RESEARCH ARTICLES
Professional profile of university level workers in mental health services
Nathália dos Santos SilvaI; Elizabeth EsperidiãoII; Kelly Kan Carvalho da SilvaIII; Adrielle Cristina Silva SouzaIV; Ana Caroline Gonçalves CavalcanteV
INurse, Master's in Nursing, Federal University of Goias, School of Nursing, Goiânia, Goiás, Brazil, Email: silvans09@gmail.com,
IINurse, PhD in Psychiatric Nursing, Federal University of Goias, School of Nursing, Goiânia, Goiás, Brazil, Email: betesper@fen.ufg.br,
IIINurse, Federal University of Goias, School of Nursing, Goiânia, Goiás, Brazil, Email: anagcavalcante@gmail.com,
IVNurse, Federal University of Goias, School of Nursing, Goiânia, Goiás, Brazil, Email: drica_140@hotmail.com,
VNurse, Federal University of Goias, School of Nursing, Goiânia, Goiás, Brazil, Email: kkellynhaa@yahoo.com.br,
VIWe thank the Mental Health management of the Secretary of Health, State of Goiás for logistical support in the development of this research. We are grateful for the financial support of the National Council of Scientific and Technological Development (CNPq) and the Research Support Foundation of the State of Goiás.
ABSTRACT: The change in the model assitencial in mental health care in Brazil changed the logic of organization of work of workers. At a time of transition in specialized assistance that can represent a challenge for workers, with the need to change the profile and actions that will develop the specialized health services. The objective of this study was to characterize the socioeconomic profile and formation of workers in mental healthcare services in the state of Goias-Brazil. This is a descriptive study with the participation of 100 professionals working in 22 services. The results revealed characteristic in multidisciplinary training of workers, mostly young with little experience in mental health. The salaries are low and few professionals possess expertise in the area. There is a lack of investment in professional qualification and improvement of working conditions.
Keywords: Mental health; Human resources; Mental health services; Health Personnel.
INTRODUCTION
With the changes in the mental health care modelVI caused by the Brazilian Psychiatric Reform, it is essential to invest in continuing education of employees and managers who are working in this area to be able to rethink and instituting practices of care inherent in the National Mental Health Policy (PNSM), with a view to improving the living conditions and social reintegration of the users of the services of this area. The construction of the logic of mental health care is not restricted to new technology or scientific advance, but the new conception of science, places, social spaces and production of subjectivities1. Therefore the construction of the psychosocial care network goes far beyond the creation of non-hospital services2.
Thus, the change in the mental health care model represents a challenge to the workers, in the sense that they must adopt new knowledge, technologies and therapeutic methodologies, passing by the relations between the other components of the work team3,4.
In accordance with the approach of treating the patient with mental disorders, as the PNSM, there is a need for changes in the profile and in the actions that the professionals will establish in substitutive services5.
The World Health Organization (WHO) shows that human resources for mental health are insufficient in most low and middle-income countries6. Improving care must then consider adopting a decentralized care approach with the inclusion of workers from different areas: ensuring enough mental health specialists and adequate infrastructure, promote training and continuing education of professionals; adopt a social inclusion model and ensuring an intersectoral approach7.
Thus, the changes are necessary to consolidate, in fact, the Psychiatric Reform, favoring the implementation of psychosocial treatment for the patient and their family5.
There are still few studies that address this issue and that serve not only as criticism of reality, but also as exhibitors of the current context of care, with references to changes and or adaptations in the PNSM care. Whereas the state of Goiás, as well as throughout the country, is in a time of transition the hospital-centered model for the psychosocial model, this study was planned with the objective of this study was to characterize the professional graphic profile of top-level workers who work in public mental health services in the state of Goiás.
THEORETIC REFERENTIAL
The beginning of the Psychiatric Reform process in Brazil and prior to the beginning of the health movement in the 70s, which advocated a change of care models and management in the healthcare practice, fairness in the provision of services and involvement of workers and users of healthcare services in the processes of management and production technologies of care2,8,9.
Although contemporary Health Reform, the process of Psychiatric Reform in Brazil has a history of its own; this movement was influenced by reform movements that raged in Europe and in the United States, where various sectors of civil society have been mobilized in favor of the fight for the rights of patients and against segregation, violence and the abuse of this clientele8,9.
In 1978 came the Workers Movement in Mental Health (MTSM) who initiated the criticism this psychiatric model that prevailed in the exclusionary practices of psychiatric institutions and their role explicitly physician-centered8. On the one hand, the service model centered at the psychiatric hospital was in crisis and, on the other hand, efforts of MTSM defended the rights of psychiatric patients8,9.
The Brazilian Psychiatric Reform emerged from that juncture of democratization, it is much more that the sanction of new laws and standards and greater than the set of changes in government policies and health services2,8,9.
The psychosocial model care proposed provides for differing practices, placing emphasis on the de-institutionalization that can be understood as a process that involves the construction of meanings and projects for which occurs de-hospitalization, rebuild lives in society and face difficulties and disabilities9,10.
This model is regulated by Law 10.216/2001 which provides for the protection and rights of people with mental disorders and establishes that treatments should be used, preferably in community mental health services, with a view to social reintegration of persons with disorder mental in their midst11.
In this perspective, the PNSM proposes psychosocial care in the care for people with mental disorders, in order to overcome the assistance asylums, hospital-centric. Thus, the aid projects are aimed at creating a network of care with alternative services to the hospital2,8.
The Psychosocial Care Centers (CAPS) are important among the substitutive services offered, consider covering the care, emphasize the importance of the inclusion of the family in treatment and comply with the subjectivity of the user2,5,12.
The creation of the CAPS allowed the insertion of new actors in mental health services and changed the logic of organization of the work of the professionals, in addition to the hospital spaces. In view of this change, emerged the need to direct the practice of professionals, according to the psychosocial model, which emphasizes the interdisciplinary characteristics3, and is guided by the professional liability and the therapeutic bond structured to meet the integrality of the subject, in the promotion of psychosocial rehabilitation and guarantee the rights of citizenship4,6.
METHODOLOGY:
This research is part of a research project coordinated by the School of Nursing of Ribeirão Preto, University of São Paulo (EERP / USP), in the Faculty of Nursing, Federal University of Goiás (FEN / UFG) conducts studies in Goiás.
This is a descriptive study. The data collection was carried out between February and May 2011, in all the interior cities in the State of Goiás, which had public services of mental health, enabled until December of 2010, and which had workers of higher level acting in these services for more than three months. Faced with these criteria and the objective of this study included 19 municipalities and 22 services, all CAPS, because it is the only device that care had, until that moment, higher education professionals in the composition of the multi professional team.
At the time of data collection there were 114 workers of higher level, of which 14 have refused to participate in the study, totaling 100 participants. Thus, the participation corresponded to 87.7% of the subjects.
For the retrieval of data, the authors used an instrument developed by the group of researchers from the EERP/USP13. This instrument consists of a self-report form consists of open and closed questions with their answers coded, aiming to get as much information as possible to characterize the profile of the top-level workers and their actions.
The responses were entered into a Microsoft Excel spreadsheet, version 2003, with double space with the purpose of correcting possible errors. The characterization of professional graphic profile of the participants was performed using absolute and relative frequency percentages.
This study was approved by the Research Ethics Committee of the Federal University of Goias, in compliance with the guidelines of the CNS Resolution no. 196/96, with the protocol 303/10.
RESULTS AND DISCUSSION
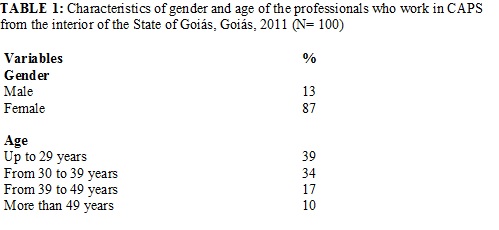
The characteristics of gender and age of the professionals who work in mental health services in the State of Goiás are shown in Table 1. The vast majority of them were female (87%), are young people, 73% of which were up to 39 years of age. On the other hand, around 10% of workers are more than 50 years of age.
Service workers surveyed are mostly female, following a trend also identified in other research13-16.
In the healthcare field there is a tendency to associate the female work with a relational content in situations of suffering and pain. This condition is related to the fact that the work be exercised mostly by nursing17. Although nurses have been the second most common occupational category, this assumption can also be considered in this study, as psychologists, who represented most other providers, have similarly centered their practices on relationships and caring for others.
The CAPS in he interior of Goiás has young workers, unlike those found in other studies14,16. This characteristic may be relevant to the extent that they can act in services with commitment and exploration of ideas, provided that they have had training consistent with the objectives of the Brazilian Psychiatric Reform.
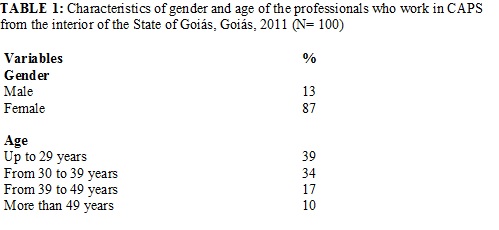
As regards the data concerning the training and qualification of higher education professionals who participated in this study, prevail the psychologists (35%), followed by nurses (16%), occupational therapists (12%) and social workers (11%), as shown in Table 2. The others who make up 17% of the professional working in the services surveyed are art therapists, pharmacists, physical therapists, music therapists, educators and physical education teachers. Physicians who work in the services surveyed represent 9% of the professionals who participated in the study, as many of these (13%) refused to participate and 3% worked in more than one CAPS in the State of Goiás, having been counted only once.
Global data reflect different context being that nurses form the largest professional category in the system of mental health, followed by psychiatrists. It is worth pointing out that the number of psychiatrists has been much more prevalent in high-income countries, where the median was 172 times higher than in low-income countries18.
It is worth mentioning that in many services the composition of the teams was reduced and the number did not meet the minimum legal requirements. Some of them did not have the participation of doctors and nurses or, mandatory occupational categories in mental health services like CAPS.
Interestingly, a significant representation of professionals from other classes in traditional and non-medical mental health services in the state of Goiás The results reveal the composition of multidisciplinary teams in CAPS researched, which is in accordance with the guidelines of the PNSM. This fact may indicate some progress in specialized assistance, to the extent that other professional categories, in addition to doctors and nurses, are included in the teams.
The WHO defines three groups of workers in mental health: the first consists of skilled workers, such as neurologists, psychiatric nurses, psychologists, social workers and occupational therapists. The second is formed by non-specialized health professionals and, the third, by other professionals, such as teachers and other workers in the Community6. Thus, it is evident that the specific composition of mental health workers should be varied and aligned with the existing health system18.
It is expected that the interdisciplinary work bring repercussions among users and their families in these services. For both, the team in CAPS and stimulated to organize themselves in a horizontal fashion and form a new collective to be able to meet the complexity of demands19.
For ethical reasons, the teams and their respective services were not described separately. It is noteworthy that the majority of sites visited (68%) by the researchers do not have a complete minimum team, with a general lack including psychiatrists. Given the scenario it was found possible to see the great scarcity of human resources in mental health services within the State of Goiás In addition, the lack of specialist in the area and also a factor to be considered as it may compromise the specific actions of health facing the clientele.
It was evidenced in the study that many professionals also act as coordinators of services for which they are crowded. This information is consistent with research conducted in the State of Mato Grosso, where the manager position was super-qualified with professional practice and did not provide any bonus salary for this purpose. In other words, it is noted that the work for which he will act both as a technician and manager in a single day's work, a condition that limits their participation in team20.
The multi professional characteristic and the basis for realization of the PNSM, that will make a difference in the quality of service to users of mental health services, if the exchange of knowledge and experience to meet the complexity of this area. Its objective, therefore, that the various specialties seek solutions to emerging problems21.
With this perspective in the team is no longer just a grouping of professional categories to work together in an interdisciplinary way to different demands and dimensions that the user presents19. The interdisciplinary approach aims to overcome the hierarchical relationships and other professionals behave beyond the therapeutic teams20.
Regarding the time of graduation, 73% of workers are trained up to a maximum of 10 years, being that 52% of them with up to 4 years, followed by 21% between 5 and 9 years of completion of the undergraduate course. There are few professionals who work in mental health care with more than 20 years of being graduated.
It is recommended specialized training to professionals in mental health, considering their specificity and complexity. Among the workers surveyed 21% have specialization course in the area, 42% in other and 37% do not have any skill.
It is undeniable that, in recent years, many changes have occurred in the implementation of public policies in the area of mental health, especially concerning the care paradigm, and many substitutive services were deployed. However, the influences that produce in daily reality is perceived as inadequate, especially within distant capital cities and metropolitan areas21.
There is a pressing need for changes in the abilities and attitudes of those involved in specialized assistance, in order that the psychosocial model produces effects that are consistent with the proposal of the Brazilian Psychiatric Reform. One of the possibilities of adequacy of practices in accordance with the current healthcare and the professional qualification paradigms. Empowering workers constitutes an action more than necessary, since many of them are generalists or have expertise in other areas of knowledge, in addition to having little time to experience and insertion in the services.
The fact that the majority of participants have Latu sensu training in another area may reflect the non-option for mental health. On the other hand hand, the low supply of courses in the State of Goiás, the fragility of employment of workers and the lack of political support these initiatives may explain the few specialists in mental health services in Goiás.
This reality provides little build critical to psychiatric centered model, the absence of social movements in mental health and the understanding of the Psychiatric Reform just as de-hospitalization20.
Study with network professionals’ specializing in mental health in the city of Goiânia-GO shows that claims for training programs in the field of mental health are mostly made by those newcomers in the services17.
The question of the specialization has been very focused since, in most cases, the singularities of mental health, PNSM and consequently the psychosocial model are ignored during academic education17,22. The training of professionals in the area of health is still considered to be a limiting factor because it is strongly marked by biological-medical paradigm at the expense of a more humanistic education20.
Whereas various professions work in mental health services and many of them were not in any way in the gym, content related to psychosocial assistance, it is possible to understand the difficulties of dialog between the areas of health and education can be an obstacle in the relationship of the staff to interdisciplinary practice17.
It is noteworthy; therefore, focus on the interaction of training professionals to work in mental health, in that interchange of the various areas of knowledge is an important requirement to execute the PNSM in Brazil. On this aspect, it is essential to develop methodologies for management and professional practices aiming at significant paradigm shift related to mental health that meet the expectations of the Psychiatric Reform and government proposals16,17.
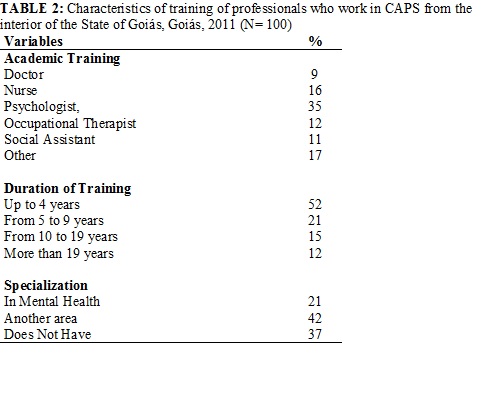
With relation to the contextualization of the work of the professionals who work in mental health services for the interior of the State of Goiás, it stands out that the vast majority (90 %) have little time for insertion into mental health, being that 76% of them have been active in the area for up to 4 years. Another significant result is related to the time that the professionals are linked to the surveyed institutions, revealing that 85% are crowded in CAPS there are less than 4 years, as shown in Table 3.
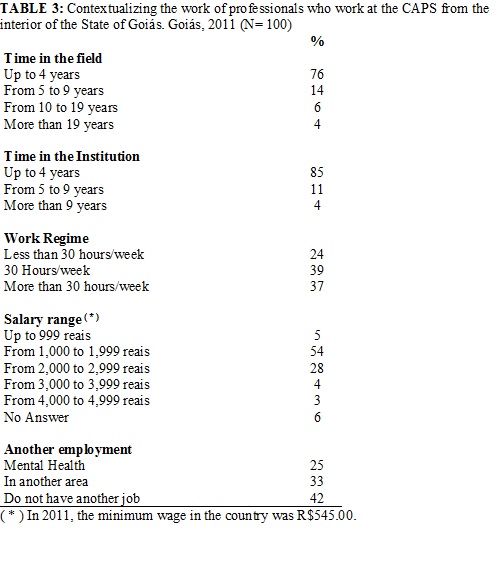
In addition to young professionals, the majority has little experience in the area (76 %) and a good proportion of them is inserted in services searched for less than 4 years (85%). However, It is worth mentioning that the majority of services are implemented for less than four years.
Professionals with experience in the mental health field may have difficulty working with users of services and feel dissatisfied with the projects17,19.
On the other hand, older and experienced workers that experienced conflicts and discussions arising from the reform movement are able to view more easily the advances that the psychosocial model has already reached19. Similarly, many of these professionals have made option for acting in the health care model proposed by PNSM, believing in the work that they are developing17.
In this sense, in the composition of the teams in mental health services, it is recommended that you rely on professionals who defend different models of previously applied, not to reduce the healthcare proposal the mere opening of substitutive services19.
In relation to the work regime, it was found that 76% of the employees are dedicated to the services approximately 30 hours per week. Considering the salary range, more than half (54%) receive between R$ 1,000.00 and R$ 1,999.00, followed by 28% who receive between R$ 2,000.00 and R$ 2,999.00. In spite of only five of the participants receiving less than R$ 1,000.00, these results show low remuneration of workers in the area.
More than half of the study participants (58%) reported having another job, being cited the mental health area by 25% of them.
The results of this study also demonstrated that the low wages of professionals, in addition to the workload of 30 or more hours per week. These are unfavorable conditions to work that can justify the search for another job to supplement their income.
Although the data collection instrument did not address the type of employment of professionals, contact with the teams during this procedure enabled us to verify that most of them have a temporary contract with the municipality in which they are working.
Qualitative Studies with mental health workers conducted in Brazil demonstrate the fragility of employment relationships, poor working conditions, such as low pay and double shifts generating reasons for dissatisfaction with thier work in mental health3,17,19-21.
This context does not favor the permanence of professionals in services, cause de-motivation and can negatively influence the work process of their teams in services20-22. Thus, the bonds, the turnover of workers and working time should be considered as aspects which hinder specialization of the professionals22.
In fact, it is reaffirmed the questioning of how teams so low as those found in this study and with conditions of training and work so vulnerable, they can work all the complexities that mental health involves for all?20
Employment stability, appropriate structure and full team may promote the practice in mental health services because they allow for the integration of the team, the interdisciplinary work and the bond with the users and their families.
In light of the results of this study, it reiterated that one of the main challenges for the process of consolidation of the Brazilian Psychiatric Reform: the training and development of human resources, whose process requires ever more theoretical-technical aspects and attitudinal of workers to act with quality service to users of health services.
CONCLUSION
The results revealed that the workers in the mental health services in the interior of the State of Goiás are of several professional categories, characterizing the multidisciplinary work. The majority of them are young, with little time to completion of graduation and have limited experience in the mental health area, with rare exceptions. The employment relationships are fragile and wages very low when compared with other Brazilian localities.
Even if the public services of mental health of the interior of the State of Goiás have workers of several professional categories, the fact that they have little time to completion of the undergraduate course and limited experience in the mental health area can compromise the effectiveness of the PNSM in the State.
Similarly, the work conditions which the area offers signals weakness in specialized assistance compromising the principles suggested by psychosocial model, in particular those who value substantially the bond between the user and the professional.
This study highlights the lack of investment in human resources in the mental health field, highlighting the imminent need for investments in the training of professionals who work in mental health services of the State of Goiás and improvements in working conditions, such as strengthening of employment relationships and remuneration consistent with the professional performance.
As a result of switching from state government, at the beginning of the year 2010, there were many changes of contracts of workers by the municipalities. It is therefore considered that the data collection instrument was limited because it does not allow the identification of the form of recruitment and selection of workers, as well as detailed information about the type of employment relationship of professionals.
Finally, the results can be generalized to the interior of Goiás, considering that almost all workers working in it were included in the study. It is noteworthy; however the need for further research on the influence of these professional graphic characteristics evidenced in the work process, the actions developed by the professionals and the impact of psychosocial care within the State.
REFERENCES
1. Amarante P, Torres E. A constituição de novas práticas no campo da atenção psicossocial: análise de dois projetos pioneiros na Reforma Psiquiátrica no Brasil. Saúde Debate. 2001; 25(58):26-34.
2. Wetzel C, Kantorski LP, Souza J. Centro de Atenção Psicossocial: trajetória, organização e funcionamento. Rev enferm UERJ. 2008; 16:39-45.
3. Guimarães JMX, Jorge MSB, Assis MMA. (In)satisfação com o trabalho em saúde mental um estudo em Centros de Atenção Psicossocial. Ciênc saúde coletiva. 2011; 16:2145-54.
4. Jorge MSB, Pinto DM, Quinderé PHD, Pinto AGA, Sousa FSP, Cavalcante CM. Promoção da Saúde Mental - Tecnologias do Cuidado: vínculo, acolhimento, co-responsabilização e autonomia. Ciênc saúde coletiva. 2011; 16:3051-60.
5. Mielke FB, Kantorski LP, Jardim VMR, Olschowsky A, Machado MS. O cuidado em saúde mental no CAPS no entendimento dos profissionais. Ciênc saúde coletiva. 2009; 14:159-64.
6. World Health Organization (WHO). Mental health atlas: 2011. Geneva (Swi): WHO; 2011.
7. Petersen I, Lund C, Stein DJ. Optimizing mental health services in low-income and middle-income countries. Curr Opin Psychiatry. 2011; 24: 318-23.
8. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Coordenação Geral de Saúde Mental. Reforma psiquiátrica e política de saúde mental no Brasil. Documento apresentado à Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. Brasília (DF): PAHO; 2005.
9. Amarante PDC. O homem e a serpente: outras histórias para a loucura e a psiquiatria. Rio de Janeiro: Ed. Fiocruz; 1996.
10. Dutra VFD, Rocha RM. O processo de desinstitucionalização psiquiátrica: subsídios para o cuidado integral. Rev enferm UERJ. 2011. 19: 386-91.
11. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Coordenação Geral de Saúde Mental, Álcool e Outras Drogas. Saúde Mental no SUS: as novas fronteiras da Reforma Psiquiátrica. Relatório de Gestão 2007/2010. Brasília (DF): Ministério da Saúde; 2011.
12. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Saúde mental no SUS: os centros de atenção psicossocial. Brasília (DF): Ministério da Saúde; 2004.
13. Furegato ARF, Osinaga VLM, Galera SAF, Pillon SC. Avaliação de instrumento para diagnóstico das atividades dos profissionais de saúde mental: estudo piloto. Cad Bras Saúde Mental. 2010; 1(2):23-37.
14. Mielke FB, Kantorski LP, Jardim VMR, Olschowsky A. Avaliação de um serviço substitutivo em saúde mental. Cogitare Enferm. 2009; 14(1):52-8.
15. Furegato ARF, Galera SAF, Pillon SC, Santos JLF, Pitia ACA, Cardoso L. Characterizing mental healthcare service teams. Rev salud pública. 2010; 12: 732-43.
16. Jorge MSB, Guimarães JMX, Nogueira MEF, Moreira TMM, Morais APP. Gestão de recursos humanos nos Centros de Atenção Psicossocial no contexto da política de desprecarização do trabalho no Sistema Único de Saúde. Texto contexto - enferm. 2007; 16:417-25.
17. Silva EA, Costa II. Saúde mental dos trabalhadores em saúde mental: estudo exploratório com os profissionais dos Centros de Atenção Psicossocial de Goiânia/GO. Psicol em Revista. 2008; 14(1):83-106.
18. Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, et al. Human resources for mental health care: current situation and strategies for action. Lancet. 2011; 378: 1654-63.
19. Pinho LB, Hernández AMB, Kantorski LP. Trabalhadores em saúde mental: contradições e desafios no contexto da reforma psiquiátrica. Esc Anna Nery. 2010; 14: 260-7.
20. Oliveira AGB. Trabalho e cuidado no contexto da atenção psicossocial: algumas reflexões. Esc Anna Nery. 2007; 10: 694-702.
21. Antunes SMMO, Queiroz MS. A configuração da reforma psiquiátrica em contexto local no Brasil: uma análise qualitativa. Cad Saúde Pública. 2007; 23: 207-15.
22. Rézio LA, Oliveira AGB. Equipes e condições de trabalho nos centros de atenção psicossocial em Mato Grosso. Esc Anna Nery. 2010; 14: 346-54.