REVIEW ARTICLES
Benefits of home care to elderly peopel with chronic diseases: systematic literature review
Carolina Baltar DayI; Lisiane PaskulinII
IMaster Student from the Post-Graduation Program in Nursing, Federal University of Rio Grande do Sul. Porto Alegre, Rio Grande do Sul, Brazil. E-mail: carolinabday@gmail.com.
IIAdjunct Professor from the Post-Graduation Program in Nursing, Federal University of Rio Grande do Sul. Porto Alegre, Rio Grande do Sul, Brazil. E-mail: paskulin@orion.ufrgs.br.
ABSTRACT: The study aimed at describing the benefits of home care (HC) to elderly with chronic damages, through a systematic literature review, which was held in the MEDLINE database of the PubMed. Nine papers were included in the sample, covering a total of 1.825 elderly subjects, with a time of follow-up ranging from 3 months to 10 years. All selected papers made comparisons between home care and other kinds of care. There was a prevalence of males in the surveyed samples, and heart failure was the most common underlying disease. Mortality was lower in patients who received home care actions. As for admissions, average of days of hospital admissions, functional capacity and quality of life, the practice of home care showed similar results in comparison to other kinds of care. With regard to costs, home care proved to be a less expensive practice. The results found are not unanimous; that is why further studies are necessary to the effectiveness of these interventions.
Keywords: Home Care Service; Chronic Disease; Elderly Population; Elderly’s Health.
INTRODUCTION
The demographic and epidemiological transition is characterized by the increase of users suffering from non-communicable chronic diseases that need care at all levels of complexity1. It is known that their incidence increases with aging2. The Brazilian policies aimed at serving the elderly population suggest the deployment of specific strategies for changing the care model for this age group. One of these strategies is the home care (HC), which is configured as an alternative to the hospital admission3 and to the organization of health care4. In Brazil, there are several policies supporting the HC5.
The National Policy for Primary Care provides that the Brazilian Unified Health System (SUS) must offer a humanized home care to elderly people6. In this policy, the guideline of regionalization recommends that basic health units, according to their areas of coverage, diversify their assistential offers, including HC7. The Law nº 10.424, of April 15th, 2002, adds to the Organic Health Law nº 8.080, of September 19th, 1990, the home care through the SUS8. The Resolution of the Board of Directors nº11, elaborated in 2006, from the National Agency of Health Surveillance, determines minimum operating requirements of HC services in terms of assistance and home admission through the SUS, and complementary systems9.
Although policies contemplate HC, this has been fragmented, with recent hierarchicalized and regionalized initiatives. National papers have described some successful models and experiences, but there are few studies that show the benefits of this modality5. Several developed countries have incorporated HC in the health system, such as, for example, in most of the provinces of Canada10, Japan and Sweden11,12. In the United States and European countries, HC is a common practice for accelerated health recovery and reducing costs13. In Korea, program Home Health Nursing Care performed a significant role in the health system in the 2000s14.
Brazilian studies only address experience reports and the importance of the issue, but none, until this moment, assesses the nursing intervention in home care through randomized controlled trials15. It is hoped that this study will contribute to the effective implementation of HC in the SUS network, offering subsidies for nursing home care practice within the public health scope. The purpose of this study was to describe the benefits of HC to elderly people with chronic damages through systematic literature review.
METHODOLOGY
This is a systematic review, which was conducted in accordance with the methodology found in the Cochrane Handbook, produced by the Cochrane Collaboration and in the Competency Demonstrations Report, published by the Centre for Reviews and Disseminations, in which it must be held in seven steps: formulation of the research question, location of studies, critical assessment, data collection, analysis and presentation of data, data interpretation, enhancement and updating of the review16. The descriptors ‘home care service’, ‘chronic disease’ and ‘aged’ were surveyed as Medical Subject Headings Terms in the MEDLINE database of the PubMed, in order to identify papers, in the month of August 2010.
The 32 selected papers were subjected to critical assessment with regard to the presence of the following inclusion criteria: randomized controlled trials, with participants with an average age of 60 years or over, available in their full versions in the Portal of Periodicals of the Coordination for the Improvement of Higher Education Personnel (CAPES), published between 1990 and 2010, in English language, with HC interventions performed by nurses, multidisciplinary team or other professional, in the community scope or during transition from hospital admission to residence, compared to care provided in hospitals, outpatient units and consulting rooms, or without any provided care.
Inclusion criteria were met by nine papers17-25. During data collection, the following variables were identified: surveyed population, underlying disease, location of development of the study, performed intervention and outcomes found. These were grouped by similarities and their results were interpreted in order to determine the contributions found and their applicability, with sights to answer to the research question.
RESULTS AND DISCUSSION
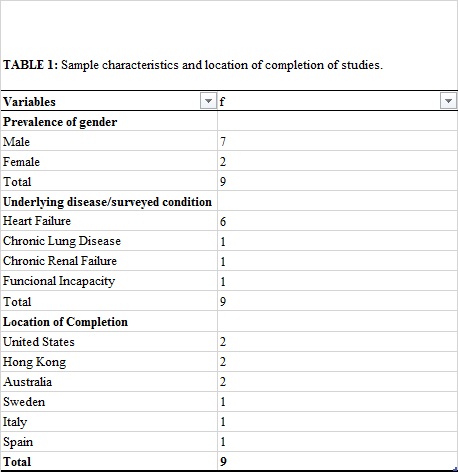
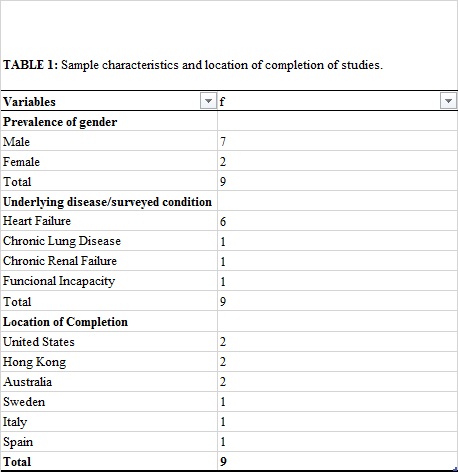
The nine studies17-25 were published in the period from 2003 to 2009 and covered a total of 1.825 elderly patients, with time of follow-up ranging from 3 months to 10 years. It was found a prevalence of males in seven studies17,18,20-24; heart failure was the underlying disease in six studies17,18,20,21,23,25. It should be noted that all studies17-25 were conducted in developed countries. The distribution of studies according to the characteristics of the investigated samples and location of completion is described in Table 1.
The intervention (I) offered in all surveyed papers was marked by the HC after hospital discharge through multidisciplinary home visits (MHV)17,18,22,23, home visits with community nurses (HVN)20,21,24,25 and interventions of occupational therapists (OT)19. For the control group (C), it was offered a care of the hospital admission type (HA)17,18,21, hospital medical consultations (MC)20,22,-24, telemedicine (TM)25 or none kind of care (NC)19.
The outcomes assessed in the nine papers are: hospital readmission (HR), costs, functional capacity (FC), quality of life (QOL), mortality, average of days of hospital admission (AHA) and survival. The variables analyzed and outcomes found in each study are described in Figure 1.
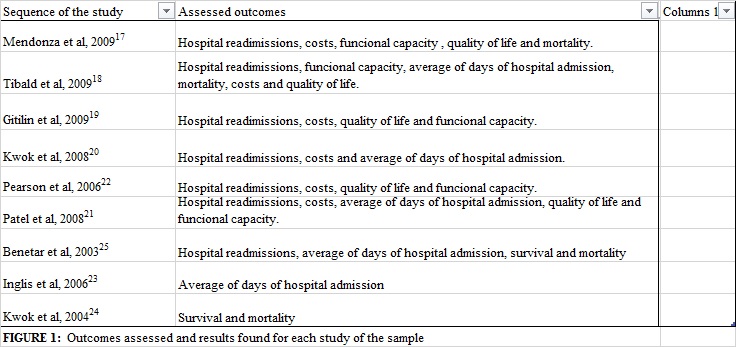
The HR was analyzed in the papers17,18,20-23,25. In five texts17,18,20-22, there was no statistically significant difference between the intervention and control groups (40,5% vs 50%, with p=0,42; 57 vs 46, with p=0,23; 17 vs. 34, with p=0,29; 65 vs 69, with p=0,23 and 76 vs 62, with p=0,08, respectively). In one study25, there was a greater number of HR in the group that received HC than in the control group (63 vs. 38, with p<0,05), and in other study23, the largest number of HR, on average, occurred in the control group, which received care actions through MC (2,04±3,23 intervention vs 3,66±7,62 control, with p <0,05). These results were statistically significant.
As for cost, the studies showed a statistically significant difference between the intervention and control groups, being that it is lower in the intervention (€2.541±2153 vs € 4.502±2153, with p <0,001; US$2.604,46 vs US$3.027,78, with p<0,00; $823±1.642 vs $960±1.376, with p=0,045; €1.122 vs €5.110, with p=0,05; US$177.365 vs US$65.023, with p<0,02, respectively). One study17 included costs involving medications and diagnostic examinations in both groups. The intervention group still included costs with home visits and HA.
Moreover, other study18 took in account the hospital costs in the control group and costs with the time spent by each professional during the home intervention. Another study22 assessed only the costs with admissions of patients with CRF in both groups. In another research2, it was considered to HC, the time costs of nurses and physicians, as well as laboratory examinations and medication administration. Hospital costs were also considered for the control group. Moreover, an investigation25 did not detail the actions and resources that were included as costs for both groups.
One study20 examined the costs from the perspectives of the health system and of patients, being that it is lower in the intervention group in both cases (HK$10.186 vs HK$21.599, with p>0,05, and HK$513 vs HK$775, with p=0,11, respectively), and these differences were not statistically significant. For the health system, we have included the costs of HVN, specialists, emergency care actions and HA. For the patient, we have included costs involving health care actions and visits conducted by nurses, in addition to the use of social services not covered by the health system. It appears that the calculations originated from all the surveyed studies17,18,20-22,25 have included the costs of HVN, MHV and HA of those linked to the HC group.
As for AHA, it was found in the papers18,22,24 that there was no statistically significant difference in this variable between the intervention and control groups (22,1±12,2 vs 25,3±9,5, with p=0,15; 5,88±10,81 vs 6,48±11,56, with p=0,28 e 20,3±25,3 vs 19,2±25,6, with p<0,29, respectively). One study25 found a lower AHA in the control group than in the intervention group (49,5 vs 105, with p<0,01), and another study found23 a lower AHA in the intervention group (14,8 ± 23,0 vs 28,4 ± 53,4, with p<0,05), and these results were statistically significant.
The FC and QOL were assessed in the studies17,18,20,21,25. The first study17, after use of the Barthel Index (BI) and of the Short Form (SF-36) Health Survey, found that the variation of the results in the two instruments was not statistically significant between the investigated groups (p>0,05). The second investigation18 used the instruments BI and Instrumental Activities of Daily Living to assess the FC, where the control group had better results, but without statistically significant difference (p=0,40, p=0,29, respectively). Better and statistically significant results were presented by the intervention group regarding depression and QOL, assessed by the Geriatric Depression Scale and Nottingham Scale (p=0,02 ; p = 0,046 respectively).
The third study20 assessed the FC through the test of six-minute walk and the London Handicap Scale and found that there was no statistically significant difference (p>0,05) in both groups. Regarding the independence of patients, those belonging to the intervention group became less limited than those of the control group. The fourth study21, which made use of the Kansas City Cardiomyopathy Questionnaire, the Short Form (SF-36) and the EuroQol five-dimension questionnaire (EQ-5D), did not observe any difference in QOL and FC in both groups after the intervention.
The latter study25 used the instruments Minnesota Living with Heart Failure Questionnaire, Quality of Life Index-Cardiac Version, Hospital Anxiety and Depression Scale and the Heart Failure Self-Efficacy Scale 30 to assess how patients perceive the effect of the disease in their lives, the psychological distress manifested by anxiety and depression and, finally, the treatment adherence. The scores between the two groups showed no statistically significant differences (p>0,05), however, the best results were found in the group that received care actions by means of telemedicine.
With respect to mortality, two studies17,18 showed no statistically significant differences between the control group and the intervention group (5,4% vs 8,8%, with p=0,67; mortality in 15% of the sample, with p>0,05) 17,18. Nonetheless, in other studies19,23, the difference of mortality between the intervention and control groups was statistically significant (77% vs 89%, with p=0,02; 5,6% vs 13,2%, with p=0,0006, respectively).
Regarding survival and risk for vital event, in one study22 it was only reported that home care had no impact on patient survival. In another study23, the average of survival was nearly 2 times greater in the HC group than in the MC group (44 vs 22 months), and home care was associated with a reduction of 40% in the risk for fatal event after the time of follow-up of the study (p <0.0001). Longer survival of patients of the intervention group than in the control group was identified in another study19, where the effect of HC on survival remained statistically significant for two years (p=0,02) and the risk for death was eight times higher in the control group, which received no care.
It was perceived a prevalence of male samples in most studies17,18,20-24. It was expected to find a larger number of women, since they live longer and therefore have more chronic damages26. The most common underlying disease found in these approached researches, with the largest number of male patients in their samples, was the HF, which is an illness prevalent in men and its incidence increases with age, especially over 50 years old27. It is also possible that it is the most studied disease because of the mentioned characteristics and the fact that there are several professional interventions to promote self-care of such patients. It should be observed that all studies17-25 were conducted in developed countries, since these countries face the aging process for a longer time, thereby holding a large proportion of elderly people living alone and seeking modalities of care most appropriate for the care of this population.
Regarding mortality, it was found a statistically significant difference in half of the studies in which this variable was studied, and only two studies17,18 have demonstrated a lower number of deaths among patients who received HC19,23. It is noteworthy to mention that studies with statistically significant results followed these patients for a longer time than in studies that did not achieve significant results. The number of patients who comprised the sample of studies with statistical significance was approximately 3,5 times greater than the others (606 patients vs. 172 patients, respectively). Two meta-analyses that assessed the effectiveness of home visits in the promotion and prevention of the elderly subjects found that these visits have reduced mortality28,29. A most recent systematic review has identified in six studies, which assessed the mortality of elderly patients with poor health who received home visits and who did not receive such intervention, that there was no statistically significant difference in mortality between the two groups30.
The HR during the course of the studies17,18,20-23,25 was similar for those who received HC and for those who received other kinds of care. The difference between these values was statistically significant in two studies23,25, but only one study23 has shown HR indexes lower in patients who received home interventions, or that were monitored for 10 years. It is noteworthy to emphasize that the time of follow-up of this study was 5 times greater than the average time of follow-up of non-statistically significant studies. The AHA was also similar between the intervention and control groups in the three studies that assessed this outcome18,22,24. Results found in the literature claim that home visits have not shown significant effect on the frequency of hospital admissions and on the AHA of the elderly population28,30. The study in which the telemedicine was offered to the control group showed less HR and shorter hospital stay, however, the duration of such study was 1 year, which might have influenced its results25.
A review study that compared the effects of telemedicine in different health situations showed no significant results in reducing readmissions31. The same was found in a meta-analysis comparing telemedicine with multidisciplinary outpatient care, which revealed that the number of hospital admissions, for any kind of illness, did not obtain statistically significant difference32. A systematic review of studies, comparing the use of communication technologies with the direct contact with patients with chronic damages through home care, primary care and emergency services, identified that there is still little evidence on clinical benefits of this kind of technology in relation to others33.
Most studies have demonstrated that survival was greater in patients who underwent HC19,23. Regarding the characteristics of the subjects who comprised the sample in two groups of studies with statistically significant differences19,23, it was identified a higher proportion of people living alone compared with those of the study found no statistically significant difference22. As for QOL, only one paper18, which compared care provided by HC with care provided by HA, found improvement in quality of life of patients who received home care. A review, which identified health care models for the elderly subjects with chronic damages, showed that QOL was better in patients receiving home care actions34.
In relation to FC, the assessed studies showed no evidence that the proposed home care actions have improved the FC of elderly subjects17,18,20,21.
Nevertheless, the time of follow-up of these studies ranged from 6 months to 1 year, i.e., there is no significant time to perceive a greater functional decline in the elderly subjects of the control group and of the home intervention group. In a meta-analysis, it was identified that the FC was improved in elderly patients who received home visits in a statistically significant way, and it has unveiled a reduction of 24% in the risk of decline in the FC29. Another meta-analysis reported no significant improvement in FC of those who received home care28. A systematic review, conducted with 29 studies, assessed the FC in four of these, where one study showed improvement in FC of patients who received some care type at home, up to one year of follow-up of the study, with statistically significant differences, but three found no such differences, where one of them was not a randomized controlled trial30.
With respect to the costs of HC in comparison with the costs of care provided to the control group, in most investigations, the cost was lower for those who received HC17,18,20-22. It is still noteworthy to highlight that studies with results involving statistically significant differences17,18,20,22,25 assessed approximately 7 times more patients than the study that did not identify statistical significance21, in an average time of hospital admission five times. The cost was lower in the control group in one study25 that made use of telemedicine. Telemedicine developed by nurses was the kind of care offered, but in a shorter period of follow-up and with fewer patients in comparison with studies that found lower cost of home care. Perhaps this result might be explained by the level of complexity of health of chronic patients enrolled to this kind of program, who required monitoring of vital signs and received health guidelines by telephone, before the altered vital signs, or necessity for obtaining information about their health conditions. These patients did not require the use of other more complex resources, with no travel costs involving specialized professionals to go to the patients' household, thereby making the service cheaper. A systematic review that assessed the cost-effectiveness of telemedicine has concluded that there is little evidence that it is a care model with better cost-effective in relation to other kinds of care35.
CONCLUSION
The analyzed papers did not provide unanimous evidence of the benefits of HC compared with other modalities of care. Some studies have shown the contribution of the practice of HC to reduce mortality rates and achieve an increased survival to elderly patients with chronic damages, presenting lower costs for the completion of care actions.
As limitations of this study, it should be cited the lack of randomized controlled trials on the issue at stake, the great sampling diversity and the comparison of HC with different interventions.
It is hoped that the benefits offered by the practice of HC, identified throughout this study, might contribute to the implementation of this modality of care in the SUS, as well as to elaborate assessment indicators appropriate to the national reality. Accordingly, this study contributes to the delineation of future interventions and researches in the topic of aging and its interface with nursing, thereby helping to define best care models, target audience and means for assessment of the care actions to be developed. Thus, we suggest the development of studies that assess the benefits that the practice of HC can bring to elderly people with chronic damages in the context of the care network of the SUS.
REFERENCES
1. Silva Junior JB, Gomes FBC, Cezário AC, et al. Doenças e agravos não-transmissíveis: bases epidemiológicas. In: Rouquayrol MZ, Almeida Filho N. Epidemiologia e Saúde. Rio de Janeiro: MEDSI, 1999, p.289-309.
2. Garcia ESS, Saintrain MVL. Perfil epidemiológico de uma população idosa atendida pelo Programa de Saúde da Família. Rev enferm UERJ. 2009;17:18-23
3. Rehem TCM, Trad LAB. Assistência domiciliar em saúde: subsídios para um projeto de atenção básica brasileira. Ciênc saúde coletiva. 2005;10:231-42.
4. Merhy EE, Feuerwrker LM. A contribuição da atenção domiciliar para a configuração de redes substitutivas de saúde: desinstitucionalização e transformação de práticas. Rev panam salud publica. 2008;24:180-8.
5. Freitas IBA, Nazareth MS, FERLA AA. Atendimento domiciliar ao idoso acamado: integralidade do cuidado a partir da experiência de uma unidade básica de saúde. In: Herédia VBM, De Lorenzi RS, Ferla AA. Envelhecimento, saúde e políticas públicas. Caxias do Sul: Educs, 2007. p.113-30.
6. Ministério da Saúde (Br.). Portaria Nº 399/GM de 22 de fevereiro de 2006. Dispõe sobre o Pacto pela saúde – Consolidação do SUS. Available at: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2006/GM/GM-399.htm. [citado em 28 mai 2010]
7. Herédia VBM, De Lorenzi RS, Ferla AA. Envelhecimento, saúde e políticas sociais. In: Herédia VBM, De Lorenzi RS, Ferla AA. Envelhecimento, saúde e políticas públicas. Caxias do Sul (RS): Educs; 2007. p.9-21.
8. Presidência da Republica (Br). Lei n° 10.424, de 15 de abril de 2002. Acrescenta capítulo e artigo à Lei no 8.080, de 19 de setembro de 1990, que dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento de serviços correspondentes e dá outras providências, regulamentando a assistência domiciliar no Sistema Único de Saúde. Available at: http://www.planalto.gov.br/ccivil_03/leis/2002/l10424.htm. [citado em 29 mai 2010]
9. Agência Nacional de Vigilância Sanitária. Resolução RDC Nº 11, de 26 de janeiro de 2006. Dispõe sobre o Regulamento Técnico de funcionamento de serviços que prestam atenção domiciliar. Available at: http://www.saude.mg.gov.br/atos_normativos/legislacao-sanitaria/estabelecimentos-de-saude/atencao-domiciliar/ANVISA11.pdf. [citado em 3 jun 2010]
10. Portaria MS N° 2.528 de 19 de outubro de 2006. Institui a Internação Domiciliar no âmbito do SUS. Available at:http://portal.saude.gov.br/portal/arquivos/pdf/2528%20aprova%20a%20politica%20nacional%20de%20saude%20da%20pessoa%20idosa.pdf. [citado em 30 mai 2010]
11. Thomé B, Dykes AK, Hallberg IR. Home care with regard to definition, care recipients, content and outcome: systematic literature review. J clin nursing. 2003;12:860–72.
12. Murashima S, Nagata S, Magilvy JK, Fukui S, Kayama M. Home care nursing in Japan: a challenge for providing good care at home. PublicHealthNurs. 2002;19:94-103.
13. Amaral NN, Cunha MCB, Labronici RHDD, Oliveira ASO, Gabbai AA. Assistência domiciliar à saúde (home health care): sua história e sua relevância para o sistema de saúde atual. Revista de Neurociência. 2001;9(3):111-7.
14. Ryu H, An J, Koabyashi M. Home health nursing care agenda based on health policy in Korea. Nurs Health Sci. 2005;7:92-8.
15. Ministério da Saúde (Br.). Portaria Nº 2.528 de 19 de outubro de 2006. Dispõe sobre a Política Nacional de Saúde da Pessoa Idosa. Available at: http://portal.saude.gov.br/portal/arquivos/pdf/2528%20aprova%20a%20politica%20nacional%20de%20saude%20da%20pessoa%20idosa.pdf. [citado em 30 mai 2010]
16. Rother ET. Revisão sistemática versus revisão narrativa. Acta Paul Enferm. 2007;20:5-6.
17. Mendonza H, Martín MJ, García A, Arós F, Aizpuru F, Regaldo De Los Cobos J, et al. ‘'Hospital at home' care model as an effective alternative in the management of descompensated chronic heart failure. Eur J Heart Fail. 2009;11:1208-13
18. Tibald V, Isaia G, Scarafiotti C, Gariglio F, Zanocchi M, Bo M, et al. Hospital at home for elderly patients with acute descompensation of chronic heart failure. Arch Intern Med. 2009;169:1569-75.
19. Gitlin LN, Hauck WW, Dennis MP, Winter L, Hodgson N, Schinfeld S. Long-term effect on mortality of a home intervention that reduces funtional difficulties in older adults: results from a randomized trial. J Am Geriatr Soc. 2009;57:476-81.
20. Kwok T, Lee J, Woo J, Lee DT, Griffith S. A randomized controlled trial of a community nurse-supported hospital discharge programme in older patients with chronic heart failure. J clin nursing. 2008;17:109-17.
21. Patel H, Shafazand M, Ekman I, Höjgård S, Swedberg K, Schaufelberger M. Home Care as an option in worsening chronic heart failure: a pilot study to evaluate feasibility, quality adjusted life years and cost-effectuveness. Europ J Heart Failure. 2008;10:675-81.
22.Pearson S, Inglis SC, McLennan BA, Brennan L, Russell M, Wilkinson D, et al. Prolonged effects of a home-based intervention in patients with chronic illness. Arch Intern Med. 2006;166:645-50.
23. Inglis SC, Pearson S, Treen S, Gallasch T, Horowitz JD, Stewart S. Extending the horizon in chronic heart failure: effects of multidisciplinary, home-based intervention relative to usual care. Circulation. 2006;114:2466-73.
24. Kwok T, Lum CM, Chan HS, Ma HM, Lee D, Woo J. A randomized, controlled trial of an intensive community nurse-supported discharge program in preventing hospital readmissions of older patients with chronic lung disease. J Am Geriatr Soc. 2004; 52:1240-6.
25. Benetar D, Bondmass M, Ghitelan J, Avitall B. Outcomes of chronic heart failure. Arch Intern Med. 2003;163:347-52.
26. Aires M, Paskulin LMG, Morais EP. Capacidade funcional em idosos mais velhos: estudo comparativo em três regiões do estado do Rio Grande do Sul. Rev Latino-Am Enfermagem. 2010;18:[7 telas].
27. Ho KKL, Pinsky JL, Kannel WB, Levy D. The Epidemiology of Heart Failure: The Framingham Study. JACC. 1993; 22:6A-13A.
28. Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323:1-9.
29. Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visit to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287:1022-8.
30. Bouman A, Rossum EV, Nelemans P, Kempen GIJM, Knipschild P. Effects of intensive home visiting programs for older people with poor health status: a systematic review. BMC Health Services Research. 2008;8:1-11.
31. Schmidt S, Schuchert A, Krieg T, Oeff Ml. Home telemonitoring in patients with chronic heart failure. Dtsch Ärztebl Int. 2010;107:131-8.
32. Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewar S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 2007;334:1-9.
33. Currel R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practic and health care outcomes. Cochrane Database of Systematic Reviews. 2000;10:1-35.
34. Boult C, Green AF, Boult LB, Pacala JT, Snyder C, Leff B. Successful models of comprehensive care for older adults with chronic conditions: evidence for the institute of medicine's Retooling for an Aging America report. J Am Geriatr Soc. 2009;57:2328-37.
35. Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ. 2002;324:1434-7.