Source: Non-Conformity Reports
ORIGINAL RESEARCH
Mapping of medication errors at a university hospital
Mileide Morais PenaI; Aline Togni BragaII; Ellen Meireles MeirelesIII; Luciana Gomiero Cugler Vassao IV; Marta Maria MelleiroV
I
RN. Ph.D. Nursing Manager. Hospital of Pontifical Catholic University of
Campinas. São Paulo, Brazil. E-mail: mileidempena@gmail.com
II
RN. Ph.D. Coordinator of Quality. Hospital of Pontifical Catholic
University of Campinas. São Paulo, Brazil. E-mail: alinetogni@yahoo.com.br
III
RN. Assessor of Quality. Hospital of Pontifical Catholic University of
Campinas. São Paulo, Brazil. E-mail:
ellen-meireles@hmcp.puc-campinas.edu.br
IV
Pharmacist. Hospital of Pontifical Catholic University of Campinas. São
Paulo, Brazil. E-mail: lu_gomiero@hotmail.com
V
RN. Associate Professor, Department of Professional Orientation, School of
Nursing, University of São Paulo, São Paulo, Brazil. E-mail: melleiro@usp.br
DOI: http://dx.doi.org/10.12957/reuerj.2016.7095
ABSTRACT
Objective: to identify medications errors at a university hospital, classify them by root cause and examine their main causes. Method: this retrospective, quantitative, descriptive study was conducted at a university hospital in São Paulo State. The study sample comprised 339 medication errors occurring in 2010. Data were collected in March 2011 by non-conformity reports. Results: the main safety failure occurred at dispensation (40.4%) and the root cause was workforce-related (85.8%). When errors were classified by the Nine rights, 43.4% related to right medication. Conclusion: the predominance of errors caused by workforce failures indicates that awareness, training and continued professional development are fundamental to safety in the work of multi-professional teams.
Keywords: Medication errors; medication systems; patient safety; nursing.
INTRODUCTION
Health quality occurs when care is provided to patients to increase the probability of desired recovery and reduce the probability of undesirable events1.
Health quality is closely linked to the adoption of measures to ensure patient safety during all service processes.
Errors in health care result from unintentional actions, which result in failures during patient care and may be made by any member of staff at any stage of care, especially during the preparation and medication administration process. Thus, the term patient safety involves the prevention of errors in care and the elimination or reduction of damages to the patient2.
Administration of medication is one of the most frequent actions in hospitals, but may result in errors in various stages of the process. Such errors cause harm to patients, among them not receiving medication to injuries and deaths. Drug interactions can also result in damage to the patient, especially in intensive care units (ICU) due to the use of multiple drugs3.
The medication error is an avoidable event and is related to professional practice, the product used, the procedure, to prescription, labels, packaging, preparation, dispensation, distribution and monitoring 2.
One way of assessing the quality of health services is the implementation of so-called indicator instruments, which are measures used to determine, over time, the functions, processes and outcomes of an institution. The use of indicators enables healthcare professionals to monitor and evaluate events that affect patients, professionals and organizations, pointing to the needs and expectations of patients4.
In this perspective, it is imperative to provide conditions so that professionals can take possession of preventive measures, addressing the events constructively in the search for the root cause and decrease occurrences.
The objective of this study was to identify medication errors at a university hospital, classifying them according to the root cause and analyzing their causes.
THEORETICAL FRAMEWORK
The report "To err is human: building a safer health system of Institute of Medicine", published in 1999, points to 98,000 death-cases related to health system errors in the United States, and other adverse events5.
Among the incidents that affect patient safety, those related to drugs deserve special attention from hospitals, as epidemiological studies in the United States estimate that every hospitalized patient is subject to a medication error per day and approximately 400,000 related adverse events drug occur per year6.
In Brazil, the number of studies conducted in the last decade evidences the concern about the impact of medication errors in patient safety7 .
In this sense, a multicenter study of medication errors, conducted in five Brazilian hospitals, identified 1500 medication errors, showing that 30% of the applied doses were faulty8.
A cross-sectional study conducted in a university hospital with a sample of 735 admissions9 estimated the prevalence of medication-related incidents at 48%.
Moreover, another research cited the lack of knowledge as being a key contributor to these events10.
Medication errors have been studied from the most different of perspectives, identifying types and frequencies of errors, analyzing the impacts of packaging and similar labels, dispensing errors, and the influence of external factors during the preparation and administration of drugs and measures to minimize errors11-15.
An US non-governmental organization, dedicated to studies of the drug chain, suggests the following classification for medication errors: dose omission, improper dose, wrong concentration, wrong drug, formulation of the wrong dose, wrong technique, wrong route of administration, wrong speed, wrong time, wrong moment, wrong patient, wrong monitoring and management deteriorated drugs16.
Medication errors can also be categorized when there is non-compliance with one of the Nine Certain Medication: right patient, right medication, right route, right dose, right time, and right record, knowing the action, pharmaceutical form and monitor the effect 17 .
In order to reduce medication errors and propose preventive measures, a constant and careful analysis of events within health institutions is necessary.
One method that has been used to deepen in medication errors is the root cause analysis, incorporated in 1997 by Joint Commission on Accreditation of Healthcare Organization (JCAHO), uses the Ishikawa Diagram or Cause and Effect Diagram to elaborate the causal chain. It starts from an unwanted final event in order to find the root cause, proposing to prevent and prevent new mistakes to occur2.
A Brazilian study evaluated medication errors using the root cause analysis and identified 74 medication errors during the preparation and administration of drugs by the nursing staff. Dose errors (24.3%), time errors (22.9%) and unauthorized medicinal products (13.5%) were the most frequent. Multiple factors contributed to the occurrence of errors and strategies and recommendations were presented to avoid them2.
METHODOLOGY
This is a quantitative, descriptive and retrospective study in a private, large, tertiary level university hospital, located in the state of São Paulo. It has 350 beds, with 262 beds to meet the Unified Health System (SUS) and 88 to service private and private agreements. It has six inpatient units (pediatric, psychiatric, medical clinic, surgical, obstetric and infectious diseases); four intensive care units (adult, infant, neonatal and coronary); three emergency care units (adult, child and gynecological) and two clinics, totaling about 2,100 employees.
The study consisted of 339 Noncompliance Reports (RNC) related to medication errors that occurred in 2010.
The recording of events is voluntary and can be realized by any professional institution, in order to raise, analyze and propose interventions for the events.
Data collection took place in March 2011, after authorization of the institution in question and guaranteed anonymity.
The events were analyzed individually, in order to raise the root cause of the problem and then classified according to the nine Certain 17:
Data were analyzed using the Ishikawa Diagram or Cause and Effect Diagram to identify, explore, highlight and map factors that could affect a certain outcome and demonstrates the relationship between a quality characteristic (effect) and the factors that influence it (causes) for the occurrence of the event. The diagram analyzes the causes of errors through 6M (Method, Manual Labor, Materials, Measurement, Environment and Machine2).
Data were stored in an Excel spreadsheet and analyzed using descriptive statistics. The results were presented in tables.
RESULTS AND DISCUSSION
According to the RNC analyzed, 339 medication errors were reported in 2010, including near miss or near misses.
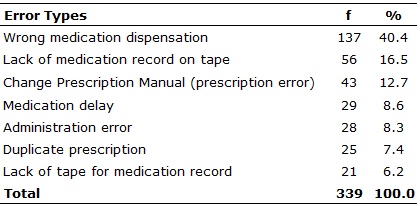
Distribution of 339 medication errors were identified: 137 (40.4%) dispensations wrong medication, 56 (16.5%) shortages of medication records on tape, 43 (12.7%) manual changes prescription, 29 (8.6%) delays medications, 28 (8.3%) administration errors, 25 (7.4%) prescriptions in duplicate and 21 (6.2%) tape faults for medication records of the period, as explained in Table 1.
TABLE 1:
Distribution of medication error types identified. São Paulo (SP), Brazil,
in 2010.
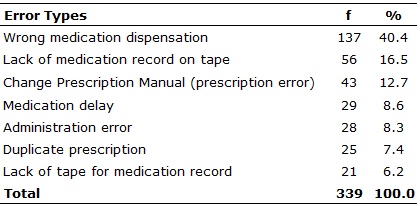
Source: Non-Conformity Reports
The drug delivery system used in the institution is the turn-based dispensing system: morning (8: 00h to 13: 59h), afternoon (14: 00h to 21: 59h) and night (22:00 to 7: 59h). The prescription is computerized and the system itself takes care of the timing, following the frequency set by the doctor. Each prescription generates a mirror, in turn, to the pharmacy. Pharmacy technicians receive the mirrors and separate medications per shift, putting the tapes medications to be delivered in the units at set times. Three lectures by pharmacy technicians and an electronic conference through bar code are performed. After the delivery of medications in the units, nursing performs the conference, preparation and administration thereof.
The main medication error events are related to the above procedure. If the dispensing errors, lack of medication in the medication tape and lack of tape on period are added, a 63.1% rate of errors is obtained in this step of the process, despite the various stages of aforementioned conference. This suggests failure to meet the established process, which may indicate a low adherence to standard operating procedure.
Comparing the dispensing error rates found in literature, especially the methodological diversity of existing studies is not a simple task.
A study conducted in Salvador, Bahia, found a lower rate of 29% for dispensing errors in 324 prescriptions in the year 2009 and 11% in 317 prescriptions of 201210. Multiple factors can influence this process, as the presence of the pharmacist, following the work of pharmacy technicians and the process as a whole. An important assignment of the pharmacist is the evaluation of drug prescriptions, preventing errors from propagating to the administration of the drug.
It discusses the importance, necessity and applicability of clinical pharmacy as a key activity to be developed in conjunction with the health team, aimed at patient safety, effectiveness of the proposed treatment and rational use of drugs. The pharmaceutical care, and pharmaceutical therapeutic needs of the individual, must ensure a safe and effective therapy, including control mechanisms to facilitate continuity of care18.
Not only the medication lag error, but also dispensing errors, lack of medication records on tape and lack of tape for medication records of the period, may result in delay in the administration of medication to the patient, incurring reduction the effectiveness of the treatment and possible damage.
In addition, the conference of the medications performed by nurses before the preparation and administration thereof, prevents drugs dispensed are wrongly administered to the patient, ensuring their safety. Note that in this study the nursing staff identified all dispensing errors at the time of the conference.
Within the distribution of medication errors according to the root cause, it was found that in 291 (85.8%) events, the prevalent cause was related to manual labor (failure of professionals), as shown in Table 2.
TABLE 2:
Distribution of medication errors according to the root cause. São Paulo
(SP), Brazil, in 2010.
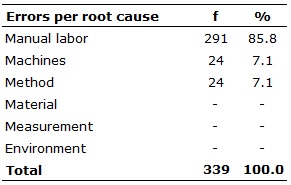
Human errors relate to institutional, financial and structural issues. The occurrence of errors should be interpreted as failure due to breakdowns of the technical and organizational systems related to health care, and not as isolated actions of professional results19,20.
Hospital care is complex and multidisciplinary, based on technical knowledge and information about the patient, the result of interrelated decisions in which the professional develops a modus operandi, performing the job. In this scenario, one may expect a high failure probability13.
Lack of preparation, lack of professionalism and oversight are considered risk factors for the occurrence of adverse events12. Another study finds distraction and fatigue (64.9%), misreading of labels ampules or syringes (54.4%), psychological pressure to the procedure (21%) and inadequate storage (19%) as contributors to the medication error 21.
Moreover, mistakes made by professionals can occur due to work overload; lack of knowledge in mathematical operations; little knowledge of the administered medications, making it difficult to care for differing dosages and increasing the risk for inadequate dilutions. Specifically, when faced with the reality of nursing professionals, it is found that distraction is an important element that can lead to professional errors. This situation can be evidenced when the professional is interrupted by others, such as the patient or even a co-worker; the phone ringing; a crying child, and other noises and factors that divert attention at the time of preparation and administration of the drug11.
Faced with such complexity, it we believe in the reinforcing of three strategies: communication, continuing education and compliance with policies and procedures for the drug chain12.
Communication is the best way to prevent human errors or improve the technical and system deficiencies. However, people often choose silence. In healthcare environments, often those that detect a problem want to talk, but they are ignored. Silence can be caused by fear or the desire to avoid transmitting unwanted news, and the pressures suffered by groups22.
It is essential to develop strategies for the notification of errors not linked to punishment but serving as a learning tool. Similarly, they should be analyzed in a multidisciplinary way, so that preventive and corrective measures are implemented, ensuring quality in the care process12.
In the literature there are various definitions and classifications for the types of medication errors. In this study, we chose to use the classification as the Nine Certain Medication, described above and shown in Table 3.
It was found that 147 (43.4%) errors were related to certain medication, 93 (27.4%) to the right record, 41 (12.1%) to the right patient, 38 (11.2%) at the right time 11 (3.2%) the right way, 9 (2.7%) the right dose. No notification was occurred for action, form or right answer.
TABLE 3:
Distribution of medication errors according to the Nine Certain - São Paulo
(SP), Brazil, in 2010.
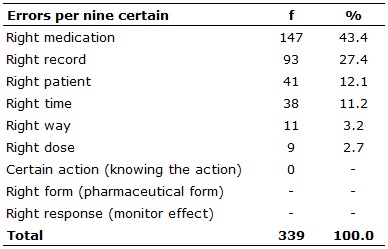
It can be inferred that the right medication-related errors, right patient, right time, right route and dose are the result of dispensing errors, lack of tape for medication records or lack of medication records on tape, error or administration delayed and prescription in duplicate; while errors related to certain registration incur manual prescription change.
A study conducted in a university hospital in Ribeirão Preto, São Paulo, pointed dose errors (24.3%) as the most frequent, correlating them to dispensing drugs in doses different from the ones prescribed2.
The drug delivery system is an important factor in the prevalence of dispensing errors. Since the 1960s, several studies provide information about the influence of the drug distribution system in medication errors, indicating that the unit dose system is safer because it allows greater participation of the pharmaceutical and reduce the continuing medication in treatment units10.
A multicenter study involving four hospitals in different regions of the country identified high error rates in the preparation and administration of medications. The authors suggest that to improve safety in drug-delivery systems, it is necessary to adopt changes in institutional culture, aiming to achieve concrete improvements23.
Literature notes that medication errors are identified and that their frequencies vary from one study to another, as this process differs per each institution having its own characteristics that need to be identified by researchers to aid in the analysis of errors22-25.
The proper patient identification is also required for safe drug administration since patients with similar names admitted in one unit; they can easily be confused, starting to receive an improper dose for the treatment or even incorrect medication24.
Error prevention should be based on the search for real causes that usually include errors in the service organization systems. Mistakes should be accepted as evidence of failure in the system and seen as an opportunity to review the process and improvement of patient care8.
It emphasizes the need of stimulating the culture of safety, which will discuss the next team, prevention strategies to ensure safe care in health institutions25.
CONCLUSION
This study made it possible to diagnose that the major security flaw of the drug chain occurs in the dispensing step and the root cause of these errors is related to labor. Importantly, the nursing staff did not administer medications dispensed erroneously due to the conference process it runs.
Another relevant fact is that most errors were related to the lack of the correct conferring of medicine. This reinforces the importance of adequate pharmaceutical services, ensuring that the patient receives the right medication (prescribed); on the track and in the appropriate dosage form; the correct doses and schedules, through activities related to the analysis of prescribing and dispensing end of the conference.
It recognizes that a safe patient care depends on interventions in the processes that make up the dispensation, preparation and administration of drugs, mainly to impose safety barriers, to avoid mistakes and minimize risks to patients.
It appears that awareness, training and continuing education process are essential for the multidisciplinary team to be able to act in processes underlying the drug chain.
A limitation of this study refers to the underreporting of events, due to feelings of guilt and fear of punishment, reported by the professionals themselves, which may have influenced the size of the sample. However, it is possible to consider the data found to support programs and modifications within the health institutions as well as for further studies.
REFERENCES
1. Joint Commission on Accreditation of Healthcare Organization [internet]. About US. [cited 2016 Aug 28] Available from: http://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx
2. Teixeira TCA, Cassiani SHB. Root cause analysis: evaluation of medication errors at a university hospital. Rev esc enferm USP. 2010; 44(1):139-46.
3. Silva LT, Santos MM. Drug interactions in intensive care unit: a review to substantiate nursing care. Rev enferm UERJ. 2011; 19(2): 134-9.
4. Lima CSP, Barbosa SFF. Occurrence of adverse events as indicators of quality of care in an intensive care unit. Rev enferm UERJ. 2015; 23(2): 222-8.
5. Kohn LT, Corrigan JM, Donaldson. To err is human: building a safer health care system. Washington (DC): The National Academy Press; 1999.
6. D'Aquino FFR, Juliani CMCM, Lima SAM, Spiri WC, Gabriel CS. Drug-related incidents in a hospital: input to improving management. Rev enferm UERJ.2015; 23(5):616-21.
7. Silva LD, Barbosa SF, Prado ML, Dal Sasso GTM. The production of Brazilian nurses about medication errors in adults patients: a bibliographic review. Evidentia [LATINDEX] 2011 [cited 2016 Aug 28]. 8(34). Available from: /evidentia/n34/ev7357p.php
8. Reis AM, Marques TC, Opitz SP, Silva AEBC, Gimenes FRE, Teixeira TCA et al. Errors in medicine administration – profile of medicines: knowing and preventing. Acta Paul Enferm. [Scielo-Scientific Electronic Library Online] 2010 [cited 2016 Jul 20]. 23(2):181-6. Available from: http://www.scielo.br/pdf/ape/v23n2/05.pdf
9. Paranaguá TTB, Bezerra ALQ, Santos ALM, Silva AEBC. Prevalence and factors associated with incidents related to medication in surgical patients. Rev esc enferm USP [Scielo-Scientific Electronic Library Online] 2014 [cited 2016 Aug 28].48(1):41-7. Available from: http://www.scielo.br/pdf/reeusp/v48n1/0080-6234-reeusp-48-01-41.pdf
10. Faria LM, Cassiani SH. Medication interaction: knowledge of nurses in intensive care units. Acta Paul Enferm [Scielo-Scientific Electronic Library Online] 2011[cited 2016 Jul 20]. 24(2): 264-70. Available from: http://www.scielo.br/pdf/ape/v24n2/en_17.pdf
11. Lopes DMA, Néri EDR, Madeira LS, Souza Neto PJ, Lélis ARA, Souza TR et al. Analysis of similar drug labeling: potential medication errors . Rev Assoc Med Bras. 2012; 58(1):95-103.
12. Galvão AA, Oliveira AM, Carvalho FB, Araújo RPC. Identification and distribution of dispensing errors in a hospital pharmacy: a comparative study in Salvador Bahia. Rev Cienc Med Biol.2012;11(1):201-6.
13. Lemos RF, Silva VR, Martinez MR. Factors that predispose to the distraction of the team of nursing during the preparation and the administration of medicines. Rev Min Enferm. 2012;16(2):201-7.
14. Santana JCB, Sousa MA, Soares HC, Avelino KSA. Fatores que influenciam e minimizam os erros na administração de medicamentos pela equipe de enfermagem. Enferm Rev [LATINDEX] 2012 [cited 2016 Aug 28]. 15(1):122-37. Available from: http://periodicos.pucminas.br/index.php/enfermagemrevista/article/view/3300/3657
15. Silva LD, Camerini FG. Analisys of intravenous medication administration in sentinel network hospital. Texto contexto - enferm.2012;21(3):633-41.
16. NCC MERP Taxonomy of medication errors [internet]. 2001 [cited 2016 Jul 20]. Available from: http://www.nccmerp.org/pdf/taxo2001-07-31.pdf
17. Elliott M, Liu Y. The nine rights of medication administration: an overview. British J Nurs. 2010; 19(5):300-5.
18. Bernardi EAT, Rodrigues R, Tomporoski GG, Andrezejevski VMS. Implementation of pharmaceutical evaluation of the prescription and the actions of clinical pharmacy at a Cancer Hospital in southern Brazil. Rev Esp Saúde. 2014; 15(1):29-36.
19. Pereira FGF, Caetano JA. Human error and patient safety in health services. Rev Enferm UFPI. 2014; 3(1):115-9.
20. Novaretti MCZ, Santos EV, Quitério LM, Daud-Gallotti RM. Nursing workload and occurrence of incidents and adverse events in ICU patients. Rev Bras Enferm. 2014; 67:692-9.
21. Erdmann TR, Garcia JHS, Loureiro ML, Monteiro MP, Brunharo GM. Profile of drug administration errors in anesthesia among anesthesiologists from Santa Catarina. Rev Bras Anestesiol. 2016; 66(1):105-10.
22. Okuyama A, Wagner C, Bijnen B. Speaking up for patient safety by hospital-based health care professionals: a literature review. BMC Health Serv Res. 2014; 14(61):1-8.
23. Costa LA, Valli C, Alvarenga AP. Medication dispensing errors at a public pediatric hospital. Rev Latino-Am Enfermagem. [Scielo-Scientific Electronic Library Online] 2008 [cited 2016 Aug 28]. 16(5):1-15. Available from: http://www.scielo.br/pdf/rlae/v16n5/pt_03.pdf
24. Gimenes FRE, Mota MLS, Teixeira TCA, Silva AEBC, Opitz SP, Cassiani SHB. Patient safety in drug therapy and the influence of the prescription in dose errors. Rev Latino-Am Enfermagem [Scielo-Scientific Electronic Library Online] 2010 [cited 2016 Jul 20].18(6): [07 telas]. Available from: http://www.scielo.br/pdf/rlae/v18n6/pt_03.pdf
25. Duarte SCM, Stipp MAC, Silva MM, Oliveira FT. Adverse events and safety in nursing care. Rev. Bras. Enferm. [Scielo-Scientific Electronic Library Online] 2015 [cited 2016 Aug28]. 68(1):144-54. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672015000100144&lng=en