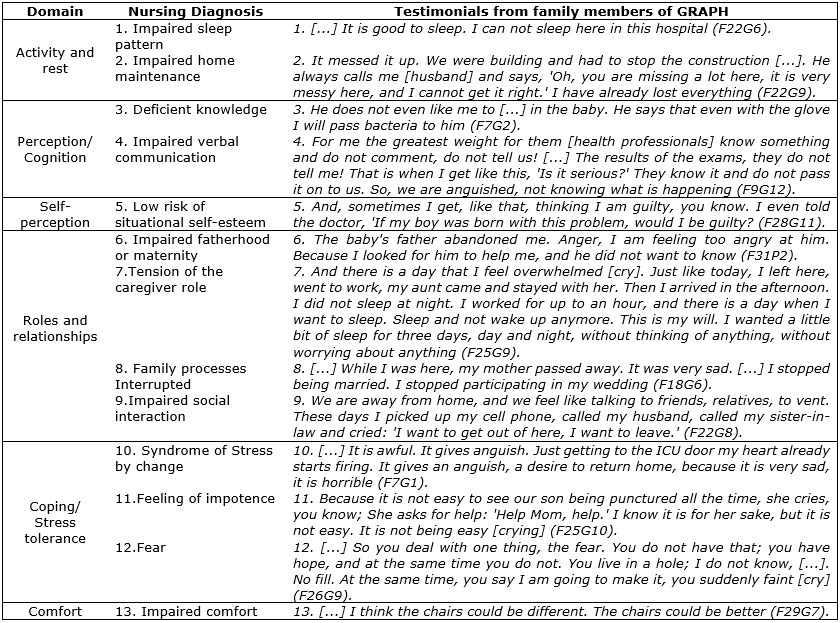
FIGURE 1: Nursing diagnoses and respective domains, identified in the statements of the family members who participated in the (GRAPF).Goiânia, Goiás, Brazil, 2015.
ORIGINAL RESEARCH
Nursing diagnoses and interventions in families of hospitalized children
Leidiene Ferreira SantosI; Lizete Malagoni de Almeida Cavalcante OliveiraII; Selma Rodrigues Alves MontefuscoIII; Maria Alves BarbosaIV
I
Nurse. Ph.D. Assistant Professor, Federal University of Tocantins. Palmas,
Brazil. E-mail: leidienesantos@uft.edu.br
II
Nurse. Ph.D. Professor, Federal University of Goiás. Goiânia, Brazil.
E-mail: lizete@ufg.br
III
Nurse. Ph.D. Assistant Professor, Federal University of Goiás. Goiânia,
Brazil. E-mail: sramontefusco@gmail.com
IV
Nurse. Ph.D. Professor, Federal University of Goiás. Goiânia, Brazil.
E-mail: maria.malves@gmail.com
VResearch developed by the Center for Nursing Research in Management,
People Development and Group Technology in the Context of Health Work
(NEPEGETS), Nursing School, Federal University of Goiás.
DOI: http://dx.doi.org/10.12957/reuerj.2016.8253
ABSTRACT
Objective: to identify the main nursing diagnoses (ND) in families of hospitalized children and describe nursing interventions (NI) in a support group for parents and relatives (SGPR). Method: this quantitative and qualitative descriptive study, conducted in the pediatric ward of a teaching hospital in Goiânia, Goiás, Brazil, collected data from February to July 2010, by recording and transcribing 12 meetings of a SGPR. The study was approved by the ethics committee (Protocol 153/2009). Results: The NDs identified were: impaired sleep pattern; impaired housekeeping; lack of knowledge; impaired verbal communication; risk of low situational self-esteem; mothering or fathering impaired; caregiver role strain; family processes interrupted; impaired social interaction; change-related stress syndrome; and feelings of helplessness, fear and discomfort; and two NIs: increased socialization; and education for health. Conclusion: Families of hospitalized children need to receive information and emotional support from health personnel.
Keywords: Nursing; family health; nursing diagnosis; hospitalized child.
INTRODUCTION
In the last decades, the number of research that deal with the topic of families and the emergence and chronification of diseases has been expanded, corroborating a better understanding the complex the experience of having and living with the sick loved one1.
In the pediatric area, it is seen that the hospitalization of the child significantly interferes with family dynamics, physical and mental health and maintenance of the social network of the people involved in this process2,3.
However, authors suggest that many health professionals still do not include families in their workplace and perform fragmented and biological assistance, with the sole goal of controlling the disease. Psychosocial and cultural aspects involved in the caring process are not always considered, and there is an impairment in communication and interaction between families and health staff4,5.
It should be emphasized that, although it is common and frequent, the suffering of families should not be considered normal and expected in the hospital context. Thus, it is necessary for health professionals to reflect on the practice and to feel restless and uncomfortable with this situation, to the point of being compelled to implement care strategies aimed at the inclusion of families to contribute minimizing possible traumas and reducing sources of suffering, anxiety, and stress6,7.
In this sense, studies with families can contribute to qualify and humanize the care provided by health professionals, and they are fundamental to produce evidence that, in some way, allows changes in the way of perceiving and attending to the needs of families and hospitalized children8,9.
Also, knowing the demands of care allows the health team to implement interventions that qualify and humanize family care, helping them overcome sources of distress and stress, and enabling the transformation of professional practice to avoid fragmentation of care4,10.
Thus, it was aimed to identify the main nursing diagnoses (ND) in families of hospitalized children and to describe the nursing interventions (NI) in a parent and family support group (GRAPF) of these children.
ND and NI are part of the nursing process (NP), a strategy organized in five correlated, interdependent and recurrent stages: data collection, ND, planning, implementation, and evaluation11. The NP corroborates the quality of the information obtained and the use of critical thinking and clinical reasoning, favoring satisfactory care and efficiency of nursing care12,13. In this way, the results of this research can collaborate to give visibility to the assistance to the families and the activities able to contribute to making the integral and humanized care, in the hospital environment.
THEORETICAL-METHODOLOGY REFERENCE
This is a descriptive and quantitative-qualitative study carried out in the pediatric hospitalization unit (PHU) of a highly complex school hospital located in Goiânia, Goiás, Brazil, from February to July 2010. The PHU has two blocks of hospitalizations, the pediatric clinic (PC) and the neonatal intensive care unit (NICU). The PC has 20 beds, on average 12 daily occupancies. The NICU has 10 beds destined to the care of serious newborns and usually with the total occupation.
The testimonies of 12 meetings of a support group for parents and relatives (GRAPF) of the children hospitalized in the PHU were recorded on digital media to collect data. At the end of each meeting, the recordings were transcribed by two researchers, GRAPF coordinating nurses, and analyzed with the objective of identifying the NDs, according to the North American Nursing Diagnosis Association International (NANDA-I) taxonomy 14, and to plan the NI to be implemented in the group, according to the Nursing Interventions Classification (NIC) taxonomy 15.
It should be noted that data collection, material content analysis, identification of NDs and selection and implementation of NI were supported by Wanda de Aguiar Horta's Theory of Basic Human Needs, in which nursing is conceived as a science and an art that must respect and maintain the uniqueness, authenticity, and individuality of the human being, carry out preventive, curative and rehabilitative actions, and recognize the human being as a member of a family and a community and an active participant in the process of self-care16.
To identify NDs, the GRAPF coordinators performed the diagnostic reasoning, which is gradual, interactive and intuitive. It is worth mentioning that the recognition of the evidence, the mental generation of the possible diagnoses, the comparison of the evidence, the data collection of the focused client and the validation of the diagnoses were part of this process, as recommended by specialized literature16-18.
NDs of NANDA-I are distributed in 13 domains: health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, roles and relationships, sexuality, coping/stress tolerance, safety/security, comfort and growth/development. They represent clinical judgments about individual, family, or community responses to health needs. NDs provide the basis for NI selection and the achievement of results for which nurses are responsible14.
In response to the identified NDs, NI was planned and implemented in GRAPF. The NI is understood as actions that, based on judgment and clinical knowledge, are performed to intensify patient/client outcomes. They include both direct and indirect assistance, assistance to individuals, families and the community15.
In the NIC, there are 514 interventions validated and codified directed to ND of NANDA-I, and more than 12 thousand activities. The interventions are grouped into 30 classes and in the basic physiological, physiological complex, behavioral, safety, family, health system and community domains15.
In this research, the selection and implementation of NI were performed by the GRAPF coordinators and were supervised by two nurses, a dynamics group expert and another with experience in caring for the relatives of people hospitalized in an intensive care unit to favor the activities developed in the GRAPF respected the group movement and effectively meet the demands of families, as recommended by specialized literature19-21.
There were 34 family members accepted to be part of the research and met the following inclusion criteria: being 18 years old or older and belonging to the family of a hospitalized child at the investigated PHU during the period of data collection. The number of individuals in each session varied from three to seven, with an average of four per meeting. The participants were mainly mothers (23; 67.6%), uncles (5; 14.7%), grandparents (4; 11.8%) and parents (2; 5.9%) of the children.
The relatives were identified by the letter F and the numerical Alpha system, and by the letter, G accompanied by the number of the meeting in which the family member was present to ensure the identity secrecy and to avoid exposure and embarrassment, in the presentation of the results.
The identified NDs and their respective domains were supported by statements from the families that participated in GRAPF to present the results, and for the selected NI the activities developed in the GRAPF were described.
This research was elaborated and developed following the recommendations of Resolution 466/2012 of the National Health Council and was approved by the Committee on Ethics in Human Research (Protocol 153/2009).
RESULTS
The main ND identified in the speeches of the families that participated in GRAPF were: impaired sleep pattern; Impaired home maintenance; poor knowledge; impaired verbal communication; risk of low situational self-esteem; paternity or impaired motherhood; caregiver role tension; impaired social interaction; stress-for-change syndrome; feeling of helplessness; fear and impaired comfort. They highlight the care needs of families in the context of pediatric hospitalization and how health care behaviors can positively or negatively influence the experiences of families and children.
See Figure 1.
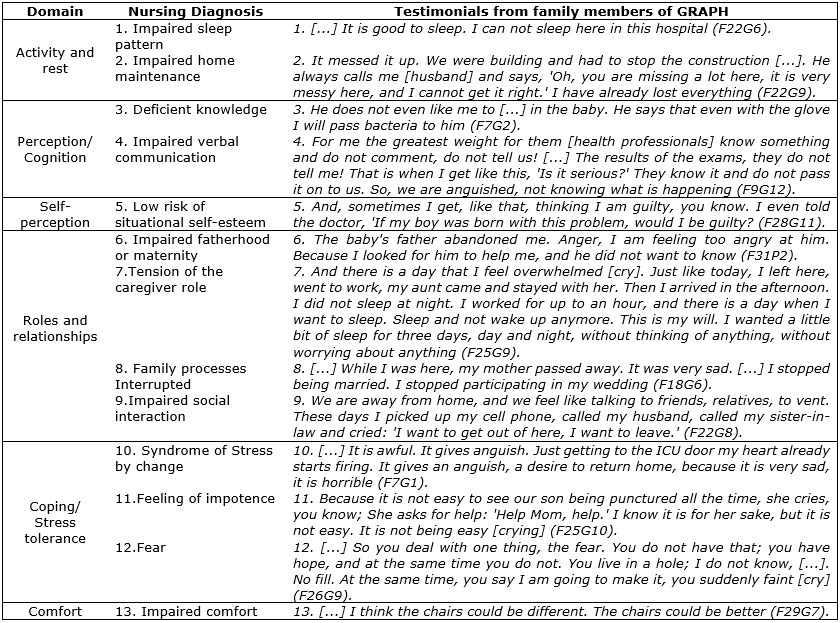
FIGURE 1: Nursing diagnoses and respective domains, identified in the statements of
the family members who participated in the (GRAPF).Goiânia, Goiás, Brazil,
2015.
Here, in response to ND, two NIs were selected, increased socialization and health education. For the first NI, activities were implemented aimed at sharing experiences, demonstrating feelings and increasing communication. For the second NI, the following items were used: family dynamics, visiting times, pathophysiological process, dietary restrictions, hospital unit routines and infection prevention, vaccines and the importance of the affective bond between family and child.
See Figure 2.
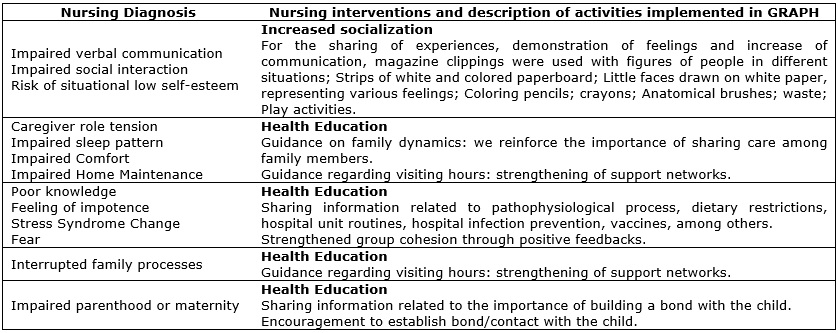
FIGURE 2: Nursing interventions and description of activities implemented in GRAPH
in response to the nursing diagnosis. Goiânia, Goiás, Brazil, 2015.
DISCUSSION
As an integral part of the universe, the human being is subject to states of equilibrium and imbalance in time and space, and their basic needs must be met for the full reach of well-being.16
In this perspective, it is emphasized that families have demands for care, imposed by the process of illness and hospitalization of the child, especially related to physiological aspects3 and psychosocial support7.
The long periods of hospitalization of the child; the rest impaired as a result of the concern, the responsibilities assumed in this process, the noise caused by other relatives and the health team; financial difficulties; the collection of care for the child, even when the family member is unable to do so; the concern about the risk of the child acquiring hospital infection and the possible sequelae due to the procedures and the disease; and the lack of knowledge about necessary and specific care for the child are examples of factors that cause physical and emotional exhaustion to the family6,7.
The ND of tension of the caregiver role, impaired verbal communication, interrupted family processes and impaired home maintenance can be identified in relatives of hospitalized subjects for treatment of chronic non-communicable diseases20. These findings corroborated the ND identified in this study and demonstrated the effects of hospitalization on the family.
Thus, it is important for health professionals to consider the demands of these people and to include them in the care plan1,10, given that unmet needs or inadequate care can cause discomfort and may even lead to the emergence of diseases16.
As interventions aimed at the humanized care of the families, in the context of pediatric hospitalization, it is suggested therapeutic communication, qualified listening, socialization activities, and education and health promotion5.
However, current research shows that health teams still face difficulties in dealing with and caring for these people in the hospital context 6,21,22. Many professionals still cannot grasp the importance and significance of care for the family and the relevance of the changes generated by their inclusion in care and hospitalization, nor they reorganize their work process in the face of expanding their care object. At the same time, it is observed a practice that corroborates a biomedical model, centered on procedures and based on control and power, which leads to a technicist and fragmented assistance21.
Also, the lack of approach and interaction between professionals and family, even experiencing moments of dissatisfaction, makes the family cancel and subjected to the conditions established by the hospital routine and the health team, as it fears to be punished with lack of care to the child. This situation generates discomfort and makes the family's hospital stay an exhausting experience7.
In this way, the health team urgently needs to establish a dialogical relationship with family members, since this behavior contributes to mutual respect, empathy, and acceptance, and demonstrates the care and hospitality of the family, helping to overcome impersonal, fragmented and inhumanity care5,21,23. It should also be noted that to take care of the family, it is necessary to consider what it says, feels and thinks 24.
In this perspective, nursing interventions should be directed to the real demands of the families, aiming to make the child's illness and hospitalization a less traumatic and stressful experience10,25, preventing and reversing imbalances, through assistance to the human being directed to the care of their basic needs16.
Strategies, such as group care, in which there is the promotion of socialization, sharing of feelings and experiences, and stimulating the integration between people, help the family in the process of coping with the disease and experiencing the hospitalization of a loved one so less traumatic.
Effective communication is also described as a resource that enables health professionals to understand and meet the real needs of parents and the child, contributing to the family-centered care and positive health outcomes8,21. In the context of the humanization of care, it is the responsibility of the health professional to provide information and emotional support to the family, so there is a strength to overcome the experience of having and living with a child suffering from illness and hospitalization6,26. In this way, the health team must commit to providing moments of their day to listen to the grievances and difficulties of the family, as well as offering training in child care4,7.
It is indicated the use of activities of education and health promotion to take care of the family, favoring the reception of the family and the child in the hospital context, contributing to maintain the strength and the hope among the people, providing space and the environment conducive to learning and the sharing of information, and constituting a network of support among health professionals and patients27.
A family is a complex unit with diverse needs, interests, contradictions and with a strong influence on health behaviors5,20. Therefore, the health team should establish a cordial and empathetic relationship with this patient, since it is difficult to deal with the child's suffering and with their suffering, requiring support to experience and overcome difficulties2,23.
The interaction and the building of affective bond corroborate the provision of nursing care with the potential to reduce traumas generated by hospitalization4.
CONCLUSION
The ND and NI survey based on the Basic Human Needs Theories showed to be an effective, qualified and safe strategy to describe the real demands of the families and to favor the implementation of activities capable of fully caring for this patient.
The ND identified in this research indicate that when experiencing the situation of having and living with a sick and hospitalized child, families present several demands, such as receiving information about the child's diagnosis and clinical condition, maintaining dialogue and interacting with the health, and receiving support from family and friends.
The selected NIs show that it is possible for the health team to implement activities capable of hosting the family and to make the hospitalization experience of the child, less traumatic and stressful.
It is suggested that undergraduate courses in the health area include the study of family care in the curriculum, enabling students to work with family members who experience situations of pain, suffering, and illness. It is necessary to equip them for the humanized care of the families, in the hospital environment, so that they can understand the importance of including the family in the care plan.
Entering the life of the family, as a person who lives the experience and not only as a spectator, leads the professional to understand the true impact of the disease on the family dynamics and sensitize him to value human experiences and to have compassion for the pain of the other, strengthening his commitment to social responsibility and the humanization of care.
The limitation of this research is the fact that it was not possible to assess the impact of NI on families, especially for the rotation of the GRAPF participants.
REFERENCES
1.Khangura SD, Karaceper MD, Trakadis Y, Mitchell JJ, Chakraborty P, Tingley K et al. Scoping review of patient- and family-oriented outcomes and measures for chronic pediatric disease. BMC Pediatr. 2015; 15(9):1-9.
2.Colesante MFL, Gomes IP, Morais JD, Collet N. Impacto na vida de mães cuidadoras de crianças com doença crônica. Rev enferm UERJ. 2015; 23(4):501-6.
3.MoraisRCM, Souza TV, Oliveira ICS. A (in)satisfação dos acompanhantes acerca da sua condição de permanência na enfermaria pediátrica. Esc Anna Nery. 2015; 19(3):401-8.
4.Gomes GC, Xavier DM, Pintanel AC, Farias DHR, Lunardi VL, Aquino DR. Meanings attributed by family members in pediatrics regarding their interactions with nursing professionals. Rev Esc Enferm USP. 2015; 49(6):953-9.
5.Santos LF, Oliveira LMAC, Munari DB, Barbosa MA, Peixoto MKAV, Nogueira ALG. When the communication is harmful in the encounter between health professional and family of hospitalized child. Enferm. glob. 2015; 14(37):192-203.
6.Gomes GC, Erdmann AL, Oliveira PK, Xavier DM, Santos SSC, Farias DHR. A família durante a internação hospitalar da criança: contribuições para a enfermagem. Esc Anna Nery. 2014; 18(2):234-240.
7.Santos LF, Oliveira LMAC, Barbosa MA, Siqueira KM, Peixoto MKAV. Reflexos da hospitalização da criança na vida do familiar acompanhante. Rev Bras Enferm. 2013; 66(4):473-8.
8.Foster M, Whitehead L, Maybee P. The Parents', Hospitalized Child's, and Health Care Providers' Perceptions and Experiences of Family-Centered Care Within a Pediatric Critical Care Setting: A Synthesis of Quantitative Research. J Fam Nurs. 2015; 1(1):1-67.
9.Wells N, Bronheim S, Zyzanski S, Hoover C. Psychometric Evaluation of a Consumer-Developed Family-Centered Care Assessment Tool. Matern Child Health J. 2015; 19:1899–1909.
10.Seliner B, Wattinger A, Spirig R. Erfahrungen und Bedürfnisse von Eltern hospitalisierter Kinder mit Behinderung und den in der Betreuung verantwortlichen medizinischen Fachpersonen – Eine systematische Review. Pflege. 2015; 28(5):263-76.
11.Conselho Federal de Enfermagem (Br). Resolução nº 358/2009: Dispõe sobre a Sistematização da Assistência de Enfermagem e a implementação do processo de enfermagem em ambientes, públicos ou privados, em que ocorre o cuidado profissional de enfermagem, e dá outras providências. Brasília (DF): Conselho Federal de Enfermagem; 2009.
12.Furtado LG, Nóbrega MML. Modelo de atenção crônica: inserção de uma teoria de enfermagem. Texto Contexto Enferm. 2013; 22(4):1197-204.
13.Leon PAP, Nóbrega MML. NANDA-I nursing diagnosis in hospitalized children: a case study. Online Brazilian Journal of Nursing. 2012;11(1).
14.North American Nursing Diagnosis Association. Diagnóstico de enfermagem da NANDA: definições e classificação 2012-2014. Porto Alegre (RS): Artmed; 2013.
15.Dochterman J, McCloskey B, Glória M. Classificação das intervenções de enfermagem (NIC). Trad. Regina Machado Garcez. 4th ed. Porto Alegre (RS): Artmed; 2008.
16.Horta WA. Processo de enfermagem. São Paulo: EPU; 1979.
17.Risner PB. Diagnosis: analysis and synthesis of data. In: Griffith-Kenney JW, Christensen PJ, organizadoras. Nursing process application of theories, frameworks, and models. 2nd ed. Saint Louis (MO): Mosby; 1986. p.124-51.
18.Rocha LA, Maia TF, Silva LF. Diagnósticos de enfermagem em pacientes submetidos à cirurgia cardíaca. Rev Bras Enferm. 2006; 59(3):321-6.
19.Oliveira LMAC, Santos LF. Trabalhando com grupos na assistência a familiares em UTI. Curitiba (PR): Appris; 2015.
20.Montefusco SRA, Bachion MM, Nakatani AYK. Avaliação de famílias no contexto hospitalar: uma aproximação entre o Modelo Calgary e a taxonomia da NANDA. Texto Contexto Enferm. 2008; 17(1):72-80.
21.Corrêa AR, Andrade AC, Manzo BF, Couto DL, Duarte ED. The family-centered care practices in newborn unit nursing perspective. Esc Anna Nery. 2015; 19(4):629-34.
22.Machado NA, SousaMLXF, Silva MEA, Coutinho SED, Reichert APS, Collet N. Dificuldades para a efetivação do acolhimento hospitalar durante a internação de crianças com doença crônica. Rev enferm UERJ. 2015; 23(4):556-61.
23.Okido ACC, Zago MMF, Lima RAG. Care for technology dependent children and their relationship with the health care systems. Rev Latino-Am Enfermagem. 2015; 23(2):291-8.
24.Silva TP, Silva MM, Alcantara LM, IR Silva, Leite JL. Establishing action/interaction strategies for care delivery to hospitalized children with chronic conditions. Esc Anna Nery. 2015; 19(2):279-85.
25.Craig JW, Glick C, R Phillips, Hall SL, Smith J, Browne J. Recommendations for involving the family in developmental care of the NICU baby. J Perinatol. 2015; 35(Suppl 1):5-8.
26.Svavarsdottir EK, Siqurdardottir AO. Benefits of a brief therapeutic conversation intervention for families of children and adolescents in active cancer treatment. Oncol Nurs Forum. 2013; 40(5):E346-E57.
27.Santos LF, Oliveira LMAC, Munari DB, Peixoto MKAV, Silva CC, Ferreira ACM et al. Grupo de suporte como estratégia para assistência de enfermagem à família de recém-nascidos hospitalizados. Rev Eletr Enf. 2012; 14(1):42-9.