(*) Standard Deviation; (**)Minimum value; (***)Maximum value; (****)Kolmogorov-Smirnov test.
ORIGINAL RESEARCH
Cardiovascular and pulmonary changes in patients undergoing hemodialysis
Maria Isabel da Conceição Dias FernandesI; Cyndi Fernandes de LimaII; Cecília Maria Farias de Queiroz FrazãoIII; Millena Freire DelgadoIV; Marilia Gabriela de Azevedo AraujioV; Ana Luisa Brandão de Carvalho LiraVI
I
Nurse. Master degree. Ph.D. student in Nursing at the Federal University of
Rio Grande do Norte. Natal, Rio Grande do Norte, Brazil. E-mail: bebel_6@hotmail.com
II
Nurse. Federal University of Rio Grande do Norte. Natal, Rio Grande do
Norte, Brazil. E-mail: cyndi_fl@hotmail.com
III
Nurse. Ph.D. Substitute Professor. Federal University of Pernambuco.
Recife, Pernambuco, Brazil. E-mail: ceciliamfqueiroz@gmail.com
IV
Nurse. Master degree student in Nursing at the Federal University of Rio
Grande do Norte. Natal, Rio Grande do Norte, Brazil. Email: millenadelgado@gmail.com
V
Nurse. Resident at the Pediatric Hospital Professor Eriberto Ferreira
Bezerra. Federal University of Rio Grande do Norte. Natal, Rio Grande do
Norte, Brazil. E-mail mariliagabi@yahoo.com.br
VI
Nurse. Ph.D. Associate Professor. Department of Nursing at the Federal
University of Rio Grande do Norte. Natal, Rio Grande do Norte, Brazil.
E-mail:
analuisa_brandao@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.8634
ABSTRACT
Objective: to identify cardiovascular and pulmonary changes in hemodialysis patients and correlate them with socioeconomic features. Method: this cross-sectional study was conducted at a university hospital and a dialysis clinic in Northeast Brazil. Data was collected between December 2012 and April 2013 by interview and physical examination. Chi-square and Mann-Whitney tests were used. The study was approved by the research ethics committee (Opinion No. 148 428). Results: the most frequent cardiovascular changes were in edema, blood pressure, central venous pressure and positive hepatojugular reflux. Pulmonary changes were pulmonary congestion and adventitious breath sounds. The variables dyspnea and altered breathing patterns showed statistically significant associations with family income. Conclusion: cardiovascular and pulmonary changes are frequent in the study clientele and these problems may be influenced by socioeconomic particulars.
Keyword: Nursing; chronic renal failure; cardiovascular system; respiratory system.
INTRODUCTION
The Brazilian population was approximately 194 million people in 20121. In 2013, the estimated total of patients on dialysis was 100,397. This number of patients in treatment has almost doubled in the last ten years2. Thus, the chronic kidney disease (CKD) is considered a public health problem.
The CKD is a pathological and physiological process associated with several etiologies, in which there is a progressive and irreversible loss of functional nephrons. It is classified in stages, defined according to glomerular filtration rate (GFR). It is used to measure the plasma filtration from the kidneys, being considered the best technique for evaluating the index of renal function3.
The progressive and irreversible loss of renal function may be divided into six functional stages according to the glomerular filtration rate, representing the degree of loss of renal function. In advanced stages, CKD is called chronic renal failure (CRF), when there is the appearance of clinical and laboratory findings, observing that organs and systems work abnormally and may accumulate uremic toxins in the body4.
Thus, it is necessary to renal replacement therapies to maintain the electrolyte balance and acid-base occurring in the body and the filtration of nitrogenous excreta. Among the dialysis models the hemodialysis (HD), the continuous replacement therapy (CRRT) and the peritoneal and hemofiltration dialysis are highlighted5. These treatments promote the relief of symptoms, as well as preserving the lives of patients with CKD, but do not promote healing6. Among the treatment options, the HD is the main choice7, even negatively affecting the quality of life of the individual8. The HD consists in filtering excreta and toxins in the blood, through a dialyzing machine, requiring vascular access for its performance5.
Although hemodialysis is considered quite effective and postpones the life of patients with CKD, it does not replace the renal function of the patient completely. Thus, the individual may have different clinical manifestations due to uremia, such as hematological, neurological, soft tissue, cardiovascular, pulmonary, gastrointestinal, reproductive and musculoskeletal manifestations7.
Among the complications found in this patient can highlight heart failure associated with dyspnea, orthopnea, pulmonary and peripheral edema, as well as a possible increase in cardiac debt9. It is known that the presence of cardiovascular disease (CVD) is responsible for the highest rates of morbidity and mortality in the population, especially those with CKD10.
Linked to the cardiovascular problems in patients with CKD ongoing hemodialysis, there are the pulmonary events, which are commonly identified in this patients for various causes11,12. Among these pulmonary changes, there are pulmonary congestion problems identified in the literature as extremely common in CKD patients in the terminal stage. This change is reflected in the left ventricular disturbances superimposed on the overhead liquid volume, besides being strongly associated with poor physical performance and be a strong predictor of death and cardiovascular events13.
In this context, it is noticed from the studies, the severity of respiratory and cardiovascular changes for customers on hemodialysis, having in mind the possibility of death when there is no effective intervention. Thus, it is important to check the occurrence of cardiovascular and respiratory changes in chronic renal failure patients on hemodialysis and relate them to socio-economic data. These observations support nurses facing the prevention as well as to the context in which these patients are included, a fact that will subsidize prerogatives to nurse thinking on what interventions would be effective to arise such changes, allowing to link care strategies and targeted education for preventive and health promotion, in the process of care and maintenance based health humanization and quality of the health service.
Thus, from the above, the aim of this study was to identify cardiovascular and pulmonary changes in patients undergoing hemodialysis, together with the socioeconomic aspects.
LITERATURE REVIEW
By their health status, Chronic renal patients may be susceptible to different comorbidities associated with CKD. Among them, there are the cardiovascular and pulmonary changes, which are responsible for high mortality rates in this population. CKD increases the risk for cardiovascular disease (CVD) when linked with risk factors: smoking, age, gender, physical inactivity, systemic arterial hypertension (SAH) and diabetes (DM)14.
Furthermore, CVD increases the risk for development of CKD, since both are associated with common risk factors such as hypertension, diabetes mellitus, malnutrition, inflammation, and atherosclerosis14. These characteristics make the difference in chronic renal patient and their cardiovascular evaluation.
Regarding the lung changes, the hemodialysis treatment is associated with changes in respiratory mechanics, since there is a significant improvement in the respiratory pattern after reduction in blood volume after ultrafiltration. This fact can be explained by the redistribution of pulmonary ventilation and improved uremia after hemodialysis. It may also be suggested that substitutive renal therapy promotes the reduction of edema by providing a dynamic fluid between the interstitial and intravascular spaces15.
METHODOLOGY
This is a cross-sectional study conducted in a university hospital and a hemodialysis clinic in northeastern Brazil. The formula of infinite proportion was used to calculate the sample size. As parameters, there was a confidence level of 95% conjectured sensitivity of indicators of 85%, one-half of the length of the confidence intervals constructed of 10%, and a proportion of 50%. Applying the formula, it was reached a value of 98 individuals, who chose to end with 101 patients.
The inclusion criteria adopted were: being a patient of chronic kidney disease; performing hemodialysis; being the first hour of hemodialysis and being 18 years old. The exclusion criterion adopted was: being in physical and mental condition impaired at the time of data collection. The sampling process occurred consecutively for convenience.
The collection took place between December 2012 and April 2013. Data were obtained by the primary source, through the interview and physical examination, by an instrument with open and closed questions, divided into socioeconomic data, clinical, general physical examination and segments.
Cardiovascular and pulmonary manifestations analyzed in this study were: jugular venous distension, edema, changes in blood pressure, increased central venous pressure, positive hepatojugular reflux, heart sound B3, change in blood pressure, pulmonary congestion, pleural effusion, dyspnea, change in breathing pattern, orthopnea, and anasarca adventitious breath sounds. They were judged by their presence or absence in patients investigated by the researchers.
For data analysis, PASW Statistic version 19.0 for Windows program was used. Therefore, descriptive statistics were used stipulating the relative and absolute frequencies, mean, median, standard deviation, maximum and minimum. It was also performed the inferential analysis using the chi-square test and Mann-Whitney test to verify the existence of a statistical association between socioeconomic variables and the above changes. Thus, to the statistical significance of the specified tests a level of 5% was adopted (p <0.05).
This study was approved by the Research Ethics Committee, through the opinion Nº 148428 and Certificate Presentation of Findings Ethics Nº 08696212.7.0000.5537. The patient expressed his acceptance to participate in the study by signing the Consent Form.
RESULTS
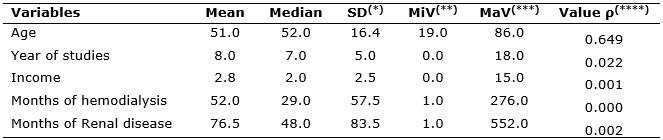
Regarding socioeconomic data, the results show that the majority of respondents were females (52.5%), and the mean age was 51 years old (± 16.4), with a minimum of 19 and maximum of 86 years old. In the years of study, the median was seven years (± 5.0) with a variation of zero to 18 years. Family income is presented with a median of 2 minimum wages (± 2.5). Regarding the time of completion of the hemodialysis treatment, the median was 29 months (± 57.5) and the months with chronic kidney disease got a median of 48 months (± 83.5), as shown in Table 1.
TABLE 1:
Socioeconomic and clinical data of chronic renal failure patients
undergoing hemodialysis in a renal disease clinic and a university
hospital. Natal-RN, 2013.
(*)
Standard Deviation; (**)Minimum value; (***)Maximum
value; (****)Kolmogorov-Smirnov test.
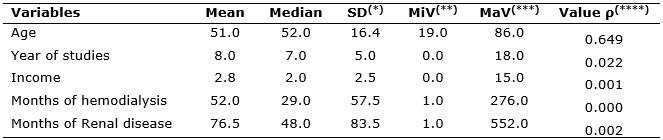
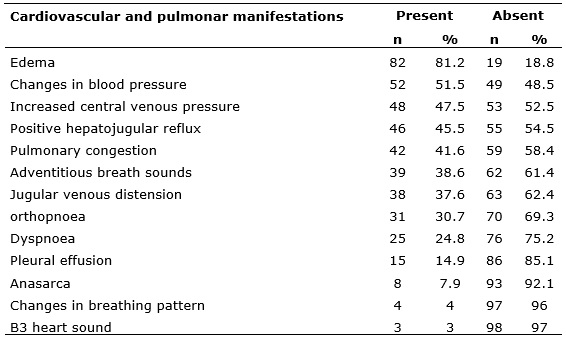
Related to cardiovascular and pulmonary disorders presented by patients, edema stood out as the most common problem (81.2%), followed by the change in blood pressure (51.5%) and central venous pressure (47.5%), as shown in Table 2.
TABLE 2:
Cardiovascular and pulmonary changes identified in chronic renal failure
patients undergoing hemodialysis in a renal disease clinic and a university
hospital. Natal-RN, 2013.(N=101)
On the existence of a statistical association between cardiovascular and pulmonary changes and socioeconomic data, the association was found between the manifestations dyspnea and change in breathing pattern with variable income, which showed values of p=0.0458 and p=0.034 respectively. These data are presented in Table 3.
TABLE 3: A
nalysis of the association between cardiovascular and pulmonary changes and
socioeconomic data of research subjects. Natal-RN, 2013
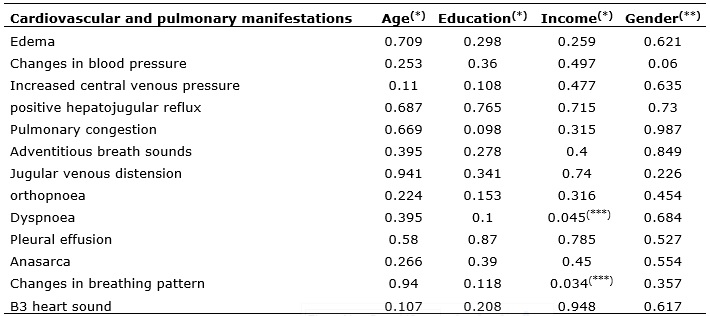
(*)
U Test of Mann-Whitney; (**) Chi-square test; (***)
Value p below 0,05.
DISCUSSION
From the data obtained in the study, the prevalence of subjects studied among the 101 CKD patients on dialysis were female, in contrast to the data in the literature, in which the highest percentage is male2. The average of age in the study was 51 years old, differing from the findings in the literature, showing that the average age of such individuals is 49 years old16. Being a predisposing factor for many chronic diseases, including CKD, it is a fact of great relevance16,17.
Regarding education, the average identified was eight years of study. Similar research carried out with the same kind of patients, revealing the low education level of respondents. On the other hand, family income with an average of 2.8 minimum wages, was above the commonly identified value compared with another study in which patients had income equal or less than two minimum wages16,17.
On the cardiovascular and pulmonary changes investigated in these patients, the edema was highlighted, being found in 81.2% of the sample. This finding, in these specific patients, is justified by the fact that there is an inability of the kidneys to excrete water, sodium and other adequate solutes of these individuals7. Thus, as a consequence, although hemodialysis is performed, the accumulation of fluid is unavoidable 18.
According to Roy Theory in a study to evaluate the adaptive problems of HD patients, revealed that most of these patients have swelling due to renal injury19, a fact that corroborates the findings of this study in which 81.2% of the population is with edema. Its occurrence is responsible for complications that lead to chronic renal emergency service and is also associated with weight gain, pulmonary edema20, besides having a direct relationship with the development of heart failure18,21.
The second most prevalent change was the change in blood pressure, present in 51.5% of patients. It is worth noting that for the evaluation of such a change were considered two values for its assessment, after the completion of hemodialysis and 48 hours before starting it, and investigated the variation in interdialytic period. According to the literature, the hemodialysis tends to promote hemodynamic changes in patients, as one of its objectives is the removal of excess fluid7.
Hypotension during dialysis is a change often present in these patients, representing one of the major complications of hemodialysis. This change is due to the removal of excess fluid during treatment, causing hypovolemia, inducing sympathetic activation of the nervous system, triggering the increase in heart rate and total peripheral resistance, which affects in a vascular imbalance and interfere with maintenance blood pressure 22. However, hypertension is less common (21.2%) as complications during hemodialysis sessions, associating with greater intensity as a risk factor for the development of CKD23.
Increased central venous pressure (CVP) was the third most prevalent manifestation (47.5%), which is considered the most variable used to estimate the volume status and cardiac function of patients. This measure assesses the pressure in the right atrium and large intrathoracic vein, and it reflects the filling pressure of the left heart, which consist of the most important venous pressure since they provide three parameter information were found blood volume, heart efficacy as pump and vascular tone7. In this study, CPV elevation was probably related to excess fluids identified in these patients.
Of the patients enrolled in this study, 45.5% had positive hepatojugular reflux. The presence of this manifestation has a strong link with cardiovascular disease, due to the decreased venous return secondary to the left ventricular failure, being aggravated by this accumulation of fluid in this patients7.
Pulmonary congestion is determined and evidenced by percussion and the presence of moist crackles on auscultation, audible especially in lung bases. It is transfigured as fluid accumulation in the pulmonary interstitial space due to increased blood volume and pulmonary venous pressure that forces blood from the pulmonary capillaries into the lung tissue and alveoli24.
In this study, pulmonary congestion was in 41.6% of patients, which corroborates a study in which 45% of hemodialysis patients had such a problem. According to the same study, 71% of patients with moderate to severe pulmonary congestion were asymptomatic or with mild symptoms of heart failure13.
The adventitious lung sounds, auscultation in 38.6% of participants for an abnormal condition occurs that reaches the bronchi and/or alveoli, which can be filled by thick secretions or fluids and/or provide a decrease in the light of the airways. Therefore, according to the type of abnormal condition, these are classified as crackles, wheezes, and snores 7. In the study, patients were considered only crackles since the occurrence of this type of noise n this specific patient is the most prevalent.
The jugular venous distension, identified in 37.6% of patients, is a measure which indicates changes in the volume of right heart chambers, and salt and water retention is a marker commonly found in systemic congestion due to right heart failure or advanced Bi-ventricular25. In this perspective, it is known the high incidence of heart failure in patients with chronic renal failure, which justifies the identification of such a manifestation26.
The orthopnea, present in 30.7% is defined as the sensation of breathlessness when the individual is in the supine position, being a better disposal for gas exchange when the head is in the high bed or sitting, being associated, commonly, to patients with cardiac or respiratory diseases7. Similar to our study, the presence of orthopnea in 55.4% of the sample was identified in research about the signs and symptoms in patients with decompensating heart failure27.
The dyspnoea, feeling reported by 24.8% of patients, is characterized by respiratory distress symptom. It is identified in 100% of chronic renal failure patients on hemodialysis study on the prevalence of dyspnea in this patient. However, it was also identified that this symptom is quite relieved after hemodialysis28.
Moreover, this demonstration was statistically associated with the income (0.045) and although there are no reports in the literature about the relationship between these variables, it can be inferred that low-income presented by the investigated sample (2.8 salaries) can influence non-adherence to prescribed drug treatment and difficulties in access to hemodialysis, which affects the failure treatment29, contributing to the occurrence of dyspnea, intrinsically problem related to accumulation of fluid in these individuals.
Pleural effusion, observed in 14.9% of patients, was a collection of abnormal fluid in the pleural space, few find prevalent in the sample. However, it is commonly found in patients with CKD. Its pathogenesis may be mainly associated with diastolic heart failure, volume overload, and uremia 30. In the pleural space, there is a small amount of liquid, about 5 to 15 ml, which allows lubrication and avoid friction between the pleural surfaces. However, when the volume of liquid in the space exceeds the normal, it can cause some complications to the affected patient, such as cardiac arrest7.
Pleural effusion can be a complication of heart failure, nephrotic syndrome, and CKD. The nurse may review the occurrence of pleural effusion performing auscultation of breath sounds, which may be absent or diminished, and observe the thrill and perform percussion, which presents a massive or submassive sound7.
The anasarca, identified in 7.9% of the sample appears as a generalized, progressive and chronic edema, directly inter-related to renal function, which is responsible for regulation of water balance, sodium, and other solutes. This signal occurs due to the increase of body fluids by transferring these into the interstitial space. The extravasation usually occurs in the pleural, abdominal cavity, the lower and upper limbs, genitals and face31.
Changes in breathing patterns mean changes in breathing amplitude associated with the change in their frequency, may be associated with ineffective airway clearance. The frequency should not exceed the minimum and maximum values from 12 to 20 breaths per minute7,32. Although this change has been identified in only 4% of the sample, a statistical association was observed in this study between it and the income (p=0.034). It is believed that the relationship between them has the same reasons for the relationship between the association between dyspnea and income.
Finally, the less frequent changes in the research were the B3 heart sound, present in 3% of the sample. This sound is produced as a result of decreased ventricular compliance and may be associated with fluid accumulation, as in the case of chronic renal patients. In children and young people, it can be considered physiological, but it is commonly auscultated in patients with cardiac disorders such as heart failure7.
CONCLUSION
It was concluded that most of the interviewed patients are women, with an average age over 50, family income nearly three times the minimum wage and corresponding education to elementary education. Regarding the amount of treatment time, there was a variation of one month to 276 months, with respect to time with renal disease, this varied from one month to 552 months.
Among the prevalent manifestations, those related to the cardiovascular system to the detriment of the lung were highlighted, namely edema, change in blood pressure, central venous pressure and positive hepatojugular reflux. These events are directly related to blood volume changes identified commonly in chronic renal patients. Therefore, most of the problems encountered are the result of excess fluid, responsible for serious heart problems and lung and/or are the precursor agent of the development of some cardiovascular and pulmonary diseases, such as heart failure and pulmonary edema respectively.
When performing the statistical association between socio-economic data and signs and cardiovascular and pulmonary symptoms, only two characteristics were significantly associated: dyspnea and changes in breathing patterns, both associated with family income. However, when seeking the available literature, there were no such results to make a comparative analysis.
Thus, from the study, it was identified that the development of cardiovascular and pulmonary disorders are frequent in the searched individuals. Moreover, these problems are responsible for complications often severe and even fatal if proper care is not readily implemented. Thus, there is the need to focus on these problems, to alert health professionals, especially nurses, as deal daily with these patients, so that they can identify the occurrence of early and better intervention.
REFERENCES
1.IBGE – Brazilian Institute of Geography and Statistics. Estimates of resident population in Brazil and Brazilian states with reference date on 1 July 2012. [cited on September 10 2015]. Available on: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2012/estimativa_tcu.shtm
2. Brazilian Society of Nephrology. Dialysis Census; 2013. Available on: http://sbn.org.br/pdf/censo_2013_publico_leigo.pdf
3.Hussain JA, Russon L. Supportive and palliative care for people with end-stage renal disease. Br J Hosp Med. 2012;73(11):640-4.
4.Roso CC, Beuter M, Jacobi CS, Pauletto MR, Timm AMB, Silva CT. Taking care of yourself: limits and possibilities in the conservative treatment of chronic renal failure. Rev enferm UFPE online. 2015;9(2):617-23.
5. Vieira ODC, Moura SRB, Pinheiro JP, Silva AC, Landim AFLP5, Martins MCC. The Scientific literature on patient quality of life with renal failure undergoing hemodialysis. Rev pesqui cuid fundam(online) [Internet]. 2013 [cited onMarch 10 2015]; 5(6): 338-47. Available on: http://www.seer.unirio.br/index.php/cuidadofundamental/article/view/3488
6.Cavalcante MCV, Lamy ZC, Lamy Filho F, França AKTC, Santos AM, Thomaz EBAF, et al. Factors associated with adult quality of life in hemodialysis in a city of northeastern Brazil. J Bras Nefrol. 2013;35(2):79-86.
7.Smeltzer SC, Bare BG, Brenda G, Hinkle JL, Cheever, KH. Brunner & Suddarth: treated in medical-surgical nursing. 12ª ed. Rio de Janeiro: Grupo Editorial Nacional Participações S/A (GEN); 2011.
8.Karkar A, Modalities of Hemodialysis: Quality Improvement. SaudiJ Kidney Dis Transpl. 2012;23(6):1145-61.
9.Vibhu D, Venkatesh A, Kunal M, Pranav D, Prasad B, Smrita D. Isolated pleural effusion as a presentation of high cardiac output heart failure in a hemodialysis patient. Hemodial Int. 2012; 16:54-7.
10. Selem SSAC, Castro MA, César CLG2, Marchioni DML, Fisberg RM. The validity of self-reported hypertension is associated with Conversely Education in a Brazilian population. Arq Bras Cardiol. 2013;100(1):52-9.
11.Safa J, Noshad H, Ansarin K, Nikzad A, Saleh P, Ranjbar A. Effect of Hemodialysis on Pulmonary Function Tests and PlasmaEndothelin Levels. Saudi J Kidney Dis Transpl. 2014;25(4):781-7.
12.Rahgoshai R, Rahgoshai R, Khosraviani A, Nasiri AA, Solouki M. Acute effects of hemodialysis on pulmonary function in patients with the end-stage renal disease. Iran J Kidney Dis. 2010; 4(3):214-7.
13.Zoccali C, Tripepi C, Torino C, Bellantoni M, Tripepi G, Mallamaci F. Lung congestion as a risk factor for end-stage renal disease.Blood Purif. 2013;36:184-91.
14.Lordsleem A, Gueiros APS, Gueiros JEB, Markman Filho B, Victor EG. Cardiologic evaluation of patients with chronic kidney disease: what are the lessons? J. Bras. Nefrol., 2012;34(1):8-15.
15.Lopes FM, Ferreira JR, Gusmao-Flores D. Impact of renal replacement therapy on lung function in patients on mechanical ventilation. Rev Bras Ter Intensiva. 2013;25(3):251-7.
16.Xavier BLS, Santos I, Almeida RF, Clos AC, Santos MT. Individual and clinical characteristics of patients with chronic kidney disease on renal replacement therapy. Rev enferm UERJ. 2014; 22:314-20.
17.Sousa MNA, Sarmento TC, Alchieri JC. A quantitative study on the quality of life for hemodialysis patients of Paraíba, Brazil. Revista CES Psicología. 2011;4(2):1-14.
18.Frazão CMFQ, Sá JD, Medeiros ABA, Fernandes MICD, Lira ALBC, Lopes MVO. Adaptive problems of hemodialysis patients: socioeconomic and clinical aspects. Rev Latino-Am Enfermagem. 2014;22(6):966-72.
19.Frazão CMFQ, Fernandes MICD, Nunes MGM, Sá JD, Lopes MVO, Lira ALBC. Components of the theoretical model of Roy in patients undergoing hemodialysis. Rev Gaúcha Enferm. 2013;34(4):45-52.
20.Cheng HWB, Sham MK, Chan KY, Li CW, Au HY, Yip T. Combination therapy with low-dose metolazone and furosemide: a ''needleless'' approach in managing refractory fluid overload in elderly renal failure patients under palliative care. Int Urol Nephrol, 2014; 46:1809–13.
21.Shlipak MG, Lash JP, Yang W, Teal V, Keane M, Cappola T, Keller C, et al. Symptoms characteristic of heart failure among CKD patients without diagnosed heart failure (2011). J Card Fail. 2011;17(1):17-23.
22.Barbosa CP, Stefanini FR, Penha F, Góes MA, Draibe SA, Canziani ME, Paranhos Junior A. Intraocular pressure and ocular perfusion during hemodialysis. Arq. Bras. Oftalmol.[online]. 2011;74(2):106-9.[citado em 10 mar 2015]. Disponível em: http://www.scielo.br/scielo.php?pid=S0004-27492011000200007&script=sci_arttext
23. Cerqueira DP, TavaresJR, Machado RC. Predictive factors of renal failure and control algorithm and treatment. Rev Latino-Am Enfermagem. 2014;22(2):211-7.
24.Martins QCS, Aliti GB, Linhares JC, Rabelo ER. Excessive fluid volume: clinical validation in patients with decompensates heart failure. Rev Latino-Am Enfermagem [Internet]. 2011:19(3):[08 telas].[cited on 15 set 2015]. Available on: http://www.scielo.br/pdf/rlae/v19n3/pt_13.pdf
25.Vecchis R, Ciccarelli A, Ariano C. Collapsibility of the Inferior Vena Cava and Signs and Symptoms of Heart Failure. New Insights and Possible Associations. Arq Bras Cardiol. 2012;98(6):544-52.
26.Martínez-Gallardo R, Ferreira-Morong F, García-Pino G, Cerezo-Arias I, Hernández-Gallego R, Caravaca F. Heart failure in advanced chronic kidney disease: relationship to vascular access. Revista Nefrología. 2012; 32(2):206-12.
27.AlitiaGB, LinharesJCC,LinchGFC, RuschelKB, RabeloER. Signs and symptoms of patients with decompensated heart failure: inference priority nursing diagnoses. Rev Gaúcha Enferm.2011;32(3):590-5.
28.Palamidas AF et al. Impact of hemodialysis on dyspnea and lung function in endstage kidney disease patients. Biomed Res Int. 2014;1-10.
29.Frazao CMFQ, Ramos VP, Lira ALBC. The quality of life in patients undergoing hemodialysis. Rev enferm. UERJ. 2011;19(4):577-82.
30.Potechin R, AmjadiK, SrourN. Indwelling pleural catheters for pleural effusions associated with end-stage renal disease: a case series. Ther Adv Respir Dis. 2015;9(1): 22-7.
31.Clark AL, Cleland JGF. Causes and treatment of edema in patients with heart failure. Nat. Rev. Cardiol. 2013;10:156–70.
32.AndradeLZC, SilvaVM, LopesMVO, ChavesDBR, TávoraRCO. Ineffective airway clearance: prevalence and spectrum of its clinical indicators. Acta Paul Enferm. 2014;27(4):319-25.