(*) Live without a partner: single, divorced and widowed.
(**) Minimum wage (MW) in force in the period of data collection was of R$ 465,00.
RESEARCH ARTICLES
Sociodemographic and health profile of elderly patients with depressive symptoms
Andréa dos Santos SouzaI; Edite Lago da Silva SenaII; Edméia Campos MeiraIII; Doane Martins da SilvaIV; Marta dos Reis AlvesV; Luma Costa PereiraVI
INurse. PHD Student from the Post-Graduation Nursing Program at the Federal University of Bahia and Assistant Professor from the Graduation Nursing Course
at the State University of the Southwest Bahia. Jequié, Bahia, Brazil. E-mail: andreasouza_75@hotmail.com
IINurse. PHD in Nursing. Adjunct Professor from the Graduation Nursing Course at the State University of the Southwest Bahia. Jequié, Bahia,
Brazil. E-mail: editelago@gmail.com
IIINurse. Master in Nursing. Adjunct Professor from the Graduation Nursing Course at the State University of the Southwest Bahia. Jequié, Bahia, Brazil.
E-mail: edmeiameira@yahoo.com.br
IVNurse. Master Student from the Post-Graduation Nursing and Health Program at the State University of the Southwest Bahia. Jequié, Bahia, Brazil. E-mail: doane.ef@hotmail.com
VNurse. Master Student from the Post-Graduation Nursing and Health Program at the State University of the Southwest Bahia. Jequié, Bahia, Brazil. E-mail: martareisalves@yahoo.com
VINurse. Master Student from the Post-Graduation Nursing and Health Program at the State University of the Southwest Bahia. Jequié, Bahia, Brazil. E-mail: lumacosta88@hotmail.com
ABSTRACT
Quantitative study, of descriptive-exploratory type aiming at describing the sociodemographic and health profile of elderly with depressive symptoms, living in the ranging area of a Family Health Unit of the municipality of Jequié-BA. The sample consisted of 125 elderly patients who underwent the application of a structured form and to the Short Geriatric Depression Scale, from October 2009 to December 2010. The results revealed the prevalence of depressive symptoms in 88.8% of the older people surveyed, who were predominantly female, of low income and education level, age group between 60 and 69 years old and suffering from chronic diseases. The screening of elderly people at risk of depression and the configuration of their demographic profile are an important support for planning and implementation of preventive actions, early diagnostic and treatment of depression.
Keywords: Evalution; depression; elderly; prevalence.
INTRODUCTION
The process of population aging has increased the prevalence of psychiatric diseases, noteworthy among them the clinical pictures of depression. Although it is not a specific disease of the third age, older people are often affected and might result in functional disability, social isolation and, even, suicide cases. It is estimated that the prevalence rates of this pathological condition range from 4,8 to 14,6% in the elderly population living in the community1.
With the prolongation of life, it becomes more common the death of friends, neighbors and spouses, the adaptation to retirement, the reduction of friendships network, difficulties in establishing new bonds and the onset/worsening of chronic pathologies. Furthermore, the longevity makes closer the most feared of all the losses – the life itself. This entire context makes the elderly people more vulnerable to depression.
It should be highlighted that this pathological condition increases the risk of morbidity, as well as can trigger a high index of utilization of health care services, which generates high economic cost to society and interferes with the quality of life of the elderly subject1.
Given the magnitude of the consequences of depression in the elderly subject, the identification of those at risk situation for the disease might contribute to the planning and the practice of interdisciplinary actions aimed at providing a quality aging, besides creating opportunity for socializing experiences of utilization of recommended tools, in addition to proposing new strategies required by the dynamics of living/aging in different contexts.
Based the above mentioned, the study aimed at delineating the sociodemographic and health-related profile of older people with depressive symptoms, who were residents in the coverage area of a family health unit (FHU) of the city of Jequié – Bahia State – Brazil.
LITERATURE REVIEW
Depression is a pathological change in mood that can reach from children to elderly people, regardless of socioeconomic status, breed, culture and geographical space. It is a psychiatric syndrome that negatively interferes with the quality of life, risking the human being in its entirety with no split between the psychological, social and physical scopes2,3.
This pathology is characterized by depressed mood, loss of interest and pleasure in previously enjoyable activities, reduction of affection, fatigue or sense of loss of energy, nervousness, anxiety, altered sleep-wake cycle, appetite change, isolation, discouragement and apathy4,5.
Currently, for identifying clinical pictures of depression, one should make use of the available diagnostic criteria in the International Classification of Diseases and in the Diagnostic and Statistical Manual of Mental Disorders, which, according to the presence and duration of certain characteristic symptoms of depression, classify the depressive disorders in greater, lesser or dysthymic6.
Furthermore, there are scales for screening depressive symptoms, noteworthy among them the Short Form of the Geriatric Depression Scale (GDS-15). This scale is comprised of 15 dichotomous questions (yes vs. no), which are easy to understand. The GDS-15 suggests risk for depression, and is not a single diagnostic criterion for this pathological condition1.
In this perspective, it becomes relevant to identify the prevalence of depressive symptoms in older people, as well as elaborating their sociodemographic and health-related profile, since this information can provide subsidies for implementing actions targeted to the care of those who experience a condition of risk for this pathology at stake.
METHODOLOGY
It is a quantitative research, with a descriptive and exploratory nature, which was performed in the coverage area of a FHU of Jequié, Bahia State, in the period from October 2009 to December 2010, having as its study population a sample of 167 elderly subjects registered in one of the teams from the family health strategy of the above mentioned unit. After statistical calculation, the sample was enclosed in 125 (74,85%) elderly, i.e., people aged 60 or over, who had the cognitive ability to answer to the form and that agreed to participate in the survey, allowing the use of their data upon the signature of the Free and Informed Consent Form, after being informed of the aims and methods of the study. It should be emphasized that the subjects were randomly selected.
The research took place in three steps. At first, the health team was assembled, the project was presented, and the team members requested the collaboration of community health workers (CHW) for finding households in which there were elderly people. Initially, we created a spreadsheet for easy filling, organized by micro-areas, updated, when necessary, by the CHW during the process of data collection. With a prior appointment, the previously trained researchers went the next step, the first contact with the elderly subjects in their respective homes and the application of the Mini-Mental State Examination (MMSE) to assess a possible cognitive deficit. Older people with no deficits were subjected to the Short Form of the Geriatric Depression Scale (GDS-15), for screening depressive symptoms, respecting the recommendations governing their usage.
This scale was translated into Portuguese and adapted for being applied in Brazil and possesses satisfactory reliability and validity properties for screening clinical pictures of depression in elderly people7. We have used the version recommended by the Brazilian Ministry of Health, which is comprised of 15 questions with dichotomous responses (yes or no). To assess the results obtained through the GDS-15, we have obeyed the following cutting off points: a score between 0 and 5 is considered normal; between 6 and 10 indicates mild depression; and between 11 and 15 can infer a severe depression4.
In the third step, the elderly people identified at risk of depression had the application of a structured form, which was developed by the researchers and encompassed sociodemographic and health-related characteristics of the elderly population, such as age group, gender, marital status, schooling, religion, family income, referred pathologies, self-perception of health status and depressive symptoms that were mentioned.
The elderly subjects were visited in a random way, since that the interviewed were those indicated by the CHW. The residences that were closed at a first time were revisited and, after a third unsuccessful attempt, the elderly were removed from the list of possible respondents. These steps were conducted until completing the total number previously calculated for composing the sample.
After possessing the filled instruments, a database in Microsoft Excel 2007 was created, which was always fed by, at least, two people who took turns at scheduled intervals, thereby reducing the possibility of error resulting from the physical and mental fatigue produced by prolonged use of computer and handling of the instruments. The analysis was performed by making use of descriptive statistical approach, being that it was held a frequency-based distribution of the variables.
This study was approved by the Research Ethics Committee from the State University of Southwest Bahia, under the Protocol nº 250/2008. It should be emphasized the fulfillment of the ethical precepts of the autonomy, non-maleficence, beneficence and justice of research involving human beings, according to the Resolution nº 196/96 of the National Health Council8.
RESULTS AND DISCUSSION
From the collected data, it was possible to observe that, from the 125 (100%) surveyed elderly people, 111 (88,8%) were at risk of depression, being that 110 were at light level and only one were at a severe level; the 14 remaining (11,2%) were at a normal level.
The prevalence of depressive symptoms in 111 (88,8%) of the surveyed seniors was superior to that found in other studies performed with elderly people living in the community, which ranged from 59,3%9 to 23,34%1. These differences in the prevalence index might be associated with different scales used to for screening clinical pictures of depression, as well as possible sociodemographic distinctions of participants. In a research conducted in the Northeast Region of Brazil, in a community of the city of João Pessoa, Paraíba State, making use of the same instrument adopted in this research, it was found a prevalence of 52% risk of depression10.
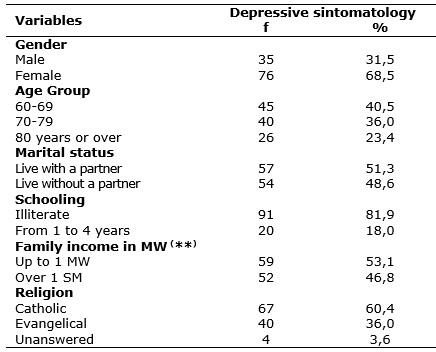
Regarding the gender, there was a prevalence of females, being that the amount was of 76 elderly subjects (68,5%), which corroborates with the results of the Synthesis of Social Indicators of the year 201011, which reveal a feminization of the older population, as shown Table 1.
TABLE 1: Sociodemographic characteristics of older people at risk of depression, who were study participants and inhabitants of Jequié-BA, 2010. (N=111)
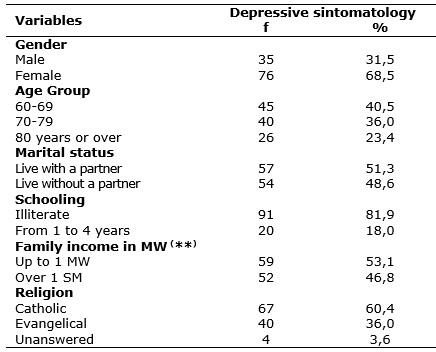
(*)
Live without a partner: single, divorced and widowed.
(**)
Minimum wage (MW) in force in the period of data collection was of R$ 465,00.
Importantly, although women live longer than men, they are exposed for longer periods to chronic diseases, widowhood and loneliness, which implies the possibility of occurrence of depressive disorders12. Another factor that fosters the occurrence of depression in elderly women is that, with the advancement of age and the arrival of menopause, there is a reduction of feminine hormones, especially estrogen, whose decreased availability promotes the occurrence of mood disorders (including depression), due to the fact that it acts on noradrenergic and serotonergic neurotransmission13.
As for age group, there was a predominance of risk of depression among younger elderly, i.e., those aged between 60 and 69 years, represented by 45 (40,5%) of the whole sample, as shown in Table 1. This result is related to the current Brazilian demographic pattern, which denotes a greater representation of this elderly segment11. Moreover, at this stage, the elderly subject faces biological, financial, psychological changes, as well as in its social roles, requiring an adjustment that not always can be held.
Nonetheless, the study shows that depressive episodes are frequent, especially in octogenarian elderly subjects, being that the decline of the health condition is considered as a risk factor for the installation of depressive clinical pictures14. Another study, conducted with elderly people in the city of Recife and its Metropolitan Region, in the Pernambuco State, found that depression is more common in the age group between 70 and 79 years 12.
Concerning the marital status, it was observed that 57 (51,3%) elderly in risk of depression were living together with their spouses/partners, which raises the need to also value the quality of the relationship between the couples, and not only the presence or absence of the sexual partner. Furthermore, it was significant the number of elderly people living without a partner, as shown in Table 1. Widowhood makes the elderly subject more vulnerable to the occurrence of depressive clinical pictures, because stressful and negative life events, such as the loss of a spouse, require adaptation and can constitute the starting point for a mental breakdown, which fosters the development of depressive symptoms9.
With respect to schooling level, it was observed that 91 (81,9%) elderly patients with depressive symptoms were illiterate, confirming results of a previous study performed in the city of Santa Cruz, Rio Grande do Norte State, whose aim was to analyze the influence of sociodemographic and health-related factors on the set of depressive symptoms15.
With regard to family income, it was observed that 59 elderly (53,1%) reported having an income of up to 1 minimum wage, as shown in Table 1. This income is primarily originated from pensions or retirements, being occasionally necessary the existence of financial support on the part of their grown-up children who do not live with these seniors. Accordingly, it should be highlighted that the low purchasing power can limit people's access to food and social care, with emphasis on education and health, which significantly affects the quality of life15.
These results are consistent with a survey conducted in the city of Rio de Janeiro, where it was demonstrated that the prevalence of depression varied in line with the socioeconomic status of the surveyed group, from 20,9%, in subjects with better conditions, to 36,8%, in those living in worst conditions 16. The loss of occupational status, as well as the economic difficulties that undermine the minimum resources to survive, end up predisposing the elderly people to the development of depression17.
As for religion, 107 (96,4%) elderly subjects reported belonging to a religious denomination, according to Table 1. This fact deserves attention, since beliefs can influence in the way in which the elderly people deal with situations that constitute risk of depression, such as stress, suffering, financial and health-related problems. Moreover, in this population group, faith becomes very important, because, the elderly usually have no one to turn to, except to a higher being, causing them to have frequent religious habits18.
In this context, it is believed that higher levels of religious involvement are associated with indicators of psychological welfare (life satisfaction, happiness, positive affect and higher moral), as well as to a lower incidence of depression, suicidal and behavioral thoughts, use /misuse of alcohol/ drugs. Generally, the positive impact of religious involvement on mental health is stronger among people under stress or in situations of weakness, such as the elderly and those people with disabilities and clinical illnesses19.
With regard to health and disease conditions in old age, studies unveil that, at this stage of life, the disease has special meanings, as the elderly subject brings with itself the fear of loss of the functional capacity, hopelessness for getting improvements and perception of the inexorable fate that approaches: death20.
Thus, in the present study, we also sought to know the health conditions of the elderly subjects, where it was found that, from the 111 (100%) seniors who were at risk for depression, 94 (84,7%) reported possessing at least one type of pathology, from whom 63 (67%) reported having a single pathology and 31 (33%) said to have two or three pathologies.
Morbidity is recurrent in aging, however, 17 (15,3%) elderly subjects reported that they had no knowledge of being carrier of any kind of pathology, as shown in Table 2.
TABLE 2: Distribution of elderly people at risk of depression according to health-related variables. Jequié-BA, 2010. (N=111)
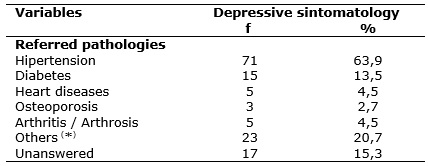
(
*) Others: eye-related and kidney diseases and esophageal varicose veins
Results from a previous study showed that the prevalence of depressive symptoms was strongly related to the number of chronic diseases, and it was evidenced that the elderly subject with more than three chronic diseases, especially Parkinson's disease, cancer and osteoarthrosis, presented a set of depressive symptoms with a greater frequency20.
Chronic diseases contribute to the development of depression through direct action on brain functions or by triggering psychosocial effects. This correlation can also be bidirectionally observed, i.e., depression might precipitate chronic diseases and these chronic diseases might exacerbate depressive symptoms20. The coexistence of depression with other pathology usually contributes to keep it unnoticed for health care professionals who focus their attention on somatic complaints, which might affect the quality of life of certain seniors who could be benefitted from specific treatments.
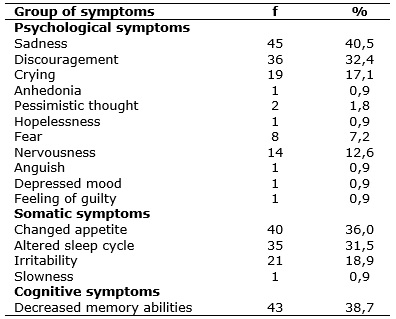
When asked about the presence of depressive symptoms, the elderly showed, with a greater frequency, the group of psychological symptoms, followed by somatic and cognitive signs, as shown in Table 3. Regarding the somatic symptoms, it should be highlighted that they can be present both in depressive disorders and be associated with other pathologies, which, in most cases, hinders the early diagnosis of clinical pictures and also the presence of depression and, consequently, delay the appropriate treatment for each kind of pathology.
TABLE 3: Frequency of depressive symptoms in elderly people at risk of depression, Jequié-BA, 2010. (N=111)
In light of the foregoing, it should be emphasized that the information about the sociodemographic and health-related profile of elderly people with depressive symptoms is crucial to the formulation of intersectoral public policies, committed to this segment of the population with regard to social issues, economic and health-related over the life cycle, which favors planning and intervention by means of more efficient actions, geared to the actual needs of the elderly subjects in their entirety.
CONCLUSION
The study has revealed the prevalence of risk for depression among elderly subjects, female, aged from 60 to 69 years, low-income, illiterate and bearers of chronic diseases.
The screening of elderly people at risk for developing depression and the elaboration of their sociodemographic and health-related profiles are relevant subsidies for planning and implementing preventive or diagnostic measures, as well as providing an early treatment towards the depression, especially in the fields of geriatric and gerontological nursing.
It is believed that knowing a risk situation of a certain health problem is to achieve the possibility to plan and implement actions that can prevent it or reduce its damage, if it occurs. The delay in diagnosis or treatment of depression might represent suffering, functional disabilities, overcharge to family caregivers and even early death of the elderly patient.
As limitations of this study, it should be pointed out the representative homogeneous sample of the socio-cultural reality of a single FHU of the addressed city, as well as the absence of an analytical approach, to observe the possible associations between the risk of depression and the sociodemographic and health-related factors in the elderly living in the community scope.
Therefore, we recommend having the investigation on the risk of depression in a larger sample, through the use of the Short Form of the Geriatric Depression Scale (GDS-15), since this is an instrument for easy application for screening depressive symptoms in the elderly population. Moreover, we suggest the conduction of further studies aimed at identifying the risk factors associated with the geriatric depression, which can help professionals working in this field to diagnose and propose earlier and more appropriate interventions.
REFERENCES
1.Frank MH, Rodrigues NL. Depressão, ansiedade, outros distúrbios afetivos e suicídio. In: Freitas EV, Py L, Cançado FAXC, Doll J, Gorzoni ML. Tratado de geriatria e gerontologia. Rio de Janeiro: Guanabara Koogan; 2006. p. 376-87.
2.Alvarenga MRM, Oliveira MAC, Faccenda O, Cerchiari EAN, Amendola F. Sintomas depressivos em idosos assistidos pela estratégia saúde da família. Cogitare enferm. 2010; 15: 217-24.
3.Coutinho MPL, Gontiès B, Araújo LF, Sá RCN. Depressão, um sofrimento sem fronteira: representações sociais entre crianças e idosos. Psico USF. 2003; 8: 183-92.
4.Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Envelhecimento e Saúde da pessoa idosa. Brasília (DF): Ministério da Saúde; 2006.
5.Santana AJ, Barboza Filho JC. Prevalência de sintomas depressivos em idosos institucionalizados em Salvador. Rev baiana saude publica. 2007; 31: 134-46.
6.Pinho MX, Custódio O, Makdisse M. Incidência de depressão e fatores associados em idosos residentes na comunidade: revisão de literatura. Rev bras geriatr gerontol. 2009; 12: 123-40.
7.Stoppe JR A, Jacob Filho W, Louzã Neto MR. Avaliação da depressão em idosos através da Escala de Depressão em Geriatria: resultados preliminares. Rev ABP-APAL. 1994; 16: 149 - 53.
8.Ministério da Saúde (Br). Conselho Nacional de Saúde. Resolução nº 196 de 10 de outubro de 1996. Diretrizes e normas regulamentadoras de pesquisa envolvendo seres humanos. Rev bioét. 1996; 4: 15-25.
9.Porcu M, Scantamburlo VM, Albrecht NR, Silva SP, Vallim FL, Araújo CR, et al. Estudo comparativo sobre a prevalência de sintomas depressivos em idosos hospitalizados, institucionalizados e residentes na comunidade. Acta sci. 2002; 24: 713-7.
10.Fernandes MGM, Almeida CB. Processo e pensamento alterado em idosos na vivencia asilar. Nursing. 2001; 4: 22-5.
11.Instituto Brasileiro de Geografia e Estatística (IBGE). Síntese de indicadores sociais: uma análise das condições de vida da população brasileira – 2010. In: Estudos e Pesquisa Demográfica e Socioeconômica. Rio de Janeiro: IBGE; 2010. [citado em 16 out 2012] Disponível em http://www.ibge.gov.br/home/estatistica/populacao/condicaodevida/indicadoresminimos/sinteseindicsociais2010/SIS_2010.pdf
12.Leite VMM, Carvalho EMF, Barreto KML, Falcão IV. Depressão e envelhecimento: estudo nos participantes do Programa Universidade Aberta à Terceira Idade. Rev bras saúde matern infant. 2006; 6: 31-8.
13.Justo LP, Calil HM. Depressão: o mesmo acometimento para homens e mulheres? Rev psiq clin. 2006; 33: 74-9.
14.Xavier FMF, Ferraz MPT, Bertollucci P, Poyares D, Moriguchi EH. Episódio depressivo maior, prevalência e impacto sobre a qualidade de vida, sono e cognição em octogenários. Rev bras psiquiatr. 2001; 23: 62-70.
15.Maciel ACC, Guerra RO. Influência dos fatores biopsicossociais sobre a capacidade funcional de idosos residentes no nordeste do Brasil. Rev bras epidemiol. 2006; 10: 178-89.
16.Veras RP, Coutinho ESF. Estudo de prevalência de depressão e síndrome cerebral orgânica na população de idosos, Brasil. Rev saude publ. 1991; 25: 209-17.
17.Stella F, Gobbi S, Corazza DI, Costa JLR. Depressão no idoso: diagnóstico, tratamento e Benefícios da Atividade Física. Motriz rev educ fís. 2002; 8: 91-8.
18.Carreira L, Botelho MR, Matos PCB, Torres MM, Salci MA. Prevalência de depressão em idosos institucionalizados. Rev enferm UERJ. 2011; 19: 268-73.
19.Stroppa A, Almeida AM. Religiosidade e Saúde. In: Salgado, MIS, Greire, G, organizadores. Saúde e Espiritualidade: uma nova visão da medicina. Belo Horizonte (MG): Inede; 2008. p. 427-43.
20.Duarte MB, Rego MV. Comorbidade entre depressão e doenças clínicas em um ambulatório de geriatria. Cad saude publica. 2007; 23: 691-700.