RESEARCH ARTICLES
Evaluation of the prevalence of genital infections in pregnant women undergoing gynecological nursing consultation
Amanda Souza de OliveiraI; Thaís Marques LimaII; Fernanda Câmara CamposIII; Karine de Castro BezerraIV; Mônica Oliveira Batista OriáV; Ana Kelve de Castro DamascenoVI
INurse. Master in Nursing. Member of the Nursing Research project on Maternal Health promotion. Nursing Department. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: aso.enfa@gmail.com or mandinhadeoliveira@hotmail.com
IINurse. Nursing Doctorate. Member of the Nursing Research project on promoting women's health. Nursing Department. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: thais.ml@hotmail.com
IIINurse. Master in Nursing. Member of the Nursing Research project on Maternal Health promotion. Nursing Department. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: fernandac21@gmail.com
IVAcademic Nurse. Nursing Department. Member of the Center for studies and research in Sexual and reproductive Health promotion. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: karineufc@gmail.com
VNurse. Nursing Doctorate. Assistant Professor of the Nursing department. Coordinator of the Center for the study and research on Sexual and reproductive Health promotion. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: monica.oria@ufc.br or profmonicaoria@gmail.com
VINurse. Nursing Doctorate. Assistant Professor of the Nursing department. Member of the Nursing Research project on Maternal Health promotion. Federal University of Ceará. Fortaleza, Ceará, Brazil. E-mail: anakelve@hotmail.com
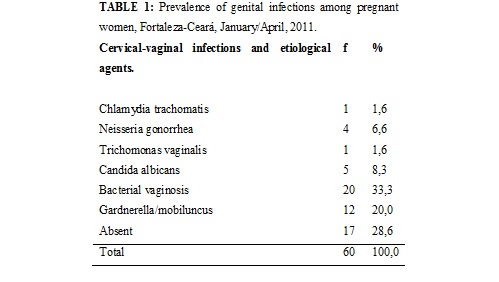
ABSTRACT: The aim of this study was to determine the prevalence and clinical profile of genital infections in pregnant women in Fortaleza-CE. It is a transversal study with 60 pregnant women at Center for Natural Childbirth Ligia Barros between January and April 2011. The data were collected through interviews and gynecological examination. For statistical analysis, we used the Pearson test (x²) and associations were considered significant when p<0,05. The cervicovaginal infections and etiological agents were the most prevalent bacterial vaginosis (33.3%) and Gardnerella (20.0%). There was no association between the variables of risk behavior with genital infection. Genital infections were associated with abnormal cervical mucus (p <0.05), test of the amines (p<0.05) and abnormal pH (p= 0.01). It is concluded that there was a high prevalence of pathogenic agents in patients, confirming the importance of prenatal care of pregnant women for diagnosis and appropriate treatment of these infections.
Keywords: Vaginal smears; Nursing; Pregnant; Sexually transmitted diseases.
INTRODUCTION
The Sexually Transmitted Infections (STI) deserve special attention from public health, because its prevalence is high in many countries. STIs are among the top five categories of diseases for which adults in developing countries seek medical help. Generally, they cause discomfort and loss of economic productivity1. Data from the National Program of Sexually Transmitted Diseases (STD) of the Ministry of Health about the prevalence of some STI indicated that, between 3,303 pregnant women, the prevalence of chlamydial infection was 9.4%, 1.5% of gonococcal infection and Human Papillomavirus (HPV) was 40.4%.
The more serious sequel and longer duration that affect women are: pelvic inflammatory disease, cervical cancer, infertility, miscarriage and ectopic pregnancy, these can lead to maternal death3.
One of the greatest challenges for the control of some of these diseases is low captivation and the consequent treatment of women diagnosed in the partners healthcare network. It is a problem that occurs with all STI and is related to various socio-cultural factors, such as prejudice, lack of sex education, the difficulty of prompting the partner to also seek medical aid, in addition to the difficulty of perception of the disease2.
The effective handling of STI prevents the development of complications and sequels, decreases the advancement of these infections in the community and offers a unique opportunity for an education focused on the prevention of Human Immunodeficiency Virus (HIV)4. The appropriate treatment of these infections in a first contact between patients and health professionals is, therefore, an important public health measure.
So, given the above, the study aimed to describe the rates of prevalence and clinical profile for genital infections in pregnant women who are attended in the Centre of Natural childbirth Lígia Barros of Fortaleza, Ceará.
LITERATURE REVIEW
Early identification of STIs in pregnant women is considered a challenge to public health, as these infections are relatively frequent and the risk of maternal-fetal transmission (vertical) is high, and can occur during pregnancy, in childbirth or during breastfeeding5.
Studies show that spontaneous abortions, stillbirths, low birth weight, congenital and perinatal infection, are associated to STI in pregnant women not treated3,6. In addition, the STI are predisposing factors for the acquisition of HIV, due to the presence of inflammation in cervix and can leave women more vulnerable during sexual intercourse with an infected partner7.
Because of this diversity of diseases and the difficulties already mentioned for abstraction and accession of the target audience to their treatments, the Ministry of Health, since the ´90, adopted the strategy of Syndromic approach of IST2, in order to do its early diagnosis and timely treatment, preventing sequels and reducing the risk of spread.
To this end, specific flowcharts have been developed for each category of pathologies (vaginal discharges, ulcers, urethral discharges and cervicitis). Studies show the easy applicability of flowcharts for major syndromes, with high cure rate, mainly for urethral discharge syndrome of genital ulcers2.
The identification of risk factors and symptoms of STIs associated with quick and effective treatment is critical during prenatal care, so that pregnant women have to improve their health and quality of life during this period.
Theoretically, the prenatal care quality, easily accessible, could recognize early signs or risk factors for morbidity and maternal mortality8, allowing, therefore, that appropriate interventions are applied.
METHODOLOGY
It was conducted a transversal study, descriptive and analytical delineation, held with 60 pregnant women in Natural Childbirth Center Lígia Barros of Fortaleza, Ceará, Brazil, from January to April 2011.
The study population was composed of pregnant women who performed nursing consultation in gynecology in the health unit. The study sample was defined by convenience, according to the following inclusion criteria: pregnant women in prenatal consultation on the selected Health Center forwarded for gynecological examination and/or have been forwarded by other health services to perform the gynecological examination on the study location.
The exclusion criterion was: pregnant women attended in other prenatal clinics or sexually-transmitted infections, that they have done treatment for some STI in this pregnancy. The criterion of discontinuity formed of withdrawal from participation in the research after the start of data collection and the women whose reports were not issued by the responsible laboratory for the period of the survey.
The form used for the collection of information was constituted by the registration of personal data (name, date of birth, place of birth, occupation, and marital status), clinical (symptom inventory and use of medications, surgeries and sexually transmitted infections), gynecological history (menarche, coitarche, date of last menstrual period, menstrual cycle pattern, parity, and number of partners), description of the clinical examination and the results of laboratory tests. The interview was followed by physical and pelvic examination, during which cervicovaginal samples were collected routinely.
The following tests were carried out: vaginal flow cytologic preparation for trichomoniasis; bacterioscopy by Gram of specimens of the vagina and cervix to cellular samples of bacterial vaginosis and gonorrhea, respectively; cytology ectocervix classified according to the Protocol of Bethesda9.
Bacterial vaginosis is diagnosed based on the presence of at least three of the four signs of the Amsel Criterion2: white vaginal viscous flow and homogeneous characteristic; vaginal fluid with pH > 4.5; release of fish odor coming from the vaginal fluid when mixed with 10% KOH; and clue cells composing at least 20% of vaginal epithelial cells, confirmed by Gram.
The data were organized and analyzed through the statistical program Statistical Package for the Social Sciences (SPSS) version 17.0. For comparative analysis, we used the Chi square test (x 2) of Pearson, settling less significance level than 0.05.
There were considered the ethical aspects of research involving human beings, in accordance with the established by Resolution No. 196/96, of the National Council of Health-Ministry of Health10, highlighting the signing of the Clarified Informed Consent of all participants of the study. This project was submitted for evaluation by the Committee of Ethics in Research at the Federal University of Ceará and approved as Protocol No 298/10.
RESULTS AND DISCUSION
As for the social demographic attributes, the participants were characterized with an average age of 24 years, prevalence of 50 (83.3%) pregnant women from Fortaleza, 47 (78.3%) lived with a partner, 26 (43.3%) had complete elementary school, 30 (50%) did not have a remunerated labor activity and 31 (56.4%) had household income of up to 1 minimum wage.
Genital infections were used as markers for the presence of association between risk behaviour and STIs. The prevalence rates of infections are listed in table 1.
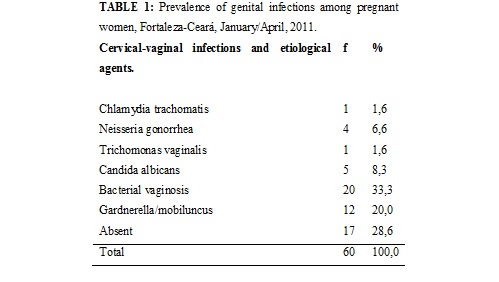
Although pregnant women are usually considered a portion of the population with low risk for STIs11, the study demonstrated a high prevalence of these infections in this public, reaching 71.7%.
The prevalence of 1.6% of chlamydial infection reported in this study, shows value of multicentric research dissenting, of nationwide ambit, in six Brazilian capitals, prevalence of 9.4%11. Other national researches show prevalence of chlamydia in pregnancy with variation between 2% and 9.4%12,13. Distant result of this study finds, and may be related to sample representation that was well below.
According to data from literature, the prevalence of chlamydia (C) can vary, depending on the population studied and the method used for the diagnosis14. The examination by the Polymerase Chain Reaction (PCR) seems to be more sensitive in infection detecting by C. trachomatis than other methods. In this way, the low prevalence among pregnant women researched in this study may be due, in part, to the test used for the detection of C. trachomatis, since the use of PCR techniques present sensibility that approaching 100%15.
As regards gonorrhea rate, value of 6.6%, this was higher than the found for Chlamydia, value of 1.6%, a result different from other Brazilian research which found prevalence of just 2%11.Comparison of prevalence measures between different regions of the world is difficult, due to the various diagnostic tests used and the population not comparable samples. Trace strategies, involving the introduction of more sophisticated and sensitive laboratory techniques, are always cause for intense debate by having greater immediate cost to the health system. We must note, however, that investment in early diagnosis and appropriate treatment of chlamydial infections and gonococo will represent the financial impact of expenditure reduction with harms to the health of the population11.
The prevalence of Trichomonas vaginalis infection amounted to 1.6%, and in recent decades, there has been a reduction in the number of cases of trichomoniasis, elucidated by use of treatment with metronidazole and improvement in the health conditions of the population1.
Still, in this study, the prevalence of infection by Candida albicans was 8.3%, lower than that found in research about the prevalence of vaginal flora changes in pregnant women, 11.8%16. It is known that 40% of pregnant women have species of Candida in vaginal flora, in larger quantity (twice) than that found in non-pregnant women. This happens due to increased levels of circulating estrogens and glycogen deposition and other substrates in the vagina during the gestational period17.
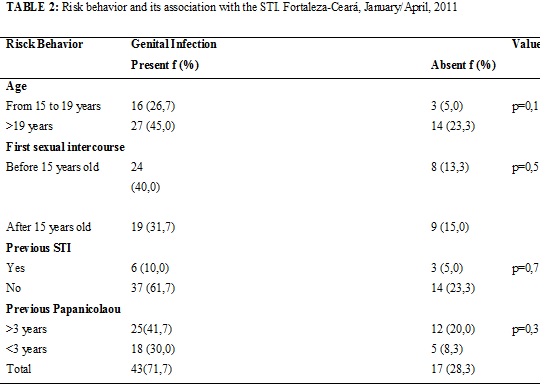
It can infer the absence of positive statistics associations with the variables related to risky behavior and presence of STI, as shown in Table 2. As regards the average age of first sexual intercourse, it was found the value of 16 (SD = ± 3.0), and 19 (31.7%) women had their first sexual intercourse after 15 years old. A similar result was found in the national study, whose average age of first sexual intercourse was 15.5 years old and 1,094 (33.1%) of pregnant women had their first sexual intercourse before 20 years old11.
In relation to prior history of STI, 51 (85%) women responded tha they have never purchased any type of STI. The presence of these infections, in addition to increasing the risk of contracting and transmitting HIV, can also cause sores and inflammation mucous membranes and skin of genitals that if they are not treated properly, can become precancerous lesions, leading to cervical cancer in the future18.
As for the time of the last cytological examination, 37 (61.7%) it was reported having prior examination in longer period of three years, worrying information, since the recommendation of screening in Brazil is three-year intervals, after two negative consecutive annual exams19. It is, therefore, essential that health services are structured to guide this population about the importance of preventive examination, since its implementation on a regular basis reduces the mortality from cervical cancer in the population at risk.
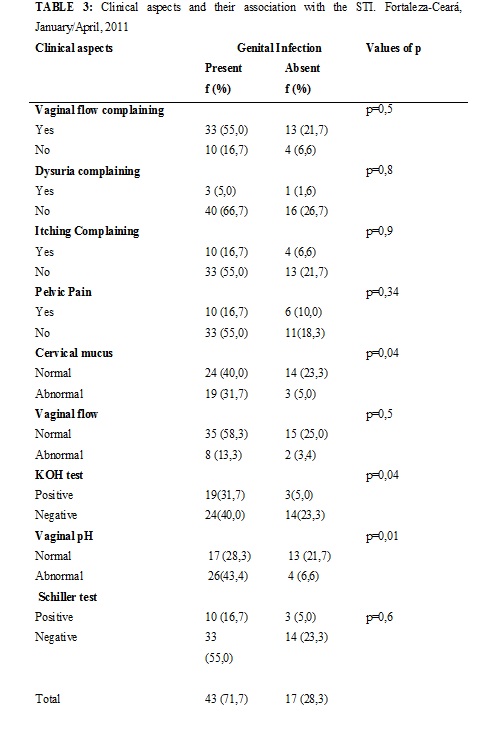
As for gynecological symptoms, vaginal flow was the most frequent symptom, being mentioned by 46 (76.7%) of users. The findings reveal that the genital infections were associated with abnormal cervical mucus (p = 0.04), test of amines (p = 0.04) and abnormal pH (p = 0.01), as represented in the Table 3. Research conducted in Botucatu, whose objective was to identify the prevalence of vaginal flora changes in low-risk pregnant women, showed the relationship between changes in the vaginal flora with bacterial vaginosis and vaginal candidiasis16.
The accuracy of clinical diagnosis of genital infections is low, while the laboratory diagnostic methods are complex and expensive, which can delay the onset of treatment. In cases where the tests that identify chlamydia and gonorrhea are not available, the use of the syndromic approach can be a tool used to diagnose symptomatic patients, since there is treatment for most organisms responsible for the syndrome20.
During the testing of Schiller, 13 have been identified (36.7%) women with a positive result. Study in Barbacena, where assessed the association between HPV infection and other genital infections, showed that the Schiller test and colposcopy changed were more common among patients with hybrid capture positive for HPV, although not statistically significant21.
It is believed that the reduction of the prevalence of HPV with the elevation of age would result from changes in sexual life, that would make women less exposed. However, many studies even report drop in prevalence of HPV infection with the advancement of age, even in women who maintain continuous and intense sexual activity22.
During the visual inspection with acetic acid (VAT), which is the direct visualization of the cervix after acetic acid application between 3 to 5%, were displayed in 18 white acetic lesions (30%) pregnant women. The VAT is the most studied trace method as an alternative to replacement or supplementation of colpocytology. However, consists of a subjective test, which can lead to a large number of false positive results, and still need to develop standards for the quality control of this21.
However, it is valid to note that even evaluating the diagnostic tests, it must highlight the gynecological complaining, as well as provide solutions and making them, whereas the reports of cytological examination, most of the time, microbiological agents which associated clinical complaining, deserve special treatment.
The accuracy of clinical diagnosis of genital infections is low, while the laboratory diagnostic methods are complex and expensive, which can delay the onset of treatment20. The establishment and use of protocols for the treatment of STIs can ensure that symptomatic and asymptomatic patients receive appropriate treatment and assistance in health services. Such protocols can also facilitate the training and supervision of health professionals and can minimize the risk of antimicrobial resistance2.
It is still necessary to strengthen measures for the prevention and treatment of the partner, of course, also contributes substantially to that these actions are actually effective. In this context, the screening of STIs during prenatal care has fundamental importance both in the early diagnosis and better therapeutic management.
CONCLUSION
Prevalence studies in pregnant women are particularly useful, since they provide estimates that can be extrapolated to the general population of sexually active women, since, by definition, the population of pregnant women does not include special risk situations and may be essential to facilitate the prevention of obstetric complications.
Considering the results, the high prevalence of STIs in pregnant women is perceived, however there was no significant statistical association between risky behavior and the presence of genital infection in this population.
Among gynecologic complaining reported, the presence of vaginal flow was the most frequent. So, it is the importance of the valuation of these complaining for the treatment of gynecological infections and prevention of these infections through health education, being the nurse cornerstone in this process.
It is during the gynecological prevention, the nurse should advise patients as to the early onset of sexual activity, multiple partners, presence of genital infections, in addition to the risk factors for HPV infection, emphasizing the importance of completion of the examination from time to time, even without symptoms and back to health unit to get the result.
It is evidenced that the vulnerability of pregnant women to the STI is something much more complex. It is based on knowledge of the customers studied that care to be provided should suit this population, respecting their social and cultural context.
The main difficulty encountered in the study was the non-attendance of women to service, needing further clarification of this population about the importance of the procedure. In this way, it is acknowledged that the study has some limitations, including the need to extend the sampling and, consequently, of the data and its possible variations. The indices of genital infections show that there is a problem to be controlled with actions directed to the evaluation of risk behavior, aimed at prevention of sexually transmitted infections.
REFERÊNCIAS
1. Barcelos MRB, Vargas PRM, Baroni C, Miranda AE. Infecções genitais em mulheres atendidas em Unidade Básica de Saúde: prevalência e fatores de risco. Rev Bras Ginecol Obstet. 2008; 30: 349-54.
2. Ministério da Saúde (Br). Programa Nacional de DST e Aids. Manual de Controle das Doenças Sexualmente Transmissíveis. Brasília (DF): Ministério da Saúde; 2006.
3. World Health Organization. Department of Reproductive Health and Research. Prevalence and incidence of selected sexually transmitted infections, Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis and Trichomonas vaginalis: methods and results used by WHO to generate 2005 estimates. Geneva: WHO; 2011.
4. Ministério da Saúde (Br). Programa Nacional de DST e Aids. Prevalências e frequências relativas de Doenças Sexualmente Transmissíveis (DST) em populações selecionadas de seis capitais brasileiras, 2005. Brasília (DF): Ministério da Saúde; 2008.
5. Figueiró-Filho EA, Senefonte FRA, Lopes AHA, Morais OO, Souza Júnior VG, Maia TL, et al. Frequência das infecções pelo HIV-1, rubéola, sífilis, toxoplasmose, citomegalovírus, herpes simples, hepatite B, hepatite C, doença de Chagas e HTLV I/II em gestantes, do Estado de Mato Grosso do Sul. Rev Soc Bras Med Trop. 2007; 40: 181-7.
6. Fonseca TMV, Cesar JA, Hackenhaar AA, Ulmi EF, Neumann NA. Corrimento vaginal referido entre gestantes em localidade urbana no Sul do Brasil: prevalência e fatores associados. Cad Saúde Pública. 2008; 24: 558-66.
7. Smeltzer SC, Bare BG. Brunner & Suddarth. Tratado de enfermagem médico-cirúrgica. Rio de Janeiro: Guanabara Koogan; 2005.
8. Peixoto CR, Freitas LV, Teles LMR, Campos FC, Paula PF, Damasceno AKC. O pré-natal na atenção primária: o ponto de partida para reorganização da assistência obstétrica. Rev enferm UERJ. 2011; 19: 286-91.
9. Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002; 287: 2114-9.
10. Ministério da Saúde (Br). Conselho Nacional de Saúde. Resolução 196/96.Diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Brasília (DF): Ministério da Saúde; 1996.
11. Jalil EM, Pinto VM, Benzaken AS, Ribeiro D, Oliveira EC, Garcia EG, et al. Prevalência da infecção por clamídia e gonococo em gestantes de seis cidades brasileiras. Rev Bras Ginecol Obstet. 2008; 30: 614-9.
12. Gavazzoni MF, Perissé ARS, Nery JAC. Sífilis e outras doenças sexualmente transmissíveis. In: Azulay-Abulafia L, Alves GF, Costa A. Dermatologia e Gravidez. Rio de Janeiro: Elsevier; 2009. p. 277-92.
13. Manela-Azulay M, Azulay DR. Doenças sexualmente transmissíveis. In: Azulay RD, Azulay DR, Azulay-Abulafia L. Dermatologia. Rio de Janeiro: Guanabara-Koogan; 2008. p. 367-88
14. Machado Filho AC, Sardinha JFJ, Ponte RL, Costa EP, Silva SS, Martinez-Espinosa FE. Prevalência de infecção por HIV, HTLV, VHB e de sífilis e clamídia em gestantes numa unidade de saúde terciária na Amazônia ocidental brasileira. Rev Bras Ginecol Obstet. 2010; 32: 176-83.
15. Meyer T. Modern diagnosis of Chlamydia trachomatis infections. Hautarzt. 2007; 58: 24-30.
16. Gondo DCAF, Duarte MTC, Silva MG, Parada CMGL. Alteração de flora vaginal em gestantes de baixo risco, atendidas em serviço público de saúde: prevalência e associação à sintomatologia e achados do exame ginecológico. Rev Latino-Am Enfermagem. 2010; 18: 919-27.
17. Bonfati G, Gonçalves TL. Prevalência de Gardnerella vaginalis, Candida spp. e Trichomonas vaginalis em exames citopatológicos de gestantes atendidas no Hospital Universitário de Santa Maria-Rio Grande do Sul. Revista Saúde (Santa Maria). 2010; 36: 37-46.
18. Casarin MR, Piccoli JCE. Educação em saúde para prevenção do câncer de colo do útero em mulheres do município de Santo Ângelo/ Rio Grande do Sul. Ciênc saúde coletiva. 2011; 16: 3925-32.
19. Ministério da Saúde (Br). Instituto Nacional do Câncer (INCA). Diretrizes brasileiras para o rastreamento de câncer de colo uterino. Rio de Janeiro: INCA; 2011.
20. Yin YP, Wu Z, Lin C, Guan J, Wen Y, Li L, et al. Syndromic and laboratory diagnosis of sexually transmitted infection: a comparative study in China. Int J STD AIDS. 2008; 19: 381-4.
21. Arian LO, Derchain SFM, Bastos JFB. Métodos diagnósticos para o rastreamento do câncer de colo. Rev Bras Ginecol Obstet. 2010; 32: 363-7.
22. Nogueres IB, Zimmermmann JB, Gonçalves LG, Fontes LC, Alves LF, Gontijo CC. Associação entre a infecção pelo Papilomavírus humano (HPV) e outras infecções genitais. Hospital Universitário Revista. 2010; 36: 19-28.