RESEARCH ARTICLES
Prevalence of common mental disorders among health professionals
Ana Paula AlvesI; Leila Aparecida Kauchakje PedrosaII ; Marli Aparecida Reis CoimbraIII ; Mário Alfredo Silveira MiranziIV; Vanderlei José HassV
I
Nurse. Master in Health Care, Federal University of Triangulo Mineiro. Uberaba, Minas Gerais, Brazil. Email: apaula.alv@gmail.com
II
Nurse. PhD in Public Health. Professor at the Federal University of Triangulo Mineiro. Postgraduate Program in Health Care. Uberaba, Minas Gerais, Brazil.
Email: leila.kauchakje@terra.com.br
III
Nurse. Master in Health Care, Federal University of Triangulo Mineiro. Uberaba, Minas Gerais, Brazil. Email: marli.apr.coimbra@gmail.com
IV Dentist. PhD in Public Health. Professor at the Federal University of Triangulo Mineiro. Uberaba, Minas Gerais, Brazil.Email: mmiranzi@mednet.com.br
V
Physicist. PhD in Physics Applied to Medicine and Biology. Professor at the Federal University of Triangulo Mineiro. Postgraduate Program in Health Care.
Uberaba, Minas Gerais, Brazil. Email: vjhaas@uol.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2015.8150
ABSTRACT
This study aimed at assessing the prevalence of common mental disorders (CMD) among health professionals of a teaching hospital. It is a quantitative cross-sectional observational study conducted with 359 health professionals, at Hospital de Clínicas da Universidade Federal do Triângulo Mineiro, Minas Gerais, Brazil. Data collection occurred from June to August, 2013. Participants answered both an instrument with professional and social and demographic variables and another one for assessing the prevalence of CMD - the Self Reporting Questionnaire. Among those health professionals, an overall 27.9% prevalence for CMD was observed. Results identified CMD. It is therefore necessary to propose health promotion measures for health professionals. Keywords: Health personnel; SRQ-20; worker's health; mental disorders.
INTRODUCTION
The exercise of professional activity permeates physical, social and emotional dimensions that are favorable to mental balance, contentment and development of capabilities, but it can also be the cause of suffering and exhaustion which in turn lead to the change of individuals' health status1,2.
Health professionals have numerous stressful situations in clinical practice, because they are frequently exposed to one or more elements that favor the onset of disease or suffering, which are highlighted by organic and psychological signs and symptoms such as mental disorders, and these factors adversely affect the results of the work and the quality of care offered by workers1,3,4.
Common mental disorders (CMD) are the non-psychotic symptoms characterized by somatic complaints, insomnia, queasiness, decreased concentration, irritability, fatigue, feeling of worthlessness and headache5. CMD are often found in diverse populations, their presence produces impacts on productive sectors, and can increase the demand for health services5,7.
Brazilian literature about CMD among health professionals is still scarce4. Given the foregoing, there is need for further exploration of the topic, focusing on the various aspects related to mental disorders. This study aims to determine the prevalence of Common Mental Disorders among health professionals and to analyze the relationship between sociodemographic factors and professionals.
LITERATURE REVIEW
Mental disorders constitute 12% of all diseases and disabilities in the world, and a quarter of people will be affected by a mental disorder at some stage of life. Due their chronic nature that produces disability, they are considered a public health problem because they cause stigmas and other problems 8,9.
Mental illnesses have difficult early diagnosis, and may cause psycho-emotional, organic, social and cultural changes. Due to its subjective nature and the social stigma attached to that pathology, this clinical picture results in deficiency in appropriate care to most people with mental distress8.
Symptoms indicating CMD are more common among older people, women, widowers, and are related to events that produce stress, reduction of social support, and variables related to poor living conditions and working conditions, lower income and low education6,9,10.
Epidemiological research on mental health began in hospitals and outpatient services. Due to the need to expand studies on this topic, they have extended the population base, and the results showed that about 90% of psychiatric manifestations consist of nonpsychotic disorders, including depression, anxiety and symptoms such as insomnia, fatigue, stress, memory difficulties and somatic complaints11.
METHODOLOGY
This is an observational, cross-sectional study with a quantitative approach, conducted at the Clinical Hospital of the Federal University of Triangulo Mineiro. The population consisted of health professionals, who were selected using simple random sampling. The calculation of sample size considered a prevalence of 32% for CMD, an accuracy of 3% and a 95% confidence interval, for a finite population of 1138 professionals, reaching the sample of 359 individuals, considering a sampling loss of 20%, the maximum number of interviews attempts was 449. The inclusion criteria adopted for the study were: working as nurse, nursing technician, nursing assistant, physician, psychologist, speech therapist, social worker, occupational therapist or physiotherapist and providing direct care to patient. Workers with less than 30 working days in the institution were excluded. Data collection was conducted from June to August 2013.
This work was based on the Resolution No. 466/12 of the National Health Council of Brazil. The research project was submitted to the Ethics Committee in Research with Human Beings under the 2505 protocol, and the participants signed an Informed Consent Form.
Data collection consisted of applying a socio-demographic and professional form and to analyze the prevalence of CMD the Self Reporting Questionnaire (SRQ-20) was used, which assesses: nonspecific somatic complaints, irritability, insomnia, headaches, fatigue, forgetfulness and difficulty in concentrating.
SRQ-20 is the version of 20 items used for tracking non-psychotic mental disorders, developed by the World Health Organization (WHO)8 and it was validated in Brazil12.
Answers used in the questionnaire are only yes or no and each positive answer corresponds to 1 point to compose the final score by the total sum of these values. Scores obtained are related to the probability of presence of non-psychotic disorders, including depression, anxiety and somatic complaints, ranging from 0, meaning no probability, and 20, meaning extremely likely to have CMD13.
Symptoms were grouped into categories, we used the classification, which sets out four subdivisions of symptoms that are depressive/anxious mood, somatic symptoms, reduction of vital energy and depressive thoughts14.
Data were entered in duplicate in a spreadsheet (Microsoft Office Excel® 2007 program for Windows®) and imported to Statistic Package for Social Sciences (SPSS) version 20.0.
For analysis of qualitative variables descriptive statistics and absolute and percentage frequency were used. Bivariate analysis included measures of association in contingency tables (chi-square, prevalence ratio and prevalence odds ratio). The analysis of risk factors for the occurrence of CMD considered a binary logistic regression model, having as variables sociodemographic and professionals predictors.
RESULTS AND DISCUSSION
Among participants, 18.4% were physicians, 73.8% composed the nursing staff and 7.8% represented other health professionals. There was predominance of female professionals - 77.2%, who claimed to be married or in stable relationships - 56.2% - and that had children - 60.4%.
The mean age of participants was 39.53 years old. The mean age of health professionals in the teaching hospital was close, but higher, to that found in another study 15.
The predominance of women, observed in this study, is consistent with other research conducted with health professionals15-17. The nursing team represented the largest part of the quota, showing that this profession still remains essentially female18-20. Women have a vital role in society, because besides being in the labor market they are sometimes the only providers of the family, adding up to this the fact that domestic work is often performed only by them.
Of all participants, 74.4% had been working for 5 years or more in the institution, 54.9% worked in the day shift, 23.1% performed their activities in the night shift and 22% in more than one shift, with this group represented by medical professionals - 71.2%.
Among the participants, 67.1% had an employment relationship, however, between doctors, 72.7% have more than one. Financial need and the search for better pay motivate professionals to accumulate several jobs, despite the exhausting work routine21. Regarding family income, 50.1% of respondents reported receiving over 2 and up to 6 minimum wages, while 14.2% had a family income of up to 2 minimum wages.
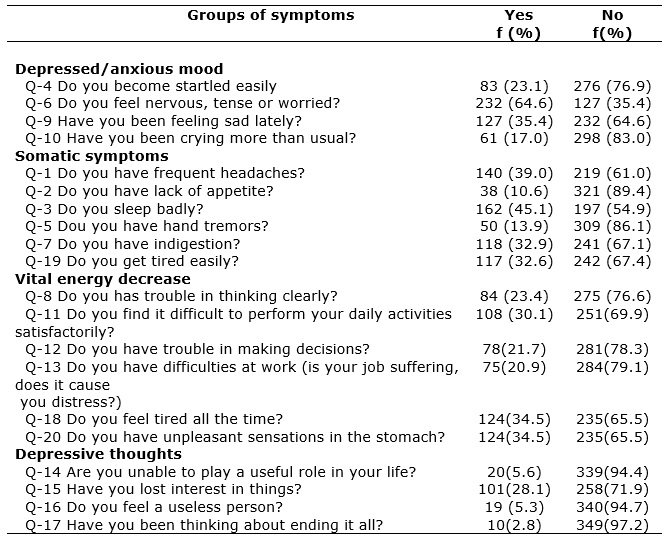
Among the symptoms grouped evaluated through the SRQ-20, there was prevalence of the category of depressive/anxious mood symptoms, especially the complaint of feeling nervous, tense or worried -64.6%, as shown in Table 1. This category of symptoms was also the most prevalent in other studies that used the same screening instrument22,23.
TABLE 1
: Prevalence of groups of mental symptoms in health care workers of a teaching hospital, according to SRQ-20. Uberaba, 2013. (N= 359)
In the group of somatic symptoms, sleeping badly represented 45.1% of the study subjects. The sleep issue was also the most prevalent complaint in the group of somatic symptoms analyzed in another study22, but it presented more frequency than in the present study.
Among health professionals of the present study we found a prevalence of 27.9% of positive screening for CMD. The prevalence was not as high as in an investigation carried out with workers of basic health services in Botucatu, which showed that 42.6% had indicative of CMD24. However, the prevalence was higher than that found in another survey with professionals in Bahia, in which prevalence was 16.0%25. It was expected that the prevalence of CMD was higher in professionals working in the hospital area than in those of primary care due to the different complexities, although studies have shown contradictory results.
The prevalence of CMDs, found in this study, was higher than that identified among workers in Ethiopia, which showed that the presence of CMD reached 17.7% of the population in this country, representing 25.9% in women and 12.4% in men26.
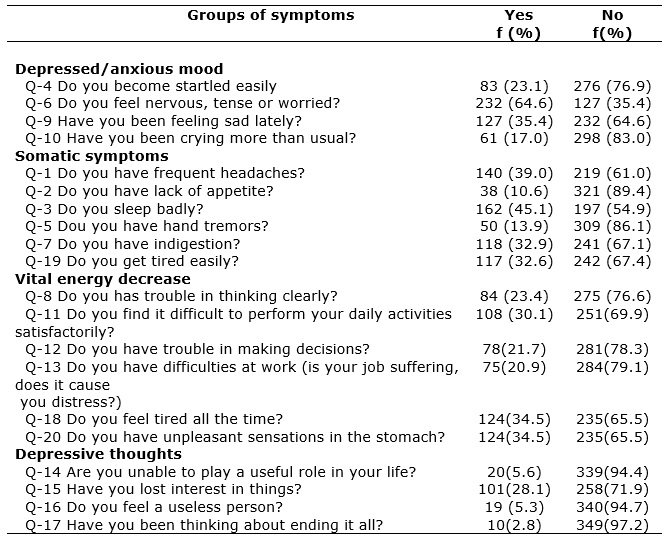
Findings of the bivariate analysis of CMD, according to sociodemographic variables among health professionals, are listed in Table 2.
TABLE 2
: Prevalence of common mental disorders among health professionals in a teaching hospital, according to sociodemographic variables. Uberaba, 2013. (N= 359)
(*)Statistically significant, considering α = 0.05.
The prevalence of CMDs among women was 32.5%, while in males was 12.2%; the prevalence ratio (PR) reached 2.66 (95% CI 1.45 to 4.87), as shown in Table 2.
In bivariate analysis, the association between CMD and family income was statistically significant (p = 0.001), professionals who have income between 1 and 2 minimum wages had twice CMD than those with income greater than 6 minimum wages (PR: 2.39, 95% CI 1.45-3.95), as exposed in Table 2. Prevalence of lower income was 41.2%, while those with earnings above 2 and up to 6 minimum wages reached 31.7% and more than 6 wages was 17.2% of positive screening for CMD.
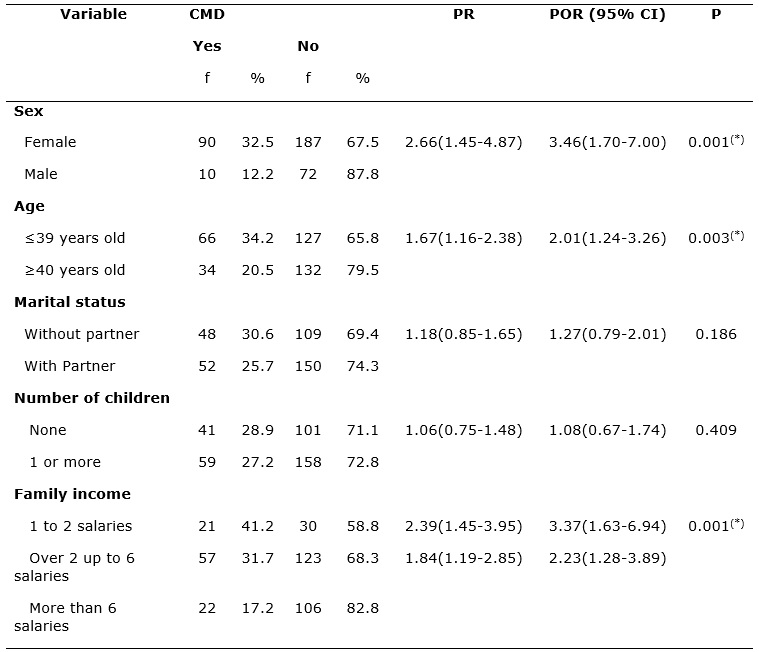
Results of the bivariate analysis of CMD, according to professional variables, are specified in Table 3.
TABLE 3
: Prevalence of common mental disorders among health professionals in a teaching hospital, according to professional variables. Uberaba, 2013. (N= 359)

(*)Statistically significant, considering α = 0.05.
The nursing team showed 33.6% of prevalence for CMD, other professionals - 17.9% and doctors - 9.1%. The prevalence ratio of nursing staff was 3.69 (95% CI 1.69-8.07) compared to physicians, as shown in Table 3.
Regarding the work shift, association of CMD with the night shift was statistically significant (p = 0.003), professionals working at night presented three times more mental disorders than those professionals working in more than one shift (PR: 3.42, 95% CI 1.41-8.26), and 34.9% of professionals working in the night shift demonstrated tendency to CMD.
Logistic regression analysis revealed that among health professionals, women had 2.36 times higher chance (95% CI 1.09-5.10, p = 0.028) to have CMD; and among those under 39 years of age there was 2.21 times higher chance (95% CI 1.31-3.71, p = 0.003) of screening for CMD be positive, even after adjustment of variables identified as potential confounding (professional category, income and work shift).
Regarding age, we found a higher prevalence of CMD in young people, which corroborates other studies12,26,27. However, a survey conducted with members of nursing team showed that older people have a higher frequency of indicative to CMD28.
Prevalence of CMDs was significantly higher in females, a fact also confirmed by several studies conducted in different populations9,10,26-28.
Although the family income variable, after adjustment as a potential confounder, was not statistically significant, it is noteworthy that the lower the income, the greater the presence of CMD, which is mentioned by study conducted in Pernambuco6. The income variable can provide better conditions of life, so people with good financial conditions have lower prevalence of mental disorders, a fact confirmed by other studies27,28.
A study carried out in public hospitals showed higher prevalence of CMD in night shift workers29, with values close to those found in this study. Night work may bring harm to the health of professionals, it is considered something complex and may be associated with individual factors, life conditions and the complexity of labor activity17,18.
Although the professional category has not shown to be statistically significant when adjusted to other variables, using logistic regression, it is necessary to highlight the prevalence for the presence of CMD. Bivariate analysis showed that in the nursing staff the prevalence was 33.6% for CMD, a fact that corroborates other studies involving similar population in which the prevalence ranged from 24.6% to 33.9%27-30. The prevalence of 91% for CMD among physicians was lower than that found in other studies with the same type of population, however, in different scenarios, which showed variation from 17.4% to 68%21,22,24,25.
CONCLUSION
The presence of CMD in the studied population indicates that, due to the subjective nature of non-psychotic disorders, many professionals may be underdiagnosed, and therefore may not be undergoing appropriate treatment. Therefore, it is necessary to propose strategies that can promote workers' health, especially among women, as they showed the highest prevalence of CMD in this study. However, because this is a cross-sectional study, in which there is a limitation of causality, it is emphasized the need for longitudinal studies to examine the influence of considered risk factors.
REFERENCES
1.Dejours C. A loucura do trabalho: estudo de psicopatologia do trabalho. São Paulo: Cortez- Oberé; 1992.
2.Chaves LD, Ramos LH, Figueiredo EN. Satisfação profissional de enfermeiros do trabalho no Brasil. Acta Paul Enferm. 2011; 24: 507-13.
3.Aiken LH, Sloane DM, Clarke S, Poghosyan L, Cho E, You L, Finlayson M, Kanai-Pak M, Aungsuroch Y. Importance of work environments on hospital outcomes in nine countries. Int J Qual Health Care. 2011; 23: 357-64.
4.Tavares JP, Beck CLC, Magnano TSBS, Greco PBT, Prestes FC, Silva RM et al. Produção cientifica sobre os distúrbios psíquicos menores a partir do self report questionnaie. Rev Enferm UFSM. 2011; 1:113-23
5.Goldberg D, Huxley P. Common mental disorders: a bio-social model. London (UK): Tavistock; 1992.
6.Ludermir AB, Melo Filho DA. Condições de vida e estrutura ocupacional associadas a transtornos mentais comuns. Rev Saude Publica. 2002; 36: 213-21.
7.World Health Organization. The World Health Report 2001. Mental Health: new understanding, new hope. Geneva (Swi): WHO; 2001.
8.Prince M, Patel V, Saxena S, Maj M,Maselko J, Phillips MR, Rahman A. No health without mental health. The lancet. 2007; 370: 859-77.
9.Costa AG, Ludermir AB. Transtornos mentais comuns e apoio social: estudo em comunidade rural da Zona da Mata de Pernambuco, Brasil. Cad Saúde Pública. 2005; 21:73-9.
10.Jansen Karen, Mondin TC, Ores LC, Souza LDM, Konradt CE, Pinheiro RT et al. Transtornos mentais comuns e qualidade de vida em jovens: uma amostra populacional de Pelotas, Rio Grande do Sul, Brasil. Cad Saúde Pública. 2011; 27: 440-8.
11.Coutinho ESF, Almeida Filho N, Mari JJ. Fatores de risco para morbidade psiquiátrica menor: resultados de um estudo transversal em três áreas urbanas no Brasil. Rev Psiq Clín. 1999; 26: 246-56.
12.Mari JJ, Williams P. A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of São Paulo. Br J Psychiatry. 1986; 148: 23-6.
13.Goncalves DM, Stein AT, Kapczinski F. Avaliação de desempenho do Self-Reporting Questionnaire como instrumento de rastreamento psiquiátrico: um estudo comparativo com o Structured Clinical Interview for DSM-IV-TR. Cad Saúde Pública. 2008; 24: 380-90.
14.Iacoponi E, Mari JJ. Reability and factor struture of the Portuguese version of Self: reporting questionnaire. Internat J Social Psychiat. 1989; 35: 213-22.
15.Ebling M, Carlotto MS. Burnout syndrome and associated factors among health professionals of a public hospital. Trends Psychiatry Psychother. 2012; 34: 93-100.
16.Mendes SS, Martinho MMF. Trabalho em turnos: estado geral de saúde relacionado ao sono em trabalhadores de enfermagem. Rev Esc de Enferm da USP, 2012; 46:1471-6.
17.Pimenta AM, Kac G, Souza RRC, Ferreira LMBA, Siqueira SMM. Trabalho noturno e risco cardiovascular em funcionários de universidade pública. Rev Assoc Med Bras, 2012; 58:168-77.
18.Silva AA, Rotenberg L, Fischer FM. Jornadas de trabalho na enfermagem: entre necessidades individuais e condições de trabalho. Rev Saude Publica. 2011; 45:1117-26.
19.Silva NS, Esperidião E, Silva KKC, Souza ACS, Calvacante ACG. Perfil profissiográfico de trabalhadores de nível universitário em serviços de saúde mental. Rev enferm UERJ. 2013; 21:185-91.
20.Martins JT, Bobroff MCC,Andrade AN, Menezes GDO. Equipe de enfermagem de emergência: riscos ocupacionais e medidas de autoproteção. Rev enferm UERJ. 2014; 22:334-40
21.Cabana MCFL, Ludermir AB, Silva ÉR, Ferreira MLL, Pinto MER. Transtornos mentais comuns em médicos e seu cotidiano de trabalho. Jornal Bras Psiquiatria. 2007; 56: 33-40.
22.Carvalho CN, Melo-Filho DA, Carvalho JAG, Amorim ACG. Prevalência e fatores associados aos transtornos mentais comuns em residentes médicos e da área multiprofissional. Jor Bras Psiquiatria. 2013; 62: 38-45.
23.Galvão LLLF, Farias MCS, Azevedo PRM, Vilar MJP, Azevedo, GD. Prevalência de transtornos mentais comuns e avaliação da qualidade de vida no climatério. Rev Assoc Med Bras. São Paulo, 2007; 53:414-20.
24.Braga LC, Carvalho LR, Binder MCP. Condições de trabalho e transtornos mentais comuns em trabalhadores da rede básica de saúde de Botucatu (SP). Ciênc saúde coletiva[online]. 2010; [ citado em 20 jul 2014]. 15: 1585-96. Disponível em: http://www.scielo.br/pdf/csc/v15s1/070.pdf
25.Barbosa GB, Correia AKS, Oliveira LMM, Santos VC, Ferreira SMS, Martins JDF. Trabalho e saúde mental dos profissionais da estratégia saúde da família em um município do Estado da Bahia, Brasil. Rev Bras Saúde Ocupacional. 2012; 37: 306-15.
26.Gelaye B,Lemma S, Deyassa N, Bahretibeb Y, Tesfaye M, Berhane Y. Prevalence and Correlates of Mental Distress Among Working Adults in Ethiopia. Clin Pract Epidemiol Ment Health, 2012; 8:126-33.
27.Kirchhof ALC, Magnago TSBS, Camponogara S, Griep RH, Tavares JP, Prestes FC, Paes LG. Condições de trabalho e características sócio-demográficas relacionadas à presença de distúrbios psíquicos menores em trabalhadores de enfermagem. Texto contexto – enferm. 2009; 18:215-23.
28.Pinho PS, Araujo TM. Trabalho de enfermagem em uma unidade de emergência hospitalar e transtornos mentais. Rev enferm UERJ. 2007; 15: 329-36.
29.Diniz TB, Silva-Costa A, Griep RH, Rotenberg L. Minor psychiatric disorders among nursing workers – is there an association with current or former night work? Work 41. 2012; 41: 2887-92.
30.Araújo TM, Aquino E, Menezes G, Santos CO, Aguiar L. Aspectos psicossociais do trabalho e distúrbios psíquicos entre trabalhadoras de enfermagem. Rev Saude Publica. 2003; 37: 424-33.