RESEARCH ARTICLES
Self-medication in the elderly: a public health problem
Paulo Celso Prado Telles FilhoI; Áglidy Gomes Pena AlmeidaII; Marcos Luciano Pimenta PinheiroIII
IMaster’s and doctoral degrees from the University of São Paulo at Ribeirão Preto College of Nursing. Adjunct professor in the Department of Nursing at the Universidade Federal dos Vales do Jequitinhonha e Mucuri. Diamantina, Minas Gerais, Brazil. E-mail: ppradotelles@outlook.com.
IINursing undergraduate at the Universidade Federal dos Vales do Jequitinhonha e Mucuri. Diamantina, Minas Gerais, Brazil. E-mail: aglidygomes@yahoo.com.br.
IIIMaster’s and doctoral degrees in Pharmacology, Anesthesiology and Therapy from the Piracicaba College of Dentistry at the University of Campinas. Adjunct Professor in the Department of Basic Sciences at the Universidade Federal dos Vales do Jequitinhonha e Mucuri. Diamantina, Minas Gerais, Brazil. E-mail: marcospimenta2@gmail.com.
ABSTRACT: Self-medication can cause adverse effects, allergic reactions and intoxication. The objective of this study was to describe self-medication in regard to frequency, reasons, justifications, ingestion times and influences in elderly individuals followed at a Family Health Strategy unit, in a municipality in the interior of the state of Minas Gerais. This descriptive study was carried out with 50 elderly individuals, based on a validated questionnaire applied from January to March of 2011. In regard to reasons, pain was reported by 41 (82%) of the participants, followed by the, which was reported by 8 (16%). In regard to justification, 29 (58%) reported having the medicine at home, and five (10%) reported difficulties to schedule a medical appointment. In regard to influences, 31(62%) reported advertising/media. It is nursing’s responsibility to provide real solutions in the context of educating and informing the population about self-medication.
Keywords: Nursing; aged, drug utilization; self medication.
INTRODUCTION
Self-medication is defined as the use of drugs without a medical prescription, in which the patient he/herself decides which medicine to use, advised almost entirely by untrained persons such as friends, family members or pharmacy clerks1.
Such practice signals a public health problem, indicating various negative aspects such as adverse effects, allergic reactions, intoxications and drug interactions. Additionally, self-medication can delay the diagnosis of a pathology2. Therefore, in order to avoid problems, specific knowledge and skills on pharmacology, interaction and drug reactions are necessary3.
In the elderly, self-medication can be even more serious, implying various health risks. Aging brings with it simultaneous ailments of organs and tissues, causing a greater prevalence of degenerative and non-communicable chronic illnesses, in addition to functional changes that cause modifications to the pharmacokinetics of drugs, for example, compromising renal function, essential for purification of drugs from the body, primarily through the kidneys, as well as compromised blood flow, which is responsible for transporting the drug to its receptor, as well as hepatic biotransformation, the process responsible for metabolizing the drugs4.
It is important to highlight that in 2001, 80 million people practiced self-medication, and every year about 20,000 people die as a result5. Of this number, the percentage of elderly is not known; however, from 1991 to 2007, average life expectancy in Brazil increased from 67 to 72.57 years, and it is estimated that by 2015 it will have the world’s sixth largest elderly population, thus demanding special care6.
Based on the above, it is clear that with regard to medication, the overall health situation -of elderly Brazilians should be the target of improvements, through the rigorous fulfillment of health legislation and implementation of efficient measures for pharmaceutical care in both the public and private health systems, for the promotion of health and quality of life of the elderly population.
It is, therefore, vital to identify and analyze self-medication in the elderly, so that such information can serve as the basis for health care actions, thus permitting to plan a rational use of drugs, providing information to maximize individual and collective health conditions, as well for the implementation of preventative and/or curative projects.
The objective of this study was to describe self-medication in regard to frequency, reasons, justifications, ingestion times, and influences in elderly individuals followed by a Family Health Strategy (FHS) unit in a municipality in the interior of the state of Minas Gerais.
LITERATURE REVIEW
With the alteration of the demographic profile during the last decades of the 20th century, related to increased longevity and reduced mortality rates, Brazil ceased to be a country with a young population. This change to the demographic profile, and consequently to the illness profile, makes it necessary to create public policies especially designed for the promotion of elderly health. However, iatrogenesis has been pointed out by specialists on elderly health as a public health problem. The pharmacological interactions between some drugs are extremely harmful to the balance of the human organism, especially in advanced age7.
Further, the use of medicines increases linearly with increased age, and in Brazilian society, elderly people are more exposed to polypharmacotherapy, on average taking two to five medicines per day. This fact can partly be or be partly? justified by the chronic diseases that emerge with aging which require the use of such medicines. It is worth emphasizing that despite not being the only phenomenon of modernity, the consumption of medications without a prescription has become common practice in the Brazilian population8.
It is imperious to add that medicines play a central role in the search for health recuperation, and is a key element of professional practice. The availability of these products can satisfy the expectations of users, but should be considered by health professionals as an additional tool, an accessory to preventative and public health measures, especially those affecting the elderly, which have a growing need for maximization of their quality of life9.
Nevertheless, self-medication moved approximately R$ eight billion in 2008, corresponding to 30% of the entire market for pharmaceuticals in Brazil. Medications are a symbol of health, and the belief that it is possible to achieve complete cure for most pathologies by taking capsules or pills is mistaken, but has persisted for years. It is known, however, that the indiscriminate use of drugs can aggravate the patient’s state of health, causing intoxication or even death10.
METHODOLOGY
This is a descriptive study that has the objective to systematically describe factors and characteristics present in a determined population or area of interest, seeking to determine the frequency with which something occurs, or the relationship between two variables11.
The study was carried out in an FHS located in a municipality in the interior of the state of Minas Gerais, which serves an area with approximately 900 registered families, or about 3525 people, of which 317 are elderly. It operates from 7am to 5pm, with a health care staff composed of a nurse, nursing technician, physician and six community health agents.
The sample was randomized and the study counted with 50 individuals, all of whom were registered in the FHS, of both genders and aged 60 years or older, with preserved cognitive capacity, who agreed to participate in this research. Data collection was performed from January to March 2011, in the elderly participants’ homes, after they read and signed the Free and Informed Consent Form, using an adapted questionnaire12, which was applied by the researcher, including the reading and annotation of responses. The privacy of the subjects that responded to the questionnaire was guaranteed, as it was filled out at a location without the presence of other individuals.
The questionnaire contained the following variables: age range, gender, marital status, level of education, frequency, reasons, justifications, ingestion times, and influences on the practice of self-medication.
The data were tabulated in the software program SPSS 18, and analysis was done using descriptive statistics.
The research was approved by the Coordination of the FHS under study, as well as by the Ethics Committee of the Universidade Estadual de Montes Claros, under protocol number 2029/2011. All ethical principles for human research were complied with, according to resolution 196/96 of the Ministry of Health13.
RESULTS AND DISCUSSION
Of the total 50 elderly individuals interviewed, 14 (28%) were ages between 60 and 65; 17 (34%) from 66 to 70 years; 7 (14%) from 71 to 75 years; 5 (10%) from 76 to 80 years; 6 (12%) from 81 to 85 years, and 1(2%) from 86 to 90 years.
In regard to gender, there were 13 (26%) men and 37 (74%) women. The socio-demographic characteristics of the elderly respondents resembled that observed in Brazilian population studies, with the predominance of women due to male excess mortality and subsequent feminization of the aging population14.
In regard to marital status, 22 (44%) were married, 20 (40%) were widowed, 4 (8%) were single, and 4 (8%) were divorced. Regarding level of education, 37 (74%) completed the 4th year of primary education and 13 (26%) were illiterate.
When questioned about the frequency with which they resorted to self-medication in the previous year, 44 (88%) confirmed that they had done so more than ten times per month, and six (12%) less than two times. This is worrisome, as the elderly present physiological changes that make them more prone to developing adverse reactions to drugs, and also because statistics show that adverse reactions to drugs are responsible for 10 to 20% of acute hospital admissions among the elderly15.
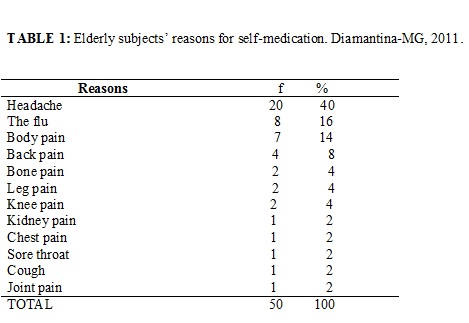
Table 1 lists the reasons for self-medication, as reported by the respondents.
Of the 12 reported reasons for self-medication, ten refer to pain, as shown in Table 1. This fact is extremely worrying, because it is known that self-medication can mask a disease or make it more serious. For example, an individual with hypertension who self-medicates because of a headache may suffer a stroke. Another who takes antibiotics on his or her own accord because of a sore throat, and always uses this medication for the same symptom, in addition to increasing bacterial resistance may be masking throat cancer.
In light of these facts, the nursing team is responsible for providing guidance on the drug, aiming for reduced risk and the greatest possible efficacy, promoting health education focused on the needs of the elderly, considering practices that may be damaging to health, promoting reflection and discussion on the theme for the entire population, as well as involving other professionals, managers and politicians16.
It is important to critically educate health professionals so that they become multipliers of information regarding the rational use of drugs17.
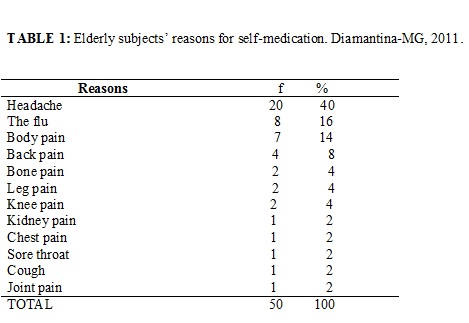
Table 2 lists the justifications for self-medication.
It is highlighted that 29 (58%) participants have the medicine at home, which contributes to self-medication not only of the individual but the entire family, because at the time at which the symptoms appear, having the drug within reach, without the need for a prescription, is the first step toward its indiscriminate use.
Despite being the justification with the lowest percentage, it should be noted that participants confirmed that they self-medicated because they did not deem a medical appointment necessary. This may be related to the predominant level of education in the study, that being the 4th year of primary education, which does not provide knowledge on physiopathological and pharmacological processes. Clearly, without specific knowledge, individuals are not fit for such a practice.
Further, it is possible to perceive that the justifications are not excluding. Actually, they complement one another, because the family member recommends a drug, there is no restriction to its purchase, when ingesting it s/he perceives that the symptoms are momentarily relieved, scheduling an appointment is difficult and the individual does not deem it to be necessary, culminating in self-medication, as shown in Table 2.
This fact is very worrying, as the health service, in addition to taking the time to search for strategies to minimize difficult access, must also act on every justification listed, because these constitute a vicious cycle that, independent of the starting point, tends to end in self-medication.
Therefore, focal intervention is not enough, as if, for example, the difficulty of scheduling an appointment was not recorded as a justification, the others would maintain the cycle.
The entire nursing team must assume an attentive stance, observing the situation which brought the individual to the unit, and, in some way, not allow him or her to return home without effective medical care, and show clear interest in a solution to the problem. This strategy is known as patient embracement, and allows patients to understand that the entire team participates in his/her recovery, without emphatically prioritizing medical and pharmacological care.
Additionally, it is necessary to develop work on health education, focusing on negative points related to self-medication, which has not only the elderly as the target audience, but the community in general, with the aim to reach family members responsible for recommending the use of medicines without prescription. With these attitudes adopted by the team, the middle- and long-term effect would be an effective reduction in the practice of self-medication.
Therefore, the need for including the family in the different moments of the educational process of the patient through active participation is emphasized, aiming for increased commitment towards patients18.
In terms of ingestion time, 46 (92%) confirmed using the drug from one to two days, and four (8%) confirmed using it for five days or longer. It is worth highlighting that all respondents reported that with the recurrence of symptoms, they returned to practice self-medication.
The fact that individuals reuse the drug when symptoms recur demonstrates that this study is in accordance with another in the literature, in which the drug plays a central role as a solution to health problems, transforming it into a type of hope for a cure that clouds the thoughts of the individuals19.
Unfortunately, this attitude of the population places health as merchandise and people lose autonomy in the healing process. This should instigate teams to incorporate other forms of care, in which the elderly take on a leading role in their own care, encouraging sensible self-care in families as indispensable for a good quality of life and health aging.
In Brazil, data on the irrational use of drugs shows that one-third of hospitalizations and 27% of intoxications are the result of incorrect use of drugs, and of these, 16% end in death20.
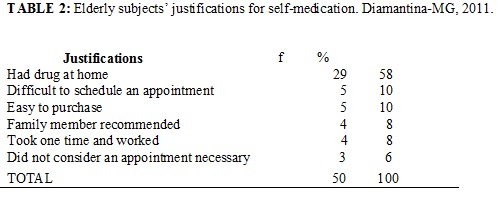
The influences to practice of self-medication by the research subjects are specified in Table 3.
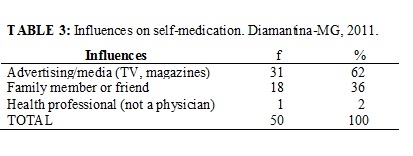
The media plays an important role in influencing self-medication, as 31 (62%) of the elderly subjects confirmed that they self-medicated encouraged bydrugs advertisements, as shown in Table 3.
It is sad that drug manufacturers use the means of communication to stimulate consumption, presenting the drugs as merchandise that needs to be constantly updated and renewed.
The dispute between manufacturers guaranteeing the efficiency and safety of their products, combined with the power of mass circulation of the media through announcements such as: immediate pain relief, improvement of physical performance, increased appetite and calms you down are strong incentives to self-medication.
The Brazilian Health Surveillance Agency (ANVISA) has a project called Monitoring of Advertising, which points to irregularities in about 90% of drug commercials. The situation is more alarming in the publicity directed to physicians and pharmacists. Of 1.5 thousand advertisements for prescription drugs analyzed by ANVISA, 15% did not present cautions or warnings; 14% did not warn about side effects; and approximately 10% contain claims without proof of scientific studies21.
Due to their close relationship with the elderly individual, family and community, it is understood that nursing professionals could develop a sharper eye for self-medication, as it is a common practice with serious risks to health, and which requires extreme caution in interventions. The ideal would be to orient everyone, as it is known that the elderly’s close ones have the strongest influence on them.
The concern with care for the elderly and their quality of life is not only restricted to the family, but evokes discussion about the formation of a support network for elderly care in a multidimensional context, focusing not only on physical aspects, and also considering psychological conditions, social relationships and the environment22.
The high frequency of influences from advertising and the media is confirmed, and keeping in mind that self-medication is a cultural phenomenon that is encouraged by commercials worldwide, it is noted that this is a delicate theme that has deserved the attention of health professionals for years.
Drug advertising is a theme that generates a lot of discussion, because different studies affirm it causes self-medication, which is increasingly common in the Brazilian population23.
Therefore, it is worth emphasizing that serious issues must be minimized for the sake of the elderly’s safety, and that this study presented the limitation of being developed in only one FHS, and, therefore, further studies should be developed on such an important topic.
CONCLUSION
This study described self-medication with regard to frequency, reasons, justifications, ingestion times, and influences in elderly patients of an FHS.
It shows the nursing team must create real solutions in terms of educating and informing the population, because as demonstrated in this study, self-medication is intimately related to lack of information.
REFERENCES
1. Vitor RS, Lopes CP, Menezes HS, Kerkhoff CE. Padrão de consumos de medicamentos sem prescrição médica na cidade de Porto Alegre, RS. Ciênc saúde coletiva. 2008;13:737-43.
2. Loyola FAI, Uchoa E, Lima CMF. Estudo epidemiológico de base populacional sobre uso de medicamentos entre idosos na região metropolitana de Belo Horizonte, MG. Cad Saúde Pública. 2006; 22:2657-67.
3. Silva LD, Santos MM. Interações medicamentosas em unidade de terapia intensiva: uma revisão que fundamenta o cuidado do enfermeiro. Rev enferm UERJ. 2011;19:134-9.
4. Flores VB, Benvegnú AL. Perfil de utilização de medicamentos em idosos da zona urbana de Santa Rosa, RS. Cad Saúde Pública. 2008;24:1439-46.
5. Instituto Virtual de Fármacos [site de Internet]. Automedicação: hábito perigos para a saúde. [citado em 20 dez 2012]. Available at:// www.ivfrj.ccsdecania.ufrj.br/ivfonline/edicao 0012/automedicacao.html.
6. Barros SM, Cabral BJA, Oliveira SPPB. Automedicação em idosos na cidade de Salgueiro, PE. Rev Bras Epidemiol. 2007;10:75-8.
7. Gallagher P, Barry P, O Mahony. Inappropriate prescribing in the elderly. J Clin Prarm Ther. 2007;3:113-21.
8. Bortolon PC, Medeiros EFF, Naves JOS, Karnikowski MO, Nobrega OTA. Análise do perfil de automedicação em mulheres idosas brasileiras. Cienc saúde coletiva. 2008;13:1219-26.
9. Araújo JJC, Vicentini GE. Automedicação em adultos na cidade de Guairaça, PR. Arq Ciênc Saúde Unipar. 2007;11:83-8.
10. Lima GB, Nunes LCC, Barros JAC. Uso de medicamentos armazenados em domicílio em uma população atendida pelo programa saúde da família. Ciên saúde coletiva. 2010;15:3517-22.
11. Gressler LA. Introdução a pesquisa, projetos e relatórios. São Paulo: Editora Loyola; 2004.
12. Vosgerau MZS, Soares DA, Souza RKT. Automedicação entre adultos na área de abragência de uma unidade de saúde da família. Lat Am J Pharm. 2008;27:831-8.
13. Ministério da Saúde (Br). Resolução 196 de 10 de outubro de 1996: normas de pesquisa envolvendo seres humanos. Brasília (DF): Ministério da Saúde; 1996.
14. Naves JOS, Castro LLC, Carvalho CMS, Merchán-Hamann E. Automedicação: uma abordagem qualitativa de suas motivações. Ciênc saúde coletiva. 2010;15:1751-62.
15. Silva CSO, Pereira MI, Yoshitome AY, Rodrigues Neto JF, Barbosa DA. Avaliação do uso de medicamentos pela população idosa em Montes Claros, Minas Gerais, Brasil. Esc Anna Nery. 2010;14:811-8.
16. Aquino D. Por que o uso racional de medicamentos deve ser uma prioridade? Ciênc saúde coletiva. 2008;13:733-6.
17. Telles Filho PCP, Pereira Júnior AC. Automedicação em crianças de zero a cinco anos: fármacos administrados, conhecimentos, motivos e justificativas. Esc Anna Nery. 2013;17:291-7.
18. Castro RA, Aliti GB, Linhares JC, Rabelo ER. Adesão ao tratamento de pacientes com insuficiência cardíaca em um hospital universitário. Rev Gaúcha Enferm. 2010;31:225-31.
19. Budó MLD, Resta DG, Denardin JM, Ressel LB, Borges ZN. Práticas de cuidado em relação à dor. Esc Anna Nery. 2008;12:90-6.
20. Marin MJS, Cecílio LCO, Perez AEWUF, Santella F, Silva CBA, Gonçalves Filho JR, et al. Caracterização do uso de medicamentos entre idosos de uma unidade do Programa Saúde da Família. Cad saúde pública. 2008;24:1545-55.
21. Agência Nacional de Vigilância Sanitária. [site de Internet]. Encontro discute propaganda e uso racional de medicamentos. [citado em 20 dez 2012] Available at: http://www.anvisa.gov.br/divulga/noticias/2005/091205_1.htm.
22. Meirelles BHS, Arruda C, Simon E, Vieira FMA, Cortezi MDV, Natividade MSL. Condições associadas à qualidade de vida dos idosos com doença crônica. Cogitare Enferm. 2010;15:433-40.
23. Silva RB, Corte TWF. A propaganda de medicamentos e sua adequação conforme a RDC 96/2008. Rev Grad PUCRS. 2009;3:1-11.