Source: the study's authors.
ORIGINAL RESEARCH
Chronic renal failure patients' perceptions of the everyday implications of hemodialysis therapy
Simone Guimarães Teixeira SoutoI; Graziela Seixas LimaII; Patrick Leonardo Nogueira da SilvaIII; Ricardo Soares de OliveiraIV; Renata Patrícia Fonseca GonçalvesV; Edna de Freitas Gomes RuasVI
I
Master in Nursing. Professor of the Nursing Department of the State
University of Montes Claros. Montes Claros, Minas Gerais, Brazil. E-mail: simonegts28@yahoo.com.br
II
Professor of the Nursing Department. Faculdades Unidas do Norte de Minas.
Montes Claros, Minas Gerais, Brazil. E-mail: grazylima@yahoo.com.br
III
Master student in Health, Society and Environment. Professor of the Nursing
Department of the State University of Montes Claros. Montes Claros, Minas
Gerais, Brazil. E-mail:
patrick_mocesp70@hotmail.com
IV
Specialist in Cardiology Nursing. Professor of the Nursing Department of
the State University of Montes Claros. Montes Claros, Minas Gerais, Brazil.
E-mail: rsoaresmoc@gmail.com
V
Master in Nursing. PhD student in Nursing. Professor of the Nursing
Department of the State University of Montes Claros. Montes Claros, Minas
Gerais, Brazil. E-mail:
renatapfonseca@yahoo.com.br
VI
Master in Nursing. Professor of the Nursing Department of the State
University of Montes Claros. Montes Claros, Minas Gerais, Brazil. E-mail: efgomesruas@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.8093
ABSTRACT
Objective: to identify chronic renal failure patients' perceptions of the everyday implications of hemodialysis therapy. Methodology: this qualitative, observational, descriptive, cross-sectional study was conducted with 20 patients with chronic renal failure (CRF) in Montes Claros, Minas Gerais, Brazil. Results: the analysis generated the categories: "the influence of hemodialysis on the life of CRF patients", in which adaptation to a new lifestyle affects biopsychosocial factors, and restricts the patient's activities; and "nutritional restrictions: personal and social repercussions for the person with CRF", which is an important factor in treatment efficiency, but leads to social isolation and deprivation of leisure. Conclusion: understanding these changes leads to new strategies to improve the quality of care provided. Therefore, education, "embracement", motivation and including the family/community constitute strategies for strengthening coping with hemodialysis.
Keywords: Chronic renal insufficiency; renal dialysis; hemodialysis hospital units; coping strategies.
INTRODUCTION
Chronic diseases are not defined by their apparent or actual severity, but rather because they have no cure or have very prolonged duration. These include diseases that lead, in a longer or shorter period, to death 1.
In recent years, chronic diseases have received greater attention from health professionals. This is because these diseases have begun to play an important role in pan-population morbidity and mortality and are no longer exclusively of the elderly population, since youngsters of productive age have also been subject to these diseases2.
Chronic kidney disease (CKD) is among the diseases that has grown annually, causing serious public health problems because it has progressive evolution and therefore becomes a condition without alternatives for immediate improvement. According to data from the annual census of the Brazilian Society of Nephrology (SBN), the estimated number of patients undergoing dialysis in 2014 was 112,0043.
CKD is defined by the progressive and irreversible loss of renal function, enabling the patient to perform renal replacement therapy in the form of peritoneal dialysis (PD), hemodialysis or transplantation. Hemodialysis has been the most indicated therapy in recent years, considering that CKD requires rapid intervention due to the difficulty of its diagnosis4.
Thus, this study aimed to identify the perception of the patient with CKD regarding the implications of hemodialysis therapy in their daily lives.
LITERATURE REVIEW
Hemodialysis is defined as a process of artificial blood filtration in relation to accumulated impurities. It is used for patients with end-stage renal failure or acutely ill patients requiring short-term dialysis 5,6.
Hemodialysis can often represent a hope of life for the patient, since the disease is irreversible. However, with adherence to treatment, patients face difficulties in accepting the disease, in social interaction and in dealing with fear of death or incapacity, among others7.
The habitual living standard of the patient with CKD tends to be affected, since an individual who usually have not needed the care of a health team starts to face the reality of needing constant assistance of the multidisciplinary team and of a machine, losing much of their autonomy of life8.
The user of hemodialysis services presents some symptoms that can result in physical limitations and complications at work, which, as a result, may interfere with their standard of living and habitual routine. Technological and therapeutic advances in dialysis have contributed to an increase in the survival of the CKD patient. However, it does not enable them to return to life in relation to qualitative aspects2.
The individual's perception of his or her position in life in the context of culture and value system in which they live in relation to their objectives includes some main domains, such as psychological status, physical health, level of independence, environmental characteristics, social relationship and spiritual pattern9,10.
METHODOLOGY
This is a descriptive, observational and cross-sectional study with a qualitative approach performed with patients diagnosed with CKD undergoing hemodialysis treatment at the Nephrology and Hemodialysis Center (CNH in Portuguese) of a Hospital Foundation located in the city of Montes Claros, Minas Gerais.
The CNH of the city of Montes Claros, Minas Gerais, was inaugurated on October 29, 2007. This institution assists 106 patients registered for hemodialysis. Participants were 20 patients undergoing renal replacement therapy (hemodialysis) who were performing the treatment in the morning and afternoon shifts. Patients accepted to participate voluntarily and were randomly chosen according to the inclusion and exclusion criteria of the research.
Patients who were undergoing hemodialysis treatment and aged between 18 and 65 years were included in the study. Patients who were undergoing other types of dialysis, such as intermittent peritoneal dialysis (IPD), continuous ambulatory peritoneal dialysis (CAPD), continuous cyclic peritoneal dialysis (CCPD), continuous dialysis, among others, and those who were younger than 18 years were excluded from the research.
For the accomplishment of this research, in the first place we sought to acquire a previous knowledge on the subject addressed through the scientific literature. Then, a semi-structured interview script was developed as a data collection tool. An MP3 player was also used to record participants' speeches during the interview and for later transcription in full of the answers collected.
The research was carried out in May 2009 by the researcher in charge, with a previous and anticipated appointment with the nurse of the sector of the hospital. Before starting the data collection procedures, the researcher guided the patients in relation to the purpose of the study, read and presented the Informed Consent Form (ICF) to authorize the interview and the recording of participants' speeches. After the recording, the statements were transcribed in full to ensure the veracity of the information.
Patients were approached at the time they were undergoing hemodialysis treatment. The interviews were carried out individually and, at the first moment, researchers asked questions that could characterize the research subject through information about age, marital status, profession, schooling, among other variables. Then, questions were made related to the interferences of the disease in the daily life of the CKD carrier, the adequacy of these to the diet and the modifications in their social life.
Data collection was completed when the data was saturated, that is, when information began to be repeated.
After the transcription of the statements, the data were analyzed through the content analysis method11, which is defined as a set of communication analysis techniques that uses systematic procedures and objectives to describe the content of the messages. Thus, the contents were categorized and discussed according to the following so-called categories: the influence of hemodialysis on the life of CKD patients; nutritional restrictions: personal and social repercussions for CKD patients.
To maintain the patients' anonymity, they were named by codes, these letters and numbers being A1, A2, A3,..., A20.
This study followed the ethical principles in research with human beings provided for in resolution 196/96 of the National Health Council, in force at the time of the study. It was approved by the Ethics Committee in Research of the Faculdades Unidas do Norte de Minas (CEP/UNORTE), under opinion no. 026/2009, of May 14, 2009.
RESULTS AND DISCUSSION
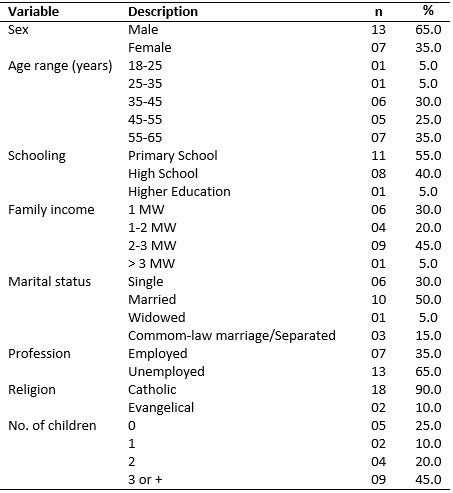
As for the profile of the 20 patients interviewed, they are included in the age group between 18 and 65 years. There was a predominance of males, with 13 (65%) participants, the age range of 55-65 years old (35%), primary education (55%), and family income of two to three minimum wages (45%). It is also verified that 10 (50%) were married, 13 (65%) were unemployed, 18 (90%) claimed to be Catholic and nine (45%) had three or more children, as described in Table 1.
Table 1:
Socioeconomic and demographic profile of participants. Montes Claros, MG,
2014.
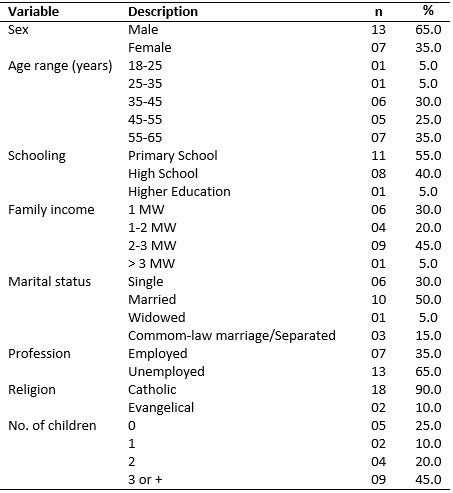
Source: the study's authors.
The influence of hemodialysis on the life of CKD patients
Adapting to a new lifestyle and getting used to the limitations of dialysis treatment can be a difficult issue to address because of several reasons. Many people do not find the right framework to deal with the changes they have acquired over the course of their lives9,12. Of the total number of participants, only six reported being able to deal with CKD and its treatment without many daily changes, despite the various restrictions provided by the disease. This can be proven by the following statements:
Oh, my life has kept normal, apart from the fact we have to come here three times [...], but I can even have a normal life [...]. (A18)
Oh, nothing has changed; almost everything is the same way [...]. (A13)
[...] no, my daily activities have not changed much, [...]. (A3)
[...] well, it has not changed many things, no [...]. (A20)
[...] I have kept doing everything normally [...]. (A12)
No, it has not changed much. I cannot do some things, but I have coped well with these restrictions [...]. (A11)
The present study showed that treatment time has a great influence in adapting to the new way of life. The patients interviewed who have undergone this therapy for more than one year had a higher acceptance rate with CKD than patients with a shorter treatment time. Scientific studies agree with this when reporting that most people who go through unpleasant episodes react with sadness or depressed mood when faced with situations that, due to severity and duration, are greater than their adaptive capacity6,8,13. The following statements confirm this idea.
[...] and it was more difficult earlier, because I used to feel revolted. In the beginning it used to be very depressed, I would not accept it, but today I have already adapted well [...]. (A19, six years on hemodialysis)
[...] these things change our lives too much. I have not adapted until now, because it is too restrictive and I get a little depressed sometimes. (A4, seven months on hemodialysis)
There was also a sense of compulsion in having to accept the treatment in order to be able to survive. Many have reported faith in God as the main factor in gaining the courage to face a condition of life with no other choices. Treatment is necessary and needs to be faced without negotiation.
[...] a lot of things get in the way, it is very painful here, but we have to do it, don't we? Thank God I keep on doing [...]. (A1)
[...] but we have to overcome these problems if we want to live, right? Because it's the machine that makes us alive [...]. (A2)
[...] so, it is difficult to take on this life, we do not accept it much, but God makes us go on [...]. (A7)
The condition of being chronically ill and of underdoing hemodialysis treatment brings several disadvantages since the person is faced with many changes in life. A large majority of respondents reported changes that are often seen as demoralizing, such as loss of employment, financial difficulties, decreased physical activity, partial inability to undertake walks, dietary restrictions, feelings of incapacity and dependence. Another scholar9 follows this line of reasoning and says that insecurity and loss of autonomy lead to disabilities in daily life.
The issue of the impairment of daily activities deserves to be highlighted since the set of some of these activities is source of satisfaction for the individual, according to the particularities of each person. Although some people reported that they have not stopped doing many pre-treatment activities, many said they have not felt able to do them anymore.
I used to play soccer almost every day, but now I have stopped doing it because I'm afraid to hurt myself [...]. (A15)
I used to ride a horse a lot and now I have hardly done that. (A2)
In CKD, the qualitative aspects are impaired by the innumerable losses and changes caused by the imposed therapy. The reality of having to rely on a machine to survive, needing frequent care and consequently having to give up work in favor of treatment brings these people a sense of incapacity within the family nucleus. There is often a reversal of roles in the family. A researcher10 agrees that social role change within the family causes psychological changes due to the various losses deriving from treatment. Of the people interviewed, most have not been working currently. The following statements reveal that one of the greatest lamentations regarding lifestyle change was the renunciation of employment.
My routine has changed a lot, right? I have always worked and cannot work anymore because of the treatment. (A10)
[...] I cannot work anymore. It's what I like to do and I cannot do it anymore. (A2)
[...] oh, working, right? Because I cannot do it anymore because of my hand; I cannot do anything [...]. (A1)
[...] and my job, I had to quit [...]. (A17)
In order to proceed to the dialysis treatment, patients need to maintain care with arteriovenous fistula (AVF), after all it is the venous access that makes possible the treatment, since it is the route that provides the intracorporeal circulation for the accomplishment of the hemodialysis. Self-care actions are the patient's responsibility13. Due to the care of the AVF, people are unable to perform activities that require some type of effort with the anastomosed arm, which implies biopsychosocial changes. There were some reports regarding the impossibility of performing activities related to AVF.
Now I cannot do anything at home, because I cannot pick up weight because of the fistula [...]. (A1)
[...] I cannot clean the house, eat food, wash clothes, because I cannot pick up weight [...], otherwise I lose the fistula [...]. (A17)
[...] I cannot work anymore [...]. I have always worked [...] and I can't anymore because of the fistula [...]. (A2)
Hemodialysis treatment usually occurs three times a week; each session lasts four hours and the person becomes permanently subjected to this treatment14. According to the testimonies, the routine provides an increase in physical and mental fatigue, takes people out of their daily routine, decreases their ability to work and leisure, which makes their standard of living very restricted. Many people reported that on these days they are exclusively dedicated to the treatment and do not feel like doing anything else.
[...] we are restricted to this here during a part of the day and we cannot fail to do it. (A18)
I have to take the day to come here, [...] I do not schedule any other appointments these days [...]. (A10)
[...] I spend a lot of time here, and lately when I get home or I don't even leave, I stay resting [...]. (A15)
There are several obstacles that the routine hemodialysis treatment brings to the patient, especially for those people who need to commute from more distant places. These patients were the ones that showed the greatest dissatisfaction in having to come to carry out the treatment frequently. The qualitative aspects for these people are more affected as a result of losing their whole day traveling.
Oh, I have to leave home early to travel, and when I come back it's already dark, so I cannot do anything else. Not to mention when the bus breaks down on the highway, then I'll get home even later [...]. (A1)
Nutritional restrictions: personal and social repercussions for the CKD patient
The CKD patient undergoing hemodialysis must follow a very restricted diet due to the effects of uremia. Although it is difficult to follow this reduced diet, if restrictions are ignored, it can result in health problems causing the risk of death14,15. Many people feel different because they cannot eat some food and beverages. These restrictions affect the habitual standard of living, being difficult to adapt.
Oh, there is a lot of restriction, even water I can only drink half a liter a day, I cannot eat salt, everything is very little. But we have to follow [...]. (A1)
Because we have to take the potassium from the food, little salt, little liquid, we have to regulate everything [...] it is very bad [...]. (A16)
Adapting to diet is often difficult at the beginning of dialysis, at which point people are still absorbing the idea of being chronically debilitated and dependent on a machine for their survival. Thus, it was found that people with longer treatment times become more resigned with the changes and therefore more adapted, as it can be observed in the following testimony of a patient with seven years of treatment.
[...] some things I cannot eat and liquids are limited, but we can handle it; we just can't exaggerate [...]. (A19, seven years on hemodialysis)
Another important factor that has been mentioned concerns those patients who, in addition to the renal problem, still had underlying diseases or comorbidities, such as diabetes mellitus (DM), for example15. In this way, the person is submitted to two specific diets, which increases the complication factor to its adaptation.
[...] now it got more difficult [...], one thing you can eat in one [diet] and in the other you cannot eat. That's complicated. (A3)
During the approach on nutritional and water diet, there was an isolated factor that deserves to be highlighted because of its importance in this context. This is a patient's report about his diet:
In my diet, nothing has changed, because I don't do it. (A12)
The diet for this patient gains a different context with respect to restrictions. He says he is knowledgeable about dietary restrictions but does not follow them because he does not like it and prefers to make use of foods that are forbidden. Added to this is the fact that he does not perform the treatment on days when he is not present in the city. This fact reinforces the idea that patient awareness should be continuous. A real re-education. A study16 stressed that complying with the diet is an important factor for the efficiency of the treatment, so it must be followed strictly. Hence the need for frequent care and attention to the patient.
Some authors1,17 have suggested that the daily life of CKD patients undergoing hemodialysis is quite repetitive, favoring sedentary lifestyle, social isolation and the loss of some functions. Due to the various restrictions and mandatory treatment, people develop a sense of incapacity towards CKD. Many isolate themselves because they find themselves unable to attend social environments because of their limitations, linking their lives to the treatment alone. The arguments of the following interviewees can confirm this idea:
I don't go out because I cannot drink, I cannot eat almost anything [...]. (A1)
I used to go out, [...], but today I have not gone anymore; I have stayed more at home [...]. (A15)
I stopped going out too much, I do not feel like it anymore [...]. (A4)
Another important factor that leads to disability and stimulates social isolation is the impossibility that some people have to work, since without working the salary is restricted to disability retirement, generating instability and a state of inactivity that prevents the person from social interaction. Some interviewees reported that living from disability retirement is bad and that they wanted to continue working.
[...] living with disability retirement is very bad, [...] I wish I could work. (A3)
The amount of the retirement is very little [...], I could still work if I did not have to do the treatment [...]. (A12)
Another relevant aspect that emerges in this study concerns the pleasure trips that have become more difficult due to the continuity of therapy, eliminating almost all the alternatives of leisure in this sense. Some people approach this difficulty:
My life has become affected. I wish I could visit my relatives but I cannot. For example: a long trip, if we do not get a vacancy there, we cannot go [...]. (A11)
[...] I have to go to a city that has dialysis, because if it does not have, I cannot go. That annoys me [...]. After I started dialysis, I have never traveled again. [...]. (A15)
Meeting what experts have said1,18, these reports demonstrate that the chronic renal patient is faced with several changes throughout his/her treatment, generating enormous losses and social changes, which, consequently, interferes in his/her life in relation to the qualitative aspects.
CONCLUSION
The accomplishment of this study allowed knowing and identifying the changes in the standard of living of the CKD patient undergoing hemodialysis. It was verified that all interviewees are aware of the impact of a chronic illness on people's lives. Most patients' reports showed a negative balance in relation to the standard of living. There are many changes in the life of the CKD carrier; the daily reality of these people is permeated by modifications that limit them in a series of events and that require adaptations.
The daily modifications after adherence to the treatment were the most approached, such as the impossibility of performing bodily and recreational activities, job loss, dietary and water restrictions, changes in social life and the monotonous routine that affect patients' lives and contribute to decrease their quality of life.
Therefore, the knowledge of the profile of the patients interviewed and their speeches allowed considering that the nursing professionals, because they are the ones who spend most of the time close to the patients in dialysis treatment, should put into practice the role of educators, thus promoting greater conditions of improvements to these patients in order to affect their adherence and adaptation to therapy. Thus, educating, welcoming, motivating and including the family/community are also strengthening strategies for coping with hemodialysis. In addition, knowledge of the limitations and difficulties of the patients assisted in the service allows the multidisciplinary team to formulate new strategies in search of excellence in the quality of care.
REFERENCES
1.Rudnicki T. Predictors of quality of life in chronic renal patients. Estud Psicol. 2007; 24(3): 343-51.
2.Martins MRI, Cesarino CB. Quality of life of people with chronic kidney disease undergoing hemodialysis. Rev Latino-Am Enferm. 2005; 13(5): 670-6.
3.Brazilian Society of Nephrology. Report of the Brazilian dialysis census. São Paulo: SBN, 2014.
4.Siviero PCL, Machado CJ, Cherchiglia ML, Drumond EF. Chronic renal insufficiency and multiple causes of death: a descriptive analysis for Brazil, 2000 to 2004. Cad Saúde Colet. 2014; 22(4): 372-9.
5.Nettina SM. Nursing practice. 7th ed. Rio de Janeiro: Guanabara Koogan; 2003.
6.Santos PR, Pontes LRSK. Change in the level of quality of life in patients with end-stage renal disease during a 12-month follow-up. Rev Assoc Med Bras. 2007; 53(4): 329-34.
7.Souza EF, Martino MMF, Lopes MHBM. Nursing diagnoses in patients undergoing hemodialysis using the theoretical model of Imogene King. Rev esc enferm USP. 2007; 41(4): 629-35.
8.Gullo ABM, Lima AFC, Silva MJP. Reflections on communication in nursing care for the chronic renal patient. Rev esc enferm USP. 2000; 34(2): 209-12.
9.Machado LRC, Car MR. The dialectic of everyday life in patients with chronic kidney disease: between the inevitable and the casual. Rev esc enferm USP. 2003; 37(3): 27-35.
10.Diniz DP, Schor N. Outpatient and hospital medicine guides: quality of life. Barueri (SP): Manole; 2003.
11.Bardin L. Content analysis. Lisbon, Portugal: Editions 70, LDA; 2009.
12.Abreu IS, Nascimento LC, Lima RAG, Santos CB. Children and adolescents with renal failure on hemodialysis: professionals' perception. Rev Bras Enferm. 2015; 68(6): 1020-6.
13.Furtado AM, Lima FET. Self-care of patients with chronic kidney disease with arteriovenous fistula. Rev Gaúcha Enferm. 2006; 27(4): 532-8.
14.Smeltzer S, Bare B. Medical-surgical nursing treaty. 10th ed. Rio de Janeiro: Guanabara Koogan; 2005.
15.Santos ACB, Machado MC, Pereira LR, Abreu JLP, Lyra MB. Association between quality of life and nutritional status in chronic renal patients on hemodialysis. J Bras Nefrol. 2013; 35(4): 279-88.
16.Cuppari L. Nutrition guides: clinical nutrition in the adult. Barueri (SP): Manole; 2002.
17.Abreu IS, Santos CB. Health-related quality of life of hemodialysis patients. Rev enferm UERJ. 2013; 21(1): 95-100.
18.Unruh MI, Hartunian MG, Chapman NM, Jaber BI. Sleep quality and clinical correlates in patients on maintenance dialysis. Clin Nephrol. 2003; 59(4): 280-8.