given in the study27, in which a slight improvement in the swallowing pattern of CP children was observed after a speech-language intervention, which consequently led to a better feeding pattern of the patients.
It is recognized the need of care for the CP children by interdisciplinary teams that may allow a more complex look on these patients and their families. The professionals involved in the process of rehabilitation (nurses, physical therapists, speech therapists, occupational therapists, physicians, among others) should involve the families in the process of co-responsibility and seek, along with them, resources and alternatives so that children perform activities that stimulate neuro-psychomotor development, in a care process based on technical-scientific knowledge and humanization28-30. Thus, the importance of parental participation in the process of children rehabilitation through the implementation of a favorable home environment and the encouragement of activities of daily living30 are highlighted.
CONCLUSION
According to this study, among the peculiar characteristics of CP children, the majority had mothers as caregivers, who were prevented from having a profession, lived with their partners in consensual union, without formal bond, and depended financially on them, had a family income of up to two minimum wages, characterizing them as part of a low socioeconomic stratum.
Regarding the clinical characteristics of children, the majority was classified as spastic CP children, whose CP had been caused by neonatal anoxia and additionally had motor involvement, other alterations, with speech problems being the more frequent. These clinical aspects show the impact of the disability on the family as an indisputable fact, which changes family dynamics, differently for each of member, causing the need to restructuring their lives.
Faced with this reality, nurses must identify these clinical changes as early as possible, during the childcare consultation, make the appropriate referrals to a multiprofessional team and periodic monitoring in order to allow interventions as early as possible and improve performance in the execution of the activities of daily living. Thus, the study revealed that many aspects should be taken into account in promoting clinical or educational interventions and in the construction of public policies for children with disabilities.
REFERENCES
1.World Health Organization. International classification of functioning disability and health. Geneva (SW): WHO, 2001.
2.Lima CLA, Fonseca LF. Cerebral Palsy: neurology, orthopedics, rehabilitation. Rio de Janeiro (RJ): Guanabara Koogan Publisher; 2008.
3.Leite JMRS, Prado GF. Cerebral Palsy: Physiotherapeutic and clinical aspects. Neuroscience Journal. [SciELO-Scientific Electronic Library Online] 2004 [cited on Sep 20, 2016] 12: 1. Available from: http://www.unifesp.br/dneuro/neurociencias/vol12_1
4.Beckung E. et al. Health status of children with cerebral palsy living in Europe: a multi-center study. Child: care, health and development. 2008, 34 (6): 806-814.
5.Lacerda TTB, Magalhães LC. Analysis of the validity of the Movement Assessment of Infants (MAI) items for preterm infants. Brazilian Journal of Maternal and Child Health. 2006, 6 (3):297-308.
6. Pan American Health Organization. ICF: International Classification of Functioning, Disability and Health. São Paulo (SP): OPS; 2003.
7.Farias N, Buchalla CM. The International Classification of Functioning, Disability and Health of the World Health Organization: concepts, uses and perspectives. Brazilian Journal of Epidemiology. 2005, 8 (1): 187-93.
8.Guerzoni VP et al. Analysis of occupational therapy interventions in the performance of daily living activities in children with cerebral palsy: a systematic review of the literature. Brazilian Journal of Maternal and Child Health. 2008, 8 (1): 17-25.
9. Ministry of Health (Br). National Health Council Resolution Nº 466/2012. Regulatory guidelines and norms of research involving human beings. Brasília (DF): National Health Council; 2012.
10.Milbrath VM et al. Mothers experiencing the diagnosis of cerebral palsy in their children. Ver Gaúcha Enferm 2009, 3 (30): 437-44.
11.Assis-Madeira EA, Carvalho SG, Blascovi-Assis SM. Functional performance of children with cerebral palsy of high and low socioeconomic levels. Rev. paul. pediatr. [Internet]. 2013 Mar [cited on July 19, 2017]; 31 (1): 51-57. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-05822013000100009&lng=en . http://dx.doi.org/10.1590/S0103-05822013000100009 .
12.Faria JB, Seidl EMF. Religiosity and coping in health and disease contexts: literature review. Psychology: Reflection and Criticism. 2005, 18 (3): 381-89.
13. Frota MA et al. Quality of Life Assessment in Children with Cerebral Palsy. International Archives of Medicine 2016, 9 (1): 1-9.
14.Paula ES, Nascimento LC, Rocha SMM. Religion and spirituality: experience of families of children with Chronic Renal Insufficiency. Rev bras enferm. 2009, 62(1):100-6.
15.Baltor MRR, Dupas G. Experiences of families of children with cerebral palsy in a context of social vulnerability. Rev Latino-am enfermagem. 2013; 21 (4): [08 screens]
16.Ribeiro MFM, Porto CC, Vandenberghe L. Parental stress in families of children with cerebral palsy: integrative review. Collective Health Science. 2013; 18 (6): 1705-15.
17. Colesante MFL, Gomes IP, Morais JD, Collet. Impact on the life of mothers caring for children with chronic diseases. Rev Enferm UERJ. 2015; 23(4):501-6.
18.Polita NB, Tacla MTGM. Cerebral palsy and social support to families. Anna Nery School Nursing Journal. 2014; 18(1):75-81
19. Sandor ERS, Marcon SS, Ferreira NMLA, Dupas G. Demand for social support by the family of the child with cerebral palsy. Rev eletr Enf. 2014; 16(2):417-25.
20.Dezoti AP, Alexandre AMC, Freire MHS, Mercês NNA, Mazza VA. Social support to families of children with cerebral palsy. Acta paul enferm. 2015; 28 (2): 172-6.
21.Morales NMO. Transverse evaluation of the quality of life in children and adolescents with cerebral palsy using a generic instrument (CHQ-PF50). 2005 119f. Dissertation (masters in health sciences). Federal University of Uberlândia, Minas Gerais, 2005.
22.Vaiman MEE. Surface electromyography as a screening method for evaluation of dysphagia and odynophagia. Head Face Med. 2009, 5 (9): 1-11.
23.Rugiu MG. Role of videofluoroscopy in the evaluation of neurologic dysphagia. Acta Otorhinolaryngol Ital. 2007, 27 (6): 306-16.
24.Furkim AM et al. The use of cervical auscultation in the inference of tracheal aspiration in children with cerebral palsy. Rev CEFAC 2009, 11 (4): 624-69.
25.Wong C et. al. Comparison of the prevalence and impact of health problems of pre-school children with and without cerebral palsy. Child: care, health dev. 2011; 38(1):128-38.
26. Coutinho KAA, Pacheco STA, Rodrigues BMRD, Silva LF. Home care of family members regarding the feeding of children with encephalopathy. Rev nursing UERJ. 2015; 23(3):318-23.
27.Vianna CIO, Suzuki HS. Cerebral palsy: analysis of swallowing patterns before and after speech-language intervention. Rev. CEFAC 2011, 13(5):790-800.
28.Geralis E. Children with cerebral palsy: a guide for parents and educators. 2 ed. Porto Alegre: Artmed; 2007.
29. Cestari VRF, Barbosa IV, Carvalho ZMF, Melo EM, Studart RMB. Scientific evidence on childhood cerebral palsy. Cogitare enferm. 2013; 18(4):796-802.
30.Ribeiro J, Beltrame TS. Characteristics of broad motricity in students with cerebral palsy enrolled in special school. Dynamis 2008, 14(3):14-28.