Source: research data.
Note: (*) p calculated through Chi-square test, significant if p < 0.05.
ORIGINAL RESEARCH
Evaluation of vital signs by the Manchester triage system: expert agreement
Helisamara Mota GuedesI; Cristiane Chaves de Souza II; Domingos Pinto JúniorIII; Sara Salgado de MoraisIV; Tânia Couto Machado ChiancaV
IPhD in Nursing. Professor in the Nursing Department at Universidade
Federal dos Vale do Jequitinhonha e Mucuri. Diamantina, Brazil. E-mail: helisamaraguedes@gmail.com
IIPhD in Nursing. Adjunct Professor in Medicine and Nursing Department at
Universidade Federal de Viçosa. Viçosa, Minas Gerais, Brazil. E-mail: souzac.cris@gmail.com
IIIAssistance Nurse at the Hospital Odilon Behrens. Master in Nursing. Belo
Horizonte, Minas Gerais, Brazil. E-mail: domingoshob@hotmail.com
IVGraduate degree in Nursing at Universidade Federal dos Vales do
Jequitinhonha e Mucuri. Diamantina, Minas Gerais, Brazil. E-mail: sarard1@yahoo.com.br
VPhD in Nursing. Entitled Professor at Nursing School of Universidade
Federal de Minas Gerais. Belo Horizonte, Minas Gerais, Brasil. E-mail: tchianca@enf.ufmg.br
VIThis research counted with resources from FAPEMIG, case number
APQ-01153-12.
DOI: http://dx.doi.org/10.12957/reuerj.2017.7506
ABSTRACT
Objective: to assess expert agreement on the need to measure vital signs and additional data based on the discriminators of Manchester triage system. Method: analytical cross-sectional study conducted in 2012 at the School of Nursing of Minas Gerais Federal University. Participants were three experts selected on predefined criteria, who analyzed the discriminators of the Manchester protocol. Data were analyzed by SPSS (version 17.0) using the Kappa index. The study was approved by COEP-UFMG (CAAE 0430.0.203.000-11). Results: excellent agreement (0.89-0.90) was found between raters and gold standard with regard to the need to measure at least one critical datum. On three (75%) of the four types of vital sign data, agreement between raters was excellent (0.85-1.00) and, on respiratory frequency, agreement between raters was good (0.72-0.79). Conclusion: disagreements on the need to measure vital signs related to discriminators for assessment of respiratory function, which points to the need to review these terms.
Keywords: Triage; emergency medical services; reproducibility of results; classification.
INTRODUCTION
Brazilian emergency services live daily with overcrowding and users who often dispute the service according to the order of arrival to the unit 1. If the severity of the cases is not identified for prioritization care may involve severe damage to the health of the users and can lead to death by negligence2.
To reorganize the work process in the emergency services, the Brazilian Ministry of health points to the use of risk classification as a device for care humanization, proposing to organize it according to the clinical severity presented by the user, and their degree of need/pain. Thus, the risk classification main objectives are: to ensure immediate care to the user with high degree of risk; to inform the patient who is not at immediate risk about the time they will probably wait; to promote teamwork through the continuous assessment of the process; to increase the user's satisfaction, allow and instigate the agreement beyond the construction of internal and external networks of care2,3.
Risk classification must be carried out by nurses, preferably experienced in emergency services and after receiving specific training for such activity. The evaluation of the nurse must be guided by a protocol, which must clearly discriminate the referral to be given to the patient after the classification2,4.
Nurses evaluated that risk classification, in addition to prioritize service to more severe cases, brings more security to the profissional15. However, it is important to note that, for the success of this strategy of the work process reorganization, it is crucial that the health care team is aware of the risk classification protocol used, and the assistance flows established for patient care after the classification6.
Among the many existing risk classification protocols, the Manchester triage system (MTS), widely used in Brazil, stands out. Decision-making using MTS consists of evaluating the main complaint presented by the patient and the signs and symptoms associated with it. The various possibilities of complaints are arranged in a flowchart in MTS and, in each flowchart, there is a set of discriminators that define the classification in different priority levels3. Nurses claim that, when used correctly, the MTS brings benefits to the patient, institution and professional, and point out that the involvement and training of the entire multidisciplinary team about this Protocol is paramount to reduce waiting time for medical care7.
Studies that test the validity of MTS have been developed and the results are favorable to the adoption of it as a risk classification system 8-10. A study that compared the risk classification inter and intra-observer in the Manchester Triage System and the Emergency Severity Index (ESI) found unanimity in the trial of 90% for MTS and 73% for ESI. The divergence level found was 8% and 23% of cases, respectively. It was found that the MTS had a better inter and intra-observer agreement compared to ESI11.
Although it is easy to use, in clinical practice, nurses do not follow a pattern to verify vital signs and additional data as oxygen saturation, blood glucose, using the Glasgow coma scale, among others, when assessing the patient for risk classification using MTS. Studies have been conducted to analyze the influence of physiological patterns in patients' severity analysis, pointing out that the change in some vital data when the patient arrives to the emergency room may interfere with the patient's evolution in the unit12,13. Some MTS flowcharts are clear on the need of measuring vital signs and specific additional data, such as the hot adult discriminator, which requires to check the body temperature to confirm its presence. However, other discriminators leave doubts as to whether it is needed to measure vital signs and additional data, with reference to each discriminator definition established.
Thus, the objective of this study is to evaluate the specialists' agreement on the need for measurement of vital signs and additional data, with reference to the discriminators definition described in MTS. This study is justified since the guiding protocol is the legal support in which the nurse is based for clinical decision-making on risk classification. Because it is a protocol that has been widely used in Brazil and in other countries, studies that assess MTS are important to make it a reliable instrument to use in nurses' clinical practice.
THEORETICAL FRAMEWORK
The MTS is a protocol of English origin, which stratifies the risk of patients in five priority levels. For each priority level is set a color for sorting and a target time for medical attention: level 1 – red – immediate; level 2 – orange – assistance in up to 10 minutes; level 3 – yellow – assistance in up to 1 hour; level 4 – green – assistance in up to 2 hours and level 5– blue – assistance in up to 4 hours3.
The MTS was introduced in the United Kingdom in 1996, translated into Portuguese of Portugal in the year 2000, by the Portuguese triage group and it is currently used universally throughout the United Kingdom and in many hospitals in Europe5. Through internationalization it was possible to test the MTS and adapt it to different cultures, validating the quality parameters and the management model of emergency services in countries such as Australia, New Zealand, the Netherlands, Germany, Italy, Japan and Canada3.
To carry out the risk classification, the health professional sets the complaint or the reason why the patient is at the emergency service, selects one of the 52 performances and identify the signs and symptoms in each clinical priority level. Each clinical priority level shows signs and symptoms that discriminate them, named discriminators and presented in the form of flowcharts for the clinical condition presented. When performing the classification, the discriminators that indicate higher priority levels are the first to be identified, the absence of relevant discriminators will allocate most of the patients classified as non-urgent3.
METHODOLOGY
It is an analytical cross-sectional study to verify the specialists' degree of agreement about the need of evaluating vital signs and additional data on different MTS discriminators.
Three specialists who met the following inclusion criteria participated in this study: being an expert in urgency and emergency area, having a master degree or PhD in nursing, and research in the field of urgency and emergency and MTS. It was ranked as a gold standard of the study the specialist who, in addition to the inclusion criteria, held training for the use of the MTS and has used in clinical practice for at least two years.
Data were collected in November 2012 at the nursing school of the Federal University of Minas Gerais and consisted in the analysis of MTS discriminators, to verify those who require verification of vital signs and/or additional data. It is noteworthy that was defined as vital signs data, blood pressure, heart rate, respiratory rate and body temperature and as additional data, those relating to the oxygen saturation, capillary glycaemia, pain scale, expiratory flow pressure (EFP) and Glasgow coma scale (GCS).
For data collection, we used an instrument that contained a table to identify, according to each MTS discriminator, the need for vital data and additional data measurement. For each discriminator, the specialists gave their opinions on the need for evaluation of these data in patients, having as a reference just the concept of discriminator established in the MTS 3. The evaluators' shield criterion was followed, that is, independent assessment, during which all the specialists had the MTS printed to check each discriminator definition.
Data were analyzed in the SPSS program, version 17.0. The degree of agreement among the specialists on the need of vital and additional data evaluation on each MTS discriminator was measured by calculating Cohen's Kappa index, which measures the degree of agreement beyond that expected by chance. The kappa index is a statistical measure more widely accepted to assess inter-observers agreement14. Convention, the kappa index is not expressed as a percentage, but as probability15,16. The kappa can range from 0 to 1, being 1 when the agreement is perfect or complete and zero when level of agreement expected is just due to chance. This study considered bad agreement when Kappa index values were between 0 and 0.20, weak (between 0.21 and 0.40), medium (between 0.41 and 0.60), good (0.61 and 0.80) and excellent (between 0.81 and 1)15.
This research complies with the 196/96 Resolution of the National Council on health research involving humans, approved by the Research Ethics Committee of the UFMG (COEP-UFMG-CAAE-0430.0.203.000-11). Before data collection, study participants were invited to participate in the research, explained their objectives and signed an informed consent term.
RESULTS AND DISCUSSION
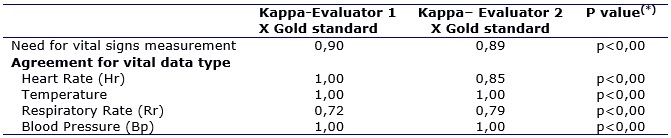
192 (100%) MTS discriminators were analyzed. Of these, according to the gold standard, 15 (7.81%) require evaluation of at least one type of vital sign. The correlation between the gold standard and evaluators 1 and 2 about the need for vital signs measurement showed that there was excellent agreement between the evaluators and the gold standard about the need for measuring at least one vital data (Kappa between 0,89-0.90), following the MTS discriminators definition. In three (75%) of the four types of vital data, the correlation between evaluators was excellent (0.85-1.00), and given vital respiratory rate, the correlation among raters was good (0.72-0.79). These differences were detected in the following discriminators: exhaustion,breathing after airway opening, inadequate breathing and signs of severe pain, as shown in Table 1.
TABLE 1:
agreement between evaluators according to the need vital signs for
measurement. Belo Horizonte, 2012.
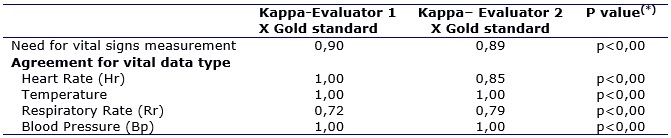
Source: research data.
Note: (*) p calculated through Chi-square test, significant if p
< 0.05.
It was noticed that most of the discriminators that presented disagreement on the need for vital signs measurement are related to the respiratory function assessment. The discriminator Exhaustion refers to patients in respiratory exhaustion with ventilatory effort reduction, although remain in respiratory failure. The discriminator Breathe after airway opening is used in multiple situations where victims should be evaluated for the presence of breath after airway opening. The absence of breath for 10 seconds after airway opening implies death, unless there are resources for cardiopulmonary resuscitation without impairing caring of other victims classified as red. The Inadequate breathing discriminator is defined for patients who cannot breathe enough to maintain adequate oxygenation . There may be an increase in breathing work, signs of inadequate respiration or exhaustion . The intense pain signals discriminator is used in the classification of small children and babies that can't describe the pain and may show signs as continuous and inconsolable crying, tachycardia, pallor and sweating3.
A study on the working satisfaction of nurses during the risk classification using the MTS in emergency services of Sweden showed a high degree of satisfaction with their work (88%). Most nurses reported that the MTS was a clear and direct method, but needs to be improved. The experience of the nurse at the time of triage contributes to patient safety in emergency services. However, an experienced nurse may not notice important parameters due to overconfidence in their thinking17.
About the need for the evaluation of additional data, the gold standard nurse pointed out that in 18 (9.37%) discriminators, there is a need for measuring at least one further data. The correlation between the evaluators and the gold standard, according to the need of measuring each data evaluated, showed that in four (80%) of the additional data, the correlation was excellent (0.82-1.00). However, for oxygen saturation data, the correlation between evaluators ranged from average to good (0.56-0.79). These disagreements were identified in the discriminators shock, inadequate breathing and acute dyspnea, as shown in Table 2.
TABLE 2:
agreement between evaluators according to the need for additional data
measurement. Belo Horizonte, 2012.
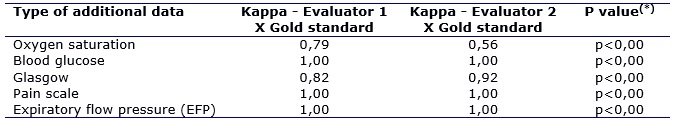
Source: research data.
Note: (*) p calculated through Chi-square test, significant if p
< 0.05.
It calls our attention the fact that, as well as on the need for vital signs measurement, disagreements over the need for additional data evaluation also refer to discriminators associated with the respiratory function. Shock is defined as the inadequate oxygenation of the tissues that result in poor tissue perfusion, which can be accompanied by signs such as sweating, pallor, tachycardia, hypotension, and decreased level of consciousness. Acute dyspnea refers toshort breath or sudden lack of air or sudden worsening of chronic short breath3.
It was also verified the agreement between the evaluators in each of the 192 MTS discriminators concerning the need for measurement of vital data and additional data, which ranged from excellent (kappa = 1.00) to bad (kappa = 0) in seven (3.64%) discriminators. It draws our attention the fact that the greatest disagreements refer to data related to the assessment of respiratory function. Disagreements regarding the evaluation of oxygen saturation represented 42.85% of the differences found, as well as the evaluation of FR (3-42.85%), as shown in Table 3.
TABLE 3:
Disagreement between evaluators according discriminators of the Manchester
Protocol. Belo Horizonte, 2012.
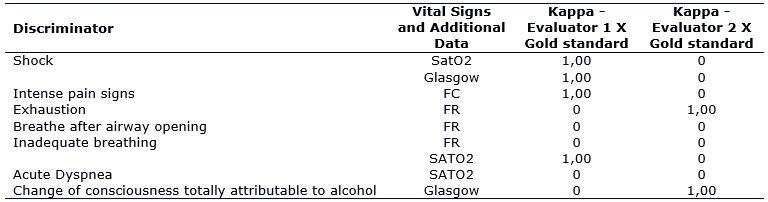
Source: research data.
When questioned as to the need for inclusion of vital data and additional data for better measure the discriminators, the evaluators pointed to the need of evaluating any further data for every discriminator, according to their clinical perception. However, the experts agreed on the need for oxygen saturation verification when evaluating the clinical discriminator jumbled sentences.
A study conducted in the United Kingdom showed that it is not known whether a screening system based on physiological parameters would be able to identify patients at risk of admission to intensive care better than MTS or provide additional information about the seriousness of the condition 12.
Other scales of triage indicated the measurement of vital signs in the process of assessment and risk classification, such as the instruments Risk Classification in Pediatrics (CLARIPED), designed for use in pediatric emergencies. Following this protocol, one of the steps in the risk classification is the measurement of respiratory rate, heart rate, oxygen saturation, and skin temperature. Studies that check the validity and reliability of this instrument are ongoing18.
Thus, there is a need to conduct studies to assess whether the assessment of vital signs and additional data on risk classification is able to predict clinical outcomes as severity level, length of stay in hospital and mortality.
Nevertheless, it is worth mentioning that, in general, the MTS has proven a reliable instrument to classify the risk of patients in emergency services, and when the higher the experience of nurses and the closer the use of the protocol origin country, the greater this reliability19. In addition, its use has extrapolated the primary objective of classifying patients about clinical risk. A study in Germany showed that the higher the risk level of the patient, the greater the time of nursing care necessary and, from that, it was developed a formula to calculate of nursing staff dimension in emergency units, taking into consideration the MTS risk classification20. Finally, the MTS is proved to be a good predictor of the need for hospitalization, mortality, and use of social resources, becoming an important managerial tool in addition to the risk classification21.
CONCLUSION
The findings of this study indicate that the operational definition of some of the MTS discriminators cause disagreement among evaluators regarding the need for vital signs evaluation, which can lead to an individual behavior of nurses working in risk classification. It is valid to note that MTS is being used in several countries, but we don't know about published studies that have investigated the suitability of it for each of the different scenarios in which it is used.
Among the limitations of this study, we include the difficulties related to the assessment of respiratory function, that are attributed to the operational definition of the discriminators. Thus, we suggest carrying out similar studies using the MTS in other locations to refine this instrument as a support for nurses' decision making in emergency services.
Finally, it is acknowledged that the MTS has represented an aid to clinical practice of nurses who work on risk classification. However, it is clear the need for submitting the protocol to cultural adaptation and validation to use it in Brazil, which could clarify the discriminators definition and increase the reliability of the protocol, in particular about the vital signs need for measurement evaluation.
REFERENCES
1.Nascimento ERP, Hilsendeger BR, Neth C, Belaver GM, Bertoncello KCG. Risk classification in emergency: evaluation of nursing staff.Rev enferm UERJ. 2011; 19(1):84-8.
2. Ministry of health (Br). National policy of SUS humanization and management of care. Reception and risk classification in emergency services [Internet website] 2009 [cited in 27 março 2016]. Available in: http://bvsms.saude.gov.br/bvs/publicacoes/acolhimentoclassificacaoriscosevicourgencia.pdf
3.Mackway-Jones K, Marsden J, Windle J. Brazilian Risk Classification group. Manchester system of risk classification. 2ª ed. Belo Horizonte (MG): 2010.
4.Christ M, Grossmann F, Winter D, Bingisser R, Platz E. Modern Triage in the Emergency Department. Dtsch Arztebl Int. 2010; 107(50):892–8.
5.Herminda PMV, Jung W, Nascimento ERP, Silveira NR, Alves DLF, Benfatto TB. Risk classification in ER unit: speeches of the nurses. Rev enferm UERJ. 2017; 25:e19649.
6.Júnior JAB, Viturill DW, Versall LGS, Furuya PS, Vidor RC, Matsuda LM. Reception with risk classification in hospital emergency service: assessment of the process. Rev enferm UERJ. 2015; 23(1):82-7.
7.Marculino LMG, Noronha MRG, Monteiro MGS, Abreu RNDC, Silva FC, Carvalho ZMF. Nursing knowledge and practices about the Manchester risk rating system. Rev enferm UFPE on line. 2015; 9(10):9462-8.
8.Santos AP, Freitas P, Martins HM. Manchester triage system version II and resource utilisation in emergency department. Emerg Med J. 2014; 31(2):148-52.
9.Pinto JD, Salgado PO, Chianca TCM. Predictive validity of the Manchester Triage System: evaluation of outcomes of patients admitted to an emergency department. Rev Lat Am Enfermagem. 2012; 20(6): 1041-7.
10.Guedes HM, Martins J CA, Chianca TCM. Predictive value of the Manchester Triage System: evaluation of clinical outcomes of patients. Rev bras enferm. 2015,68(1):45-51.
11.Storm-Versloot MN, Ubbink DT, Choi VCA, Luitse JSK. Observer agreement of the Manchester Triage System and the Emergency Severity Index: a simulation study. Emerg Med J. 2009; 26(8): 556-60.
12.Subbe CP, Slater A, Menon D, Gemmell L. Validation of physiological scoring systems in the accident and emergency department. Emerg Med J. 2006; 23(11): 841-5.
13.Merz TM, Etter R, Mende L, Barthelmes D, Wiegand J, Martinolli L, et al. Risk assessment in the first fifteen minutes: a prospective cohort study of a simple physiological scoring system in the emergency department. Crit Care. 2011; 15(1): R25.
14.Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ. 1992; 304:1491-4.
15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics
1977; 33: 159-74.
16.Silcocks P. Some issues in observer error studies in pathology J Pathol. 1992; 168(3): 255-6.
17.Forsgren S, Forsman B, Carlstrom ED. Working with Manchester triage – Job satisfaction in nursing. Int Emerg Nurs. 2009; 17(4):226-32.
18.Magalhães-Barbosa MC, Prata-Barbosa A, Cunha AJLA, Lopes CS. CLARIPED: a new tool for risk classification in pediatric emergencies. Rev paul Pediatr. 2016; 34(3):254-62.
19.Mirhaghi A, Mazlom R, Heydari A, Ebrahimi M. The Reliability of the Manchester Triage System (MTS): A Meta-analysis. J Evid Based Med. 2016; Sep.9. doi: http://dx.doi.org/10.1111/jebm.12231
20.Gräff I, Goldschmidt B, Glien P, Klockner S, Erdfelder F, Schiefer JL, et al. Nurse Staffing Calculation in the Emergency Department - Performance-Oriented Calculation Based on the Manchester Triage System at the University Hospital Bonn. PLoS One. 2016; 11(5):e0154344.
21.Zachariasse JM, Seiger N, Rood PPM, Alves CF, Freitas P, Smit FJ, et al. () Validity of the Manchester Triage System in emergency care: a prospective observational study. PLoS ONE 2017; 12(2):e0170811. https://doi.org/10.1371/journal.pone.0170811