RESEARCH ARTICLES
Condom use among goers of a motel
Helisamara Mota GuedesI; Gisele Almeida SilvaII; Patrícia de Oliveira SalgadoIII; Tânia Couto Machado ChiancaIV; Marília AlvesV
INurse. Doctorate’s Student in Nursing from the Federal University of Minas Gerais. Assistant Professor from the Nursing Department at the Federal University of the Mucuri and Jequitinhonha Valley. Diamantina, Minas Gerais, Brazil. E-mail: helisamaraguedes@gmail.com.
IIGraduating Student of the 8th period of the Nursing Course at the University Center of East of Minas Gerais. Ipatinga, Minas Gerais, Brazil. E-mail: giselealm@facebook.com
IIINurse. Doctorate’s Student in Nursing from the Federal University of Minas Gerais. Professor from the Medicine and Nursing Department at the Federal University of Viçosa. Belo Horizonte, Minas Gerais, Brazil. E-mail: patriciaoliveirasalgado@gmail.com
IVNurse. PHD in Nursing. Titular Professor from the Nursing School at the Federal University of Minas Gerais. Belo Horizonte, Minas Gerais, Brazil. E-mail: tchianca@enf.ufmg.br
VNurse. PHD in Nursing. Titular Professor from the Nursing School at the Federal University of Minas Gerais. Belo Horizonte, Minas Gerais, Brazil. E-mail: marilix@enf.ufmg.br.
ABSTRACT: This is a descriptive study aimed at analyzing the profile of goers of a motel in the city of Ipatinga, Minas Gerais State, Brazil, and verifying the use of condoms among them. The sample was comprised of 154 people. The data collection was conducted through a questionnaire in the year 2009. For data analysis, we have used the descriptive statistics. According to the results, 50,7% were female, 60,5% had less than 30 years of age and showed early sexual initiation (average 15,9 years); 73,4% were single; 70,8% of customers considered as remote the possibility of acquiring the Human Immunodeficiency Virus (HIV) in their sexual practices and 76,0% reported having no difficulty in proposing the use of condoms to their partners. It is suggested that health care professionals develop strategies that might guarantee to the individual and the community a care of excellence in the prevention and control of the HIV and the Acquired Immunodeficiency Syndrome.
Keywords: Acquired Immunodeficiency Syndrome; sexual behavior; vulnerability; condoms.
INTRODUCTION
Since its discovery, the infection caused by the Human Immunodeficiency Virus (HIV) has been changing in Brazil and in the world in relation to the epidemiological profile and the natural history. This feature imposes significant challenges, both for its prevention and for the integral health care of the affected individuals1.
It is observed, in a broad social and geographical perspective, the spread of the epidemic for a growing number of municipalities far from major metropolitan areas, reaching strongly those people living in less assisted communities.
There is an epidemic by region over a period of 10 years (2000-2010), in which the incidence rate fell in the Southeast from 24,5 to 17,6 cases per 100 000 inhabitants. Nonetheless, in other Brazilian regions this rate has grown: 27,1 to 28,8 in the South; 7,0 to 20,6 in the North; 13,9 to 15,7 in the Midwest; and from 7,1 to 12,6 in the Northeast. It should be highlighted that the highest number of cumulative cases is concentrated in the Southeast Region (56%)2.
According to notified data, in the Southeast Region there are 343.095 cases of people affected by Acquired Immunodeficiency Syndrome (AIDS) accumulated in the period between 1980 and 2011, being that 42.283 cases were reported in the Minas Gerais State. In this Brazilian State, although it has also a concentration of cases in big cities, in the year 2008, AIDS cases were reported in 670 of the 853 municipalities3. This reality includes the city of Ipatinga, which is located in the East Region of Minas Gerais. According to the Support Group for Seropositive People (known as GASP) of the Municipal Program for Sexually Transmitted Diseases (STDs)/AIDS of the city in question, the number of people with HIV in the region of Vale do Aço (Steel Valley) in 2007 increased by 29,8%, compared to the year 2006. It is estimated that, in the region at stake, approximately five thousand people are infected by the virus and do not know of it4.
Study held in the databases of Research on Sexual Behavior and Perceptions of the Population, in the years 1998 and 2005, showed an increase in the level of information of the population in relation to the use of male or female condoms, i.e., the percentage of people who were well-informed jumped from 69,2% to 90,2%. In 2005, there were no significant differences between men and women in relation to knowledge and risk perception on HIV/AIDS. However, the most educated people had higher level of information and risk perception. As to the level of knowledge of the population, the lack of significant growth in the level of knowledge about AIDS among young people from 16 to 24 years deserves specific attention5.
Currently, the biggest challenge of the Brazilian Ministry of Health (MS) and of the Department of STDs, AIDS and Viral Hepatitis of the Ministry of Health is to raise greater awareness and autonomy of the Brazilian population for the incorporation of new attitudes towards the vulnerability to the HIV infection, as well as the STDs6. This vulnerability considers that the chance of people's exposure to illness is the result of a set of aspects not only individual, but also collective, which involve the context7.
In order to reduce the vulnerability, the Brazilian Ministry of Health has been campaigning for the free distribution of condoms, but this distribution does not ensure the use by people.
Condom use is one of the most important measures in the fight against AIDS8. Laboratory and epidemiological studies show that the condom is effective against a broad variety of STDs, including the HIV infection. Nevertheless, there is still resistance to its use, both by men and by women9.
It becomes necessary to perform a differentiated work in places frequented by heterosexual and homosexual couples, with the aim of suggesting the development of health education programs. Furthermore, there are few studies in the literature with a sample of motels’ goers, considering that this kind of establishment attracts a diversified audience with regard to sexual orientation, age, gender, marital status, among other features, and that the condom is paid in many of these places, which might hinder the use10.
This study becomes relevant because it allows health care professionals to realize the emerging necessity to improve the care provided to the community, focusing on risk behaviors and vulnerability. In addition to providing data that might be compared to new studies and subsidize the planning of actions for preventing HIV/AIDS, including the provision of free condoms in motels.
Accordingly, the study aimed at analyzing the profile of goers of a motel in the city of Ipatinga, Minas Gerais State, Brazil, and verifying the use of condoms among them.
LITERATURE REVIEW
The location where the sexual scene takes place is crucial (street, drive-in, motel, home). The different scenarios might facilitate or hinder the use of condoms11,12. Most reserved places, i.e., private, where the individual has more privacy, offer less difficulty for using condom13.
In Brazil, in 2011, there were about 5.000 motels, being that they moved about four billion of reais (Brazilian currency) in the economy. The Brazilian motels are frequented by more than 100 million customers every year. By analyzing the trends of sophisticated motels, the growing purchasing power of Brazilians and the habits of the population, it is estimated that the potential market is about 15 billion of reais within ten years. These indexes represent an annual growth of 27% in the billing of Brazilian motels and of 11% in the amount of served annually customers14.
There are many variables that interfere with the use of condoms, being that some of them are cultural and gender issues, confidence in the steady partner, hierarchization of the affective-sexual relationship, early sexual practice, difficulty in proposing the use, low schooling, use of drugs and alcoholic beverages5,10 15-17, among others.
One research conducted at two motels revealed that approximately half of the participants did not use a condom at the last vaginal or oral intercourse. It was found no significant association between the amount of partners and the condom use (p=0,07), and between the condom use and the length of relationship (p=0,333). Nonetheless, the main determinant variable for not using condoms was the fact of having a steady partner (p=0,04), given that the probability of condom use is reduced by 55% in cases of steady partners compared to those without a steady partner10.
METHODOLOGY
This is a study with a quantitative approach of the descriptive type, performed in a motel in the city of Ipatinga/MG/Brazil.
The sample for this study was calculated based on a previous pilot study and had the following inclusion criteria: customers who were in the studied place to have sexual intercourse and aged over 18 years. As to the exclusion criteria, we have considered: customers who did not accept to participate in the study. For the statistical calculation of sample, we used the monthly average of motel’s goers, and for processing, we used the program Diman 1.0, with an error margin of 5%, confidence level of 95% and interest proportion of 14%, thus obtaining a sample of 154 people.
The data collection was conducted in April 2009, through a questionnaire comprised of clear and objective questions, with open and closed questions. The questions covered sociodemographic data, such as: age, gender, marital status, age at the first sexual intercourse, in addition to questions about condom use at the last sexual intercourse, time with that partner, number of partners in the last six months, frequency of condom use in vaginal, oral and anal intercourses, perception about the possibility of acquiring HIV, perceived difficulty in proposing to the partner to use condom.
The questionnaire was made available in roulette, together with the customer's account. This is the location used in motels for passing of customers and receiving accounts, in which there is no contact with customers. The questionnaire was focused on the last sexual intercourse of the person and requested that only a person who was in the room responded to the instrument. The time spent, estimated, to answer the questionnaire was calculated for being around three minutes, and it has been informed by telephone that there was a tolerance time of five minutes to exit the site after payment of the account.
The research project was presented, through a meeting, to the owner of the establishment and to the employees of general services: telephonists and liberists (people responsible for delivering and receiving the account, besides verifying the consumption in the rooms). The motel's telephonists were responsible for the succinct presentation of the research, the study objective and the questionnaire, at the time in which the customer called to request the bill. The delivery of questionnaires to the customers was a task of the liberists.
The monitoring of the provision of information and gathering of the questionnaires were performed by one of the researchers.
The collected data were analyzed by means of descriptive statistics with presentation of absolute frequencies and percentages, as well as calculation of the arithmetic average and standard deviation.
The study was approved by the Research Ethics Committee (REC) of Unileste/MG, under the protocol number 2112508. It has contemplated the Resolution 196/96 of the National Health Council, which regulates the researches involving human beings. We have guaranteed confidentiality and anonymity and under no circumstance the participants were identified. It is noteworthy that the REC has waived the use of the Free and Informed Consent Form (FICF), by considering that its signature would identify the participants.
RESULTS
Among the 154 people who formed the sample, 78 (50,7%) were female and 76 (49,3%) were male. The age of first sexual intercourse ranged between 11 and 20 years, with an average of 15,9 years and standard deviation of 0,05 years.
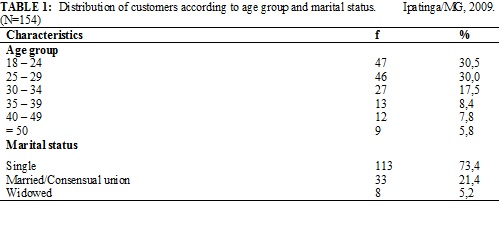
Of the surveyed participants, 93 (60,5%) had less than 30 years. With regard to marital status, the majority, 113 (73,4%), is single, followed by 33 (21,4%) customers in a consensual union, as shown in Table 1.
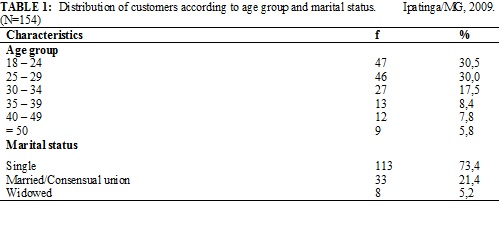
With the purpose of assessing the frequency of risk behaviors for HIV/AIDS, characteristics of sexual practices considered risky were identified, as can be seen in Table 2.
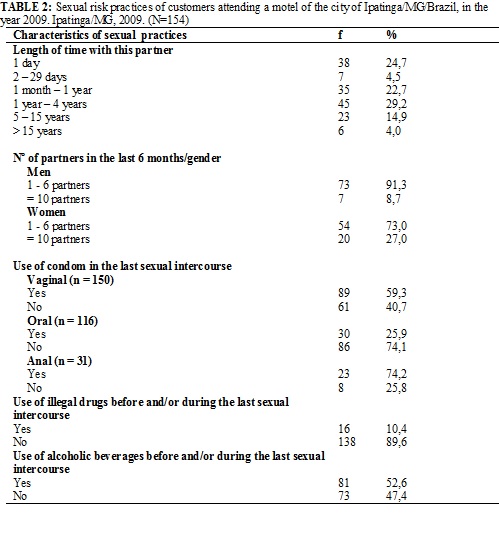
Regarding the reference about the partner with whom they were on the day of data collection, 96 (62,3%) were steady partners and 58 (37,7%) were casual partners. It was found that 80 (51,9%) customers were with their partners for less than 1 year, being that 38 (24,7%) knew him/her only a day ago.
When asking about the use and sharing of drugs (by using shared syringe, pipe or tube) before and / or during the last sexual intercourse, 138 (89,6%) customers have denied their use. However, 81 (52,6%) admitted using alcohol before and/or during the last sexual intercourse.
From the evaluation of the frequency of risk behaviors for HIV/AIDS, we have investigated the perception of vulnerability of these people towards the HIV and the condom use, as shown in Table 3.
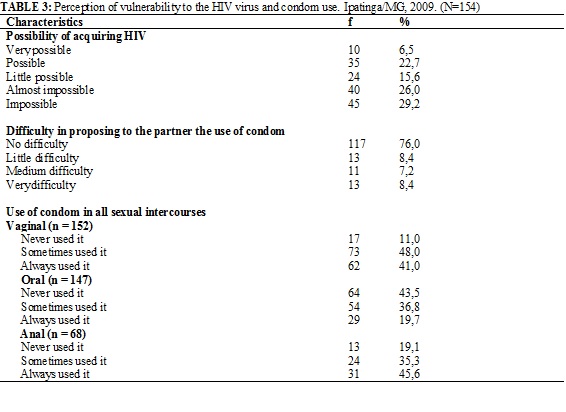
When asked about the possibility of acquiring HIV in their sexual practices, 109 (70,8%) customers (sum) consider this possibility as remote. Most people, 117 (76,0%), claimed to have no difficulty in proposing the use of condoms to their partners.
Regarding the use of condoms during sexual intercourses of people in different moments of life, it was found that 73 (48,0%) reported that in some vaginal intercourses had used a condom; most of the respondents, 64 (43,5% ), stated they never used condoms during oral sexual intercourses and 31 (45,6%) reported had always used a condom in anal intercourses.
DISCUSSION
The population of young people between 15 and 24 years is identified as an important population group in terms of epidemiological risk for sexually transmitted diseases and is defined as the priority of prevention campaigns held by the United Nations Organization18. This fact is related to the association between behavior at the first sexual intercourse and the establishment of behavioral patterns that might remain for the whole life. Moreover, there is the identification that the onset of sexual activity by very young people would be a risk factor for teenage pregnancy and acquisition of STDs, including HIV19.
In this study, 60,5% of customers who formed the sample were aged between 18 and 29 years, being that 30,5% correspond to the age group between 18 and 24 years. The sexual practice in youth has occurred increasingly earlier. As the results of this study, the found average age of the first sexual intercourse was 15,9 years, which did not vary from the average achieved in a study conducted in São Paulo, in the year 2002 (15,1 years)20.
It was found a large number of single people, 113 (73,4%), and with steady partners, 96 (62,3%), but condom use does not exceed 60% in sexual intercourses. Studies show an increased exposure to STDs/AIDS, given that these partners, in their great majority, discontinue use of condoms after a certain time of relationship, due to the fact that people start, most often, to put confidence in the other5,10,15,16.
One study held in the Federal District of Brazil with heterosexual men and women, married or in a consensual union, showed that they had important knowledge about transmission of HIV/AIDS. Nevertheless, this fact does not ensure the condom use, since their marital perceptions express the culture in which they are inserted with regard to gender roles and hierarchization of the affective-sexual relationship, which makes them vulnerable to the HIV infection15.
Historically, the non-use of condom in relationships with steady partners is attributed to the prejudice that its use is associated with prostitution, promiscuity and extramarital relationships. On the other hand, the non-use of condom with steady partners is often mistakenly considered by couples as a way to demonstrate loyalty15.
Another study showed that, in relation to married/consensual unions, the condom use decreased with age, from 17,3% in the age group between 16 and 24 years to 7,1% in the range between 45 and 65 years, among singles. This decrease is observed from the age group between 35 and 44 years. The condom use among men was 9,1% among married/cohabiting partners, 27,3% among widowed/separated/divorced and 52,8% among single. Furthermore, for the total of people who are sexually related, only with eventual partners, the consistent condom use in the 12 months preceding the interview was 65,0%15.
Still on the use of condoms during sexual intercourses, it was observed that the later sexual initiation for both sexes is essential in determining the continuity of condom use, the more delayed is the onset of sexual activity, the greater the maturity and the greater the ability of communication between the sexual partners11,21. In the present study, this fact is demonstrated as it was found that the average age of the first sexual intercourse was 15,89 years, besides a low rate of condom use during sexual intercourses (vaginal and oral) in the lifetime.
As to the condom use at the last sexual intercourse, 59,3% of customers of the present research reported having used it in vaginal intercourse and 74,2% reported its use in anal sex. In a study16 that analyzed trends of condom use in the Brazilian urban population between 1998 and 2005, it was found that 41,8% used condoms in the practice of vaginal and anal sex, 4,9% used it only in one of them and 53,3% did not use it in both practices. The behaviors differed with regard to the type of partnership, with a greater frequency (59.5%) of condom use in both practices when the sexual intercourse was with an eventual partner, in contrast to 32,6%, when the intercourse was referring to a stable partner.
The categories of vulnerability to the HIV infection were found in this study. The preventive behaviors are not practiced in large part of situations, especially in people living in steady relationships (individual vulnerability). The data indicate low condom use, despite 76% refer that they do not have any difficulty to propose the condom use and 70.8% mention having a remote possibility of acquiring HIV (social vulnerability). The culturally constructed gender relationships interfere with the adherence to condom use by individuals (cultural vulnerability).
Breaking the published data in the literature that point the alcohol consumption as factor that increases the vulnerability to sexual intercourses without condoms22, in this present paper 89 (59,3%) people reported having used a condom at the last vaginal intercourse, even with the use of alcoholic beverage - 81 (52,6%).
The use of alcohol and illegal drugs is an important factor in the analysis of sexual behavior of people and in preventing the transmission of AIDS, not only by direct infection of the virus by sharing equipment used during their consumption, but also by the action of psychoactive substances that act by altering behaviors, reducing the ability of reasoning and of decision-making of individuals for adopting preventive sexual practices, such as condom use23.
It is interesting to note that 16 (10,4%) customers have confirmed drug use in the period in which they were at the motel.
Regarding the perception of the study subjects about the possibility of acquiring HIV, 45 (29,2%) reported being impossible. It should be emphasized that the simple knowledge about prevention of the HIV infection is not sufficient to reduce the vulnerability to the virus. This knowledge needs to be of interest to the individual, assimilated and put into practice, besides the availability of resources, such as educational actions and public policy programs on HIV/AIDS for the adoption of new sexual behaviors5.
The results of this study have shown a significant increase in condom use in the last few years, which is an outcome of the efforts of the official prevention programs of STDs/AIDS. On the other hand, the systematic differential of schooling in the condom use unveils the need for further reflection on policies on access to information about prevention actions targeted to people with lower education level. Similarly, it is necessary to deepen the discussion on actions aimed at increasing the consistent condom use, especially among most vulnerable populations, such as young women or those who reveal stable partnerships.
CONCLUSION
The conduction of this research in a motel showed that this place is privileged to reduce the possibility of recall bias, since it has questioned about the last sexual intercourse. The results of this study show that the majority of customers attending a motel in the city of Ipatinga, Minas Gerais State, reported condom use during vaginal and anal intercourses. It was observed that most of the sample was composed of young people, less than 30 years old, with early initiation of sexual life (in adolescence) and single.
It is highlighted as limitations of the study the fact that the collected data represent the reality of only one motel in a city of the countryside of Minas Gerais, which prevents external validity of this study. However, the study unveils multiple causes around the non-use of condoms, which makes individuals vulnerable to HIV/AIDS. The fact that the study show that the majority has no difficulty in proposing such use makes that the challenge for health care professionals is to encourage people to put into practice the knowledge that they hold.
Thus, it is suggested that the health care professionals act more assertively together with the Municipal Health Department of the municipalities, seeking to build and develop strategies, such as, for example, free distribution of condoms and booklets in establishments like motels, as well as performing educational activities about STDs prevention at all levels of health care, with a view to ensuring to the individual and the community a care of excellence in the prevention and control of this epidemic.
REFERENCES
1. Reis RK, Gir E. Convivendo com a diferença: o impacto da sorodiscordância na vida afetivo-sexual de portadores do HIV/AIDS. Rev esc enferm USP. 2010; 44:759-65.
2. Ministério da Saúde (Br). AIDS no Brasil. Vulnerabilidade à AIDS em jovens gays [site de Internet]. Epidemia estabilizada e concentrada em populações de maior vulnerabilidade. Departamento de DST, AIDS e Hepatites Virais/SVS/MS. [citado em 20 out 2012] Available at: http://www.aids.gov.br/sites/default/files/anexos/publicacao/2011/50652/resumo_anal_tico_dos_dados_do_boletim_epidemiol__92824.pdf
3. Secretária do Estado de Saúde de Minas Gerais [site de Internet]. Boletim Epidemiológico Maio/Junho 2009. [citado em 18 mai 2011] Available at: http://www.saude.mg.gov.br/publicacoes/estatistica-e-informacao-em-saude/boletim-epidemiologico/2009/Boletim%20Epidemiologico_Ano7_N3.pdf
4. Leite R. Prevenção positiva Ipatinga (MG): Grupo de Apoio aos Soros Positivos – GASP [site de Internet]. [citado em 9 mar 2011] Available at: http://ppgasp.blogspot.com/2008/09/dstaids-no-vale-do-ao.html
5. Ferreira MP. Nível de conhecimento e percepção de risco da população brasileira sobre o HIV/AIDS, 1998 e 2005. Rev Saúde Pública. 2008; 42:65-71.
6. Souza V, Czeresnia D. Considerações sobre os discursos do aconselhamento nos centros de testagem anti-HIV. Interface: Comunic, Saúde, Educ. 2007; 11:531-48.
7. Bertolozzi MR, Nichiata LYI, Takahashi RF, Ciosak SI, Hino P, Val LF et al. Os conceitos de vulnerabilidade e adesão na saúde coletiva. Rev esc enferm USP. 2009; 43:1326-30.
8. Silveira MF, Santos I. Impacto de intervenções no uso de preservativos em portadores do HIV. Rev Saude Pública. 2005; 39:296-304.
9. Madureira VSF, Trentini M. Da utilização do preservativo masculino à prevenção de DST/AIDS. Ciênc saúde coletiva. 2008; 13:1807-16.
10. Guedes HM, Cabral LOC, Costa MVB, Reis AF, Pereira SG, Oliveira-Ferreira F. Risk behavior for the Human Immunodeficiency Virus among motel clients. Rev Latino-Am Enfermagem. 2012; 20:536-42.
11. Paiva VSF. Fazendo arte com camisinha-sexualidades jovens em tempos de AIDS. São Paulo: Summus; 2000.
12. Paiva VSF. Sem mágicas soluções: a prevenção e o cuidado em HIV/AIDS e o processo de emancipação psicossocial. Interface. 2002; 6:25-38.
13. Antunes MC. Territórios de vulnerabilidade ao HIV: homossexualidades masculinas em São Paulo [tese de doutorado]. São Paulo: Universidade de São Paulo; 2005.
14. Roveda VS. Os motéis no Brasil: origem e mercado. Zeax Expertise em Motéis [site de Internet]. [citado em 04 jun 2012] Available at: http://zeaxmoteis.com.br/publicacoes
15. Araujo TME, Monteiro CFS, Mesquista GV, Alves ELM, Carvalho KM, Monteiro RM. Fatores de risco para infecção por HIV em adolescentes. Rev enferm UERJ. 2012; 20:242-7.
16. Paiva V, Calazans G, Venturi G, Dias R. Idade e uso de preservativo na iniciação sexual de adolescentes brasileiros. Rev Saúde Pública. 2008; 42:45-53.
17. Teixeira AMFB, Knauth DR, Fachel JMG, Leal AF. Adolescentes e uso de preservativos: as escolhas de jovens de três capitais brasileiras na iniciação e na última relação sexual. Cad Saude Pública. 2006; 22:1385-96.
18. Borges ALV, Schor N. Início da vida sexual na adolescência e relações de gênero: um estudo transversal em São Paulo, Brasil, 2002. Cad Saúde Pública. 2005; 21:499-507.
19. Maia C, Guilhem D, Freitas D. Vulnerabilidade ao HIV/AIDS de pessoas heterossexuais casadas ou em união estável. Rev Saúde Pública. 2008; 42:242-8.
20. Berquó E, Barbosa RM, Lima LP. Uso do preservativo: tendências entre 1998 e 2005 na população brasileira. Rev Saúde Pública. 2008; 42:34-44.
21. Heilborn ML, Cabral CS, Bozon M. Gênero e carreiras sexuais e reprodutivas de jovens brasileiros. [site de Internet] Associação Brasileira de Estudos Populacionais (ABEP). XVI Encontro Nacional de Estudos Populacionais. [citado em 15 ago 2011] Available at: http://www.abep.org.br/usuario/GerenciaNavegacao.php?caderno_id=030&busca=Pesquisar&caderno_id=030&busca=Pesquisar&listaCadernos=&palavraChave=Heilborn
22. Cardoso LRD, Malbergi A, Figueredo TFB. O consumo de álcool como fator de risco para a transmissão das DSTs/HIV/AIDS. Rev Psiq Clín. 2008; 5:70-5.
23. Bastos FI, Bertoni N, Hacker MA. Consumo de álcool e drogas: principais achados de pesquisa de âmbito nacional, Brasil 2005. Rev Saúde Pública. 2008; 42:109-17.