RESEARCH ARTICLES
Dyspareunia, perineal pain and healing after episiotomy
Nathália Luiza Souza e SilvaI; Sonia Maria Junqueira Vasconcellos de OliveiraII; Flora Maria Barbosa da SilvaIII; Jaqueline de Oliveira SantosIV
INurse, National Council for Scientific and Technological Development (CNPq) Scholarship. Kidney and Hypertension Hospital, Unit for Immediate Post-OperativeCare. Member of the Research Group: Nursing and Birth Care: models, agents and practices. São Paulo, Brazil. E-mail: nathalia_ls@yahoo.com.br.
IIAssociate Professor.School of Nursing, Maternal Child and Psychiatric Nursing Department, Universidade de São Paulo. Leader of the Research Group: Nursing and Birth Care: models, agents and practices.São Paulo, Brazil. E-mail: soniaju@usp.br.
IIISenior Lecturer - Midwifery Course, School of Arts, Sciences and Humanities. Public Health Graduate Program, Universidade de São Paulo. Member of the Research Group: Nursing and Birth Care: models, agents and practices.São Paulo, Brazil. E-mail: floramaria@usp.br.
IVNurse Midwife. Ph.D., Lecturer -Institute of Health Sciences at Universidade Paulista. Member of the Research Group: Nursing and Birth Care: models, agents and practices.São Paulo, Brazil. E-mail: jaquelineoliveira1@hotmail.com.
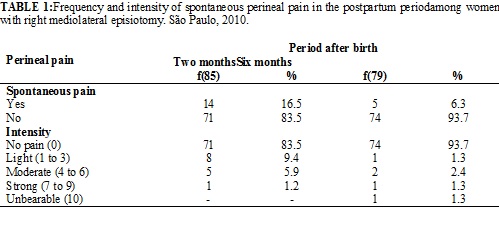
ABSTRACT: The objectives of this study were toidentifydyspareunia, perineal pain andabnormalities inperineal woundhealing in women who underwent episiotomy. Longitudinal studythatcontinuedtheclinical trialtoevaluatetheeffectivenessoflow-intensity laser in reducing perineal pain in these women.It was carried out at Amparo Maternal, cityof São Paulo,with85 and 79 women, who were interviewedattwomonths (from January to May, 2010) andsixmonthspostpartum (from June to September, 2010), respectively.Perineal painwasverifiedin 16.5% and 5.1% ofwomen,anddyspareunia in 69.7% and 29.2% ofthem,attwoandsixmonthspostpartum, respectively. At sixmonths, almosthalfof theparticipantsreported perineal painandsomeabnormality in thewoundhealing: changes in sensitivityand color oftheskin in the perinealregionanddehiscence. It was concludedthat perineal painanddyspareunia are common postpartummorbidities.
Keywords: Pain; perineum; dyspareunia; episiotomy.
INTRODUCTION
In the postpartum period, severalphysiological adjustments occur in the woman’s body, who may develop morbidities caused by spontaneous perineal trauma or due to the practice of episiotomy in vaginal birth. Perineal pain and dyspareunia are of great importance, as both may negatively affect the quality of life of the woman, causing considerable discomfort. Dyspareunia is a common, short-term complication, and rarely lastsfor more than one year after the birth1. This high prevalence of dyspareunia was verified in an English retrospective cohort study with primiparae, in which most of participants (68.2%; 379) referredpain in the first sexual relation after the birth, regardless of the presence of perineal trauma.However, the intensity of the pain during intercourse was significantly greater among those women with more severe (third and fourth degrees) spontaneous lacerations2.
These findings are corroborated by various studies that verifiedhigh rates of perineal pain following normal birth due to perineal trauma. A cross-sectional study was performed in a public teaching hospital in São Paulo, with 303 post-vaginal birth women, and verified that 80.5% present perineal trauma, 75.4% episiotomies and 24.6% lacerations.The prevalence of perineal pain was 18.5%, with moderate intensity (51.8%), associated to the episiotomy (p=0.001)3. On the other hand, in a study with 6,365 women, conducted in a maternity service wherenurse midwives provide the care to the woman in labor and normal birth, lower rates of perineal trauma were observed. Episiotomy rates were 25.9% among these women and perineal integrity was sustained by 28.6% of them4.
Additionally to pain reports, perineal trauma can impairthe sexual function of the woman. A study developed in a university hospital in Sweden compared the sexual health of women who underwent or not episiotomy.The results did not show significant differences in the level of sexual satisfaction between the groups, in spite of women who underwent episiotomy reported higher levels of vaginal discomfort. It was concluded that there is an association between the episiotomy and the occurrence of dyspareunia5.
These data were similar to a study carried out in Turkey, which compared different aspects of the sexuality of women who sustained an intact perineum with those who hadperineal trauma after normal birth. At least one of the investigated sexual problems (decrease of sexual desire, vaginal lubrication, frequency of orgasms and decrease ofvaginal excitement) was present after the birth. Comparing women with an intact perineum with those who had 2nd degree lacerations and episiotomy, the authors observed that the latter presented less sexual satisfaction and more pain during sex6. All of these findings report a relation between episiotomy and dyspareunia and point out the need to investigate the occurrence of this discomfort. Therefore, the objectives of this study were to identify the frequency of dyspareunia and the frequency and intensity of perineal pain in women who underwent right mediolateral episiotomy, at two and six months after normal birth, and to identify abnormalities in the perineal wound healing, as reported by the participants six months after birth.
BACKGROUND
The healing process of perineal traumas may influence postpartum dyspareunia.Perineal wounds usually have little tissue loss and the healing occurs by first intention, that is, union of the cut edges of the wound, such as in the episiotomy repair.Little granulation tissue is produced during the healing process, and the epithelialization is usually complete from ten to 14 days, although more time is necessary for the tissue to recover resistance to traction.Other factors, such as inadequate nutrition and smoking, also delaywound healing7.
In addition to these factors, the surgical technique and the type of suture material used in the repair may also interfere in the healing process and perineal pain. Continuous suturing technique8 and the use of the Vycril rapide9 rapidly absorbing synthetic materialare associated with less short term postpartum pain.
The woman and her partner have little professional information available on what they should expect or how to deal with the problem of dyspareunia.Therefore, the factors mentionedabove may result in morbidities and should be identified and considered by health professionals, as they might subsidize preventative and intervention strategies, in addition to information for women.
METHODOLOGY
This research is a longitudinal study with prospective data collection, a follow-up of the participants of a controlled, randomized clinical trial on the efficacy of low-intensity laser to reduce perineal pain after normal birth with right mediolateral episiotomy.The clinical trial was developed in the Birth Center (BC) of Amparo Maternal Hospital, a maternity service located in the south area of the São Paulo city, Brazil. The data collection occurred from November 2009 to March 2010.
One hundred and fourteen puerperaewere included in the clinical trial. The women were randomly assignedto three groups, in which they received the following doses of low-intensity laser on the episiotomy: Red Group (n=38) - wavelength 660 nanometers (nm); Infrared Group (n=38) - wavelength 780 nm, and Control Group (n=38) - simulation of application of low-intensity laser.Inclusion criteria were: age ≥ 18 years; full term pregnancy with a live fetus in cephalic presentation; no preparation of the perineal region during pregnancy and no evidence of perineal infection, hemorrhoids, hematomas, edema or varices in the vulvar region; no use of endogenous or exogenous photosensitive drugs and no clinical or obstetric complications.
Exclusion criteria were the use of any product on the vulvoperineal region during hospitalization, aside from soap and water. This clinical trial did not find differences amongthe three groups regarding perineal pain, after application of the laser10.
In this study, data was collected with an instrument (questionnaire) developed for this research, with the women who participated in the clinical trial. The main outcomes were: perineal pain, dyspareunia and perineal healing.
At first, participants were informed about the study and invited to take part in this new phase of the research through a telephone interview, two months after normal birth, when she was questioned about pain on the perineal region (on the suture location).
Next, she was questioned on the intensity of the present perineal pain, through a numeric scale from 0 to 10, with 0 meaning no pain, and 10 unbearable pain.The researcher inquired if the womanhad already resumedhaving sex by the date of the interview, and if yes, asked about the occurrence and intensity of pain during intercourse, using the same numeric scale of pain.These interviews were performed at two (January to May 2010) and six months after birth (June to September 2010).
In the second telephone call, the women were questioned about the characteristics or aspects of the perineal region.Most of the participants reported that they had already looked at the location with a mirror, and those that had not were requested to do so.
The women were requested to check their perineal region for the occurrence of dehiscence of the suture (if total or partial), presence of infection, fibrosis and spontaneous pain, abnormalities in skin coloration, and palpation for skin sensibility. The participants were questioned if they perceived that some or all of the suture stitches had opened; if they noticed a difference of color around the wound, and what was it like; if they felt that the region was more sensitive to touch; if the sutures hadany discharge; if they observed that the wound was thick with darker coloring, and whether the pain was constant or only sensitive to touch.
After the self-evaluation of the perineum, the women’s doubts regarding perineal pain and healing were clarified, and the telephone interview was finalized.
The intensity of perineal pain and dyspareunia was classified into the following categories: no pain (0), mild (1 to 3), moderate (4 to 6), strong (7 to 9) and unbearable. Statistical package SPSS for Windows software, version 10.0 was used for descriptive analysis of the data.
The project was approved by the Research Ethics Committee of the School of Nursing, University of São Paulo (Process number 778/2008).
RESULTS AND DISCUSSION
Of the total 114 women included in the randomized clinical trial, 87 (76.3%) were interviewed by phone. Most of them (85/114; 74.6%) agreed to participate in this study (second phase) two months after the birth. Six months after the normal birth (third phase) 79 of 114 (69.3%) participated in the study. There was a loss of 39 women at two months and six more (45) at six months. Analysis of the sociodemographic and obstetric characteristics of the 85 women in the second phase of the study showed that most of the participants, in all groups, were young, with an meanage of 22.5 ± 4.2 years, with minimum and maximum values of 19 and 36, respectively. Most of them (77/85; 90.58%) werenulliparae; had a partner (66/85; 77.6%); received emotional support during labor and delivery (81/85; 95.3%); did not smoke (78/85; 91.8%).As expected, there was an increase in the number of participants with no perineal pain as well as a reduction of the pain intensity, when the results for pain were compared between two and six months.However, one woman (1/79; 1.3%) still cited unbearable pain at six months, which was not verified in the previous phase. See Table 1.
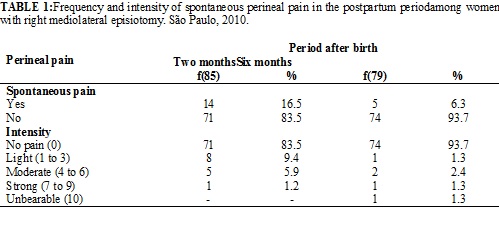
It is worth noting that among the puerperae with perineal pain at two months, the meanpain score was 3.2 with the standard deviation 2.2, with minimum and maximum values of 1 and 7, respectively.At six months, the values were: mean 6.0, standard deviation of 2.7; minimum 3 and maximum 10. Regarding the sexual activity of the participants, at two months 56 of 85 (65.9%) of the women had resumedsexual activity, and 72 of 79 (91.1%) at six months, (data not presented on the table).
Among women engaging in sexual activities, the occurrence of dyspareunia and its intensity was investigated. The data demonstrated that at two months, 39 of 85 (69.7%) participants mentioned discomfort, and at six months this value decreased to 21 of 79 (29.2%). A decreasein all scores of intensity of dyspareunia was observed, including the participants that cited unbearable pain, which fell from 3 out of 85 (5.3%) to 1 out of 72 (1.4%), as shown in Table 2.

The healing process of the episiotomy was investigated only at six months after the birth. The outcomes showed that 49.4% of the women reportedsome type of abnormality in the perineum healing and most of them cited some degree of fibrosis. More than one-third of the women reported increased sensibility and changesin the skin color. Approximately one-fifth (7/39; 17.9%) of the women cited partial dehiscence.Of these, three women reportedthat one suture point was still open, but did not search health care. The less cited abnormality was pain to palpation.
Perineal pain and dyspareunia in the postpartum period
Postnatal care is frequently neglected. There are few studies on this period (two to six months after the birth) in Brazil, with research being primarily restricted to the period of hospitalization or a few days after the birth.
Among the characteristics of the participantsof this this study, ayoung age is of note. This result was expected due to the research inclusion criteria, which excluded adolescence and included only women without previous vaginal birth and resulted in 93.3% nulliparous participants.Similar results were verified in the study carried outin the same institution, with the same criteria of the current research, and obtained participants with a mean age of 22.2 ± 3.8 years12.
Irrespective of the sociodemographic characteristics, the puerperamay have several morbidities, among which perineal pain is included and which may persist for months after the birth13. The results showed that about one-fifth of the participants mentioned perineal paintwo months after giving birth.Similar data were observed in a Brazilian research on which 18% of the participants reported spontaneous perineal pain at 41 days after normal birth14. Lower results were verified in the prospective cohort study, performedin Canada at six weeks after birth, which verified a rate of perineal pain of 7% in any type of perineal trauma15. These findings are opposite to those of the national survey-type study conducted in the United States, in which the contact was done through email or telephone, showing approximately double the pain of the women according to the type of birth, after two months.At six months, there was no relation between episiotomy and persistence of perineal pain13. In this study, as expected, there was a reduction in the frequency of perineal pain, but half of the women who cited pain at two months had still reported this morbidity six months after the birth.
The intensity of the pain is directly related to the type and degree of perineal trauma.Prospective study that evaluated perineal pain reported higher means scoresof pain among women who had 2nd, 3rd and 4th degree lacerations, in comparison with those who had sustained perineal integrity16. Perineal trauma can also negatively influence sexual activity, as reported by a study carried out with 2,490 Swedish women, which verified the association between not having resuming sex at 3 and 6 months after the birth, and type of perineal trauma. Women who had 3rd and 4th degree tears had higher risk of not having intercourse17.
In order to evaluate dyspareunia, it is needed to verify if the participants in a specific research had resumed sexual activity when obtaining the data. In the English study cited above, 40% of those researched had resumed sex seven weeks after the birth16. The resumption of sexual activity was similar to that found in our study, in which 65.9% of the women mentioned resuming sexual relations two months after the birth, and 91.1% after six months. However, in a Scottish studywomen resumed sexual activity a little later, with 90% of them having intercourse at around ten weeks after the birth18.
Regarding the occurrence of dyspareunia, our findings indicate that most of women reportedthis discomfort at two months after the birth, which decreasedfor about one-fifth of women at six months. Similar findings were reported in the study cited above, which showed dyspareunia at two months postpartum, in 54.8% of primipara who had undergone episiotomy. At six months, there is no information about this discomfort13. Notwithstanding, an Italian study found the prevalence of 16.2% of dyspareunia among women interviewed about one year after the birth. Among the women who reported this morbidity, 66.2% of them had undergone episiotomy1.
Considering the healing of perineal trauma, perineal lacerations and episiotomies can be classified as acute wounds that generally heal quickly, with no complications. However, its healing may be affectedby factors such as higher maternal age, poordiet, obesity, stress and anxiety, infection, smoking and some drugs19.
Studies report different types of sutures and analyze their effects. In one study previously mentioned, the researchers concluded that the separate and continuous suture techniques are safe and secure, but the women who had continuous sutures presented less pain to palpation four days after the birth, and in activities such as sitting, walking, urinating and defecating14.
Qualitative research that evaluated the influence of the episiotomy on feminine sexuality reported that the episiotomy scar interfered in the sexual activity, as some participants cited a feeling of embarrassment with their partners due to reasons as aesthetic changes of the perineum20. It is noted that this abnormality is not uncommon, since in this study, more than half of the women reported the presence of fibrosis on the episiotomy healing.In a study carried out 41 days after the birth, the results showed that 41.0% of the women hadscar fibrosis14.
CONCLUSION
Problems with perineal pain and dyspareunia are common postpartum morbidities. Assessing the healing of the episiotomy is important, as in this period almost half of the participants cited some healing abnormality.In this study, even six months after normal birth, the women reported perineal pain, changes in the sensibility and coloration of the skin on the perineum region and partial dehiscence.
REFERENCES
1. Bertozzi S, Londero AP, Fruscalzo A, Driul L, Marchesoni D. Prevalence and risk factors for dyspareunia and unsatisfying sexual relationships in a cohort of primiparous and secondiparous women after 12 months postpartum. InternJ Sexual Health. 2010;22(1):47-53.
2. Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184:881-8.
3. Francisco AA, Oliveira SMJV, Santos JO, Silva FMB. Avaliação e tratamento da dor perineal no pós-parto vaginal. Acta PaulEnferm. 2011;24:94-100.
4. Riesco MLG, Costa ASC, Almeida SFS, Basile ALO, Oliveira SMJV. Episiotomia, laceração e integridade perineal em partos normais: análise de fatores associados. Rev enferm UERJ. 2011;19:77-83.
5. Ejegard H, Ryding EL, Sjogren B. Sexuality after delivery with episiotomy: a long-term follow-up. GynecolObstetInvest. 2008;66(1):1-7.
6. Rathfisch G, Dikencik BK, Beji NK, Comert N, Tekirdag AI, Kadioglu A. Effects of perineal trauma on postpartum sexual function. JAdvNurs. 2010;66:2640-9.
7. Grundy L. The role of the midwife in perineal wound care following childbirth. Br J Nurs. 1997;6:584-8.
8. Kettle C, Hills RK, Ismail KMK. Continuous versus interrupted sutures for repair of episiotomy or second degree lacerations. Cochrane Database of Systematic Reviews. In: The Cochrane Library, Issue 12, 2007. No. CD000947.
9. Kettle C, Dowswell T, Ismail KMK. Absorbable suture materials for primary repair of episiotomy and second degree tears. Cochrane Database of Systematic Reviews. In: The Cochrane Library, Issue 12, 2010. No. CD000006.
10. Santos JO. Ensaio clínico randomizado sobre a efetividade do laser em baixa intensidade no alívio da dor perineal no parto normal com episiotomia [tese de doutorado]. São Paulo: Universidade de São Paulo; 2010.
11. Pimenta CAM, Cruz DALM, Santos JLF. Instrumentos para avaliação da dor: o que há de novo em nosso meio? ArqBrasNeurocir. 1998;17:15-24.
12. Leventhal LC, de Oliveira SM, Nobre MR, da Silva FM. Perineal analgesia with an ice pack after spontaneous vaginal birth: a randomized controlled trial. J Midwifery Womens Health. 2011;56(2):141-6.
13. Declercq E, Cunningham DK, Johnson C, Sakala C. Mothers' reports of postpartum pain associated with vaginal and cesarean deliveries: results of a national survey. Birth. 2008;35(1):16-24.
14. Almeida SFS, Riesco MLG. Randomized controlled clinical trial on two perineal trauma suture techniques in normal delivery. RevLatino-Am Enfermagem. 2008;16:272-9.
15.Macarthur AJ, Macarthur C. Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. AmJObstet Gynecol. 2004;191:1199-204.
16.Andrews V, Thakar R, Sultan AH, Jones PW. Evaluation of postpartum perineal pain and dyspareunia-a prospective study. Eur J Obstet Gynecol Reprod Biol. 2008;137(2):152-6.
17.Radestad I, Olsson A, Nissen E, Rubertsson C. Tears in the vagina, perineum, sphincter ani, and rectum and first sexual intercourse after childbirth: a nationwide follow-up. Birth. 2008;35(2):98-106.
18.Glazener CM. Sexual function after childbirth: women's experiences, persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol. 1997;104(3):330-5.
19.Steen M. Perineal tears and episiotomy: how do wounds heal? BrJMidwifery. 2007;15(5):273-80.
20.Progianti JM, Araújo LM, Mouta RJO. Repercussões da episiotomia sobre a sexualidade. Esc Anna Nery. 2008;12:45-9.