RESEARCH ARTICLES
The use of the posterior tibial nerve electrical stimulation in the treatment of urinary incontinence
Andrelise Viana Rosa TomasiI; Gesilani Júlia da Silva HonórioII; Silvia Maria Azevedo dos SantosIII; Karina BrongholiIV
IPhysical Therapist. Master of the Graduate Program in Nursing at the Federal University of Santa Catarina. Participant of the group of studies on Health Care of the Elderly. Florianópolis, Santa Catarina, Brazil. E-mail: andrelisev@gmail.com.
IIPhysical Therapist. PhD student of the Graduate Program in Nursing at the Federal University of Santa Catarina. Participant of the group of studies on Health Care of the Elderly. Professor of the Course of Physiotherapy of Estácio de Sá University Center of Santa Catarina. Florianópolis, Santa Catarina, Brazil. E-mail: gesilani@hotmail.com.
IIINurse. PhD in Nursing. Professor in the Department and the Graduate Program in Nursing at the Federal University of Santa Catarina. Leader of the group of studies on Health Care of the Elderly. Florianópolis, Santa Catarina, Brazil. E-mail: silvia@ccs.ufsc.br.
IVPhysical Therapist. Master in Neurosciences. Professor of the course of physiotherapy of Estácio de Sá University Center of Santa Catarina.Florianópolis, Santa Catarina, Brazil. E-mail: karinab@live.estacio.br.
DOI: http://dx.doi.org/10.12957/reuerj.2014.6779
ABSTRACT: The aim of this study was to evaluate the electro-stimulation in the posterior tibial nerve for the treatment of urgent or mixed urinary incontinence. It is an almost experimental study with eight patients with a diagnosis of urinary incontinence of urgency or mixed, developed in Santa Catarina State –Brazil, in 2010. The assessment included physiotherapy evaluation form, voiding diary questionnaire quality of life from King’s Health Questionnaire. Twelve attendances of 30 minutes each were carried out, with electrical stimulation in the posterior tibial nerve. The results show a reduction in the frequency of daytime urinary incontinence in 62% of patients, a decrease in nocturnal urinary frequency in 37.5%, reduction in the amount of urinary leakage from severe to moderate and moderate to mild. There was no significant difference in scores on the questionnaire of quality of life after treatment. It is concluded that the method had a positive impact on patients compared to involuntary urine loss and the amount of urine lost.
Keywords: Urinary incontinence; electrical stimulation; tibial nerve; life quality.
INTRODUCTION
Urinary incontinence (UI) is defined by the International Continence Society (ICS) and the International Urogynecological Association (IUGA) as any involuntary urine complaint1. The loss of urinary continence is an uncomfortable and embarrassing condition, multifactorial origin and generator of exclusion, since it interferes with the physical and mental health of the people, thus compromising their quality of life2.
Urgency urinary incontinence (UUI) is defined as an overwhelming desire to urinate that is hardly abolished3. This incontinence is caused by involuntary contractions of the detrusor (Hyperactivity) together with urethral relaxing, during bladder filling. Mixed urinary incontinence (MUI) is characterized by symptoms of UUI associated with stress urinary incontinence (SUI), which in turn is described as the involuntary loss of urine in the absence of detrusor contraction, the efforts, during a intra-abdominal pressure increase4.
Increased voiding frequency and nocturia is generally together with the symptom of urgency and they are defined respectively as the complaint to submit repeated urination during the day and wake up at night one or more times to urinate. In the literature, the increased frequency is characterized as more than eight daytime urinary frequency and nocturia as more than two urination at night5.
These symptoms are common during clinical diagnosis. Another modality that indicates UUI is the urodynamic examination, in which there is detrusor hyperactivity during cystometry, may be neurogenic or idiopathic. It is assumed that, in more than 90% of the time, the detrusor hyperactivity is idiopathic6. Another way to characterize the UI is the voiding diary. This diary can be considered an important tool for the correct diagnosis of the UI. Important variables can be extracted from voiding diary: the daytime and nighttime urine output, bladder functional capacity, the number of urination during the day and the night and the number of episodes of urinary loss7.
As the UI has a great impact on the quality of life of patients, an instrument for measuring the quality of life will make it possible to evaluate the result of treatment chosen and facilitate the comparison of studies carried out in different locations, using different treatments in similar populations. There are in the literature many questionnaires that address the quality of life of women with UI, being generic or specific instruments and which can be used for surgical treatments or conservatives. In Brazil, the questionnaire King's Health Questionnaire (KHQ) was translated and validated, which assesses both the presence of symptoms of UI, as their relative impact. The use of questionnaires as tools of evaluation of quality of life has been intensified on scientific research in recent years. With this, it is valued the opinion of patients about their health condition8-10.
There are several methods of treatment for UI, from conservatives to surgical. One of the conservative treatment modalities is electrical stimulation can be applied in several locations as perineal skin, sphincter, stimulation in the dorsum of the penis or on the clitoris nerve, those methods that have been tested in different types of patients, both with instability or detrusor hyperreflexia11.
The posterior tibial nerve is a mixed nerve containing motor and sensory fibers, exiting L4, L5, S1 to S3nerve root, sharing the same roots that innervate the bladder. Consequently, the direct stimulation of the nerve must inhibit afferent S2-S3, suppressing the activity of bladder12.13. Thus, a new form of electrical stimulation can come to meet the improvement of detrusor hyperactivity is the stimulation of the posterior tibial nerve. It is still not known physiological effect of Transcutaneous electrical stimulation of the posterior tibial nerve, but it is believed that it has the function to modulate the stimulation that reach the bladder through the reciprocal innervation. The electrical impulse generated by the current, would be conducted in a retrograde manner through the posterior tibial nerve to the hypogastric Plexus and, from this until the detrusor, decreasing their contractions14.
Therefore, the objective of this study was to evaluate the use of the posterior tibial nerve stimulation in the treatment of urgency or mixed stress urinary incontinence.
LITERATURE REVIEW
The posterior tibial nerve electrical stimulation inhibits the activity of the bladder through the somatic afferent fibers depolarization and lumbar sacral. The stimulation of afferent fibers provides the central inhibition of motoneurons vesical pre- lymph node directly in the bone marrow. The etiology of vesical hyperactivity is unknown, but the hypothesis is that there is an imbalance between excitatory and inhibitory impulses, which control the bladder, in this way, the action of this neuromodulation could restore the balance in the central nervous system12.13.
The electrical stimulation of the tibial nerve in the UUI and MUI treatment has been studied and discussed with subcutaneous insertion and surface electrodes, showing favorable results, becoming an option in cases of contraindication or intolerance to inadvertent electrical stimulation, where many women present discomfort with this kind of procedure. Therefore, the posterior tibial nerve electrical stimulation with adhesive electrodes does not present adverse effects, with ease of implementation and minimal costs, and may be an important method of treatment in women with UUI15.16. In some studies that used electrical stimulation with sub-dermal electrodes, mild side events were reported as moderate, inability to tolerate the stimulation, leg cramps, vasovagal response and dormancy during using the needle17.
Conservative treatment of urgency or mixed urinary incontinence with the use of the posterior tibial nerve electrical stimulation using self-adhesive electrodes is a safe technique and can reduce the discomfort caused by the involuntary loss of urine.
METHODOLOGY
It is an almost experimental study. The study population was composed of women with a history of urinary complaint, diagnosed through the urodynamic examination, performed by an urologist, during the months of July 2009 to January 2010, with a total of 30 patients. Of them, eight women with urgency or mixed urinary incontinence accepted to participate in the study.
Exclusion criteria were considered: immediate postoperative urogynecological surgery, pacemaker use, decompensated diabetes for over 6 months and performing other forms of treatment (medicine use) for urinary symptoms during the study.
The data were collected in the Clinical School of Physiotherapy of Estácio de Sá University Center of Santa Catarina, in the period from March to May 2010. This study was approved by the Ethics Committee in Research of Estácio de Sá University Center from Santa Catarina, opinion number 055/2009.
The data were obtained through an initial assessment with each patient, containing identification data, information on urinary incontinence, such as average time of urinary complaints, anthropometric data (height and weight), as well as gynecological and obstetric history. After the initial evaluation, patients were directed to fill correctly the voiding diary, for three consecutive days. The voiding diary data collection included the following variables: voiding frequency, nocturnal and daytime urinary loss (frequency and amount). The questionnaire of quality of life – KHQ was also applied.
12 sessions were held, twice a week, with application of Transcutaneous electrical stimulation in the posterior tibial nerve, lasting 30 minutes. Two self-adhesive electrodes were placed in the region of the tibial posterior, one next to the medial malleolus and the other to 10 inches apart, with the patients in supine position with their knees in extension and hip flexion and external rotation slightly. An electrical current of 1 Hertz (Hz) and 200 milliseconds was programmed into the appliance until it has observed a flexion of the fingers. Once located the posterior tibial nerve, the frequency of the unit was changed to 20 Hz and the intensity according to the patient's tolerance was 0-10 milliampere (mA) but below the threshold nerve motor18.
All sessions were conducted in the Clinical School of Physiotherapy of Estácio de Sá University Center from Santa Catarina. At the end of the treatment, the patients were reevaluated with the same instruments used in the initial assessment.
The identification of patients was kept in anonymity in accordance with the guidelines and standards for research involving human beings established by Resolution number 196 from the National Health Council of October 10, 1996. The patients signed an informed consent form after clarification of objectives and procedures that would be carried out.
For a description of the results of the study, the following parameters were considered: analysis of voiding diary changes of urinary parameters were observed. These changes served as clinical improvement criteria of incontinence, as daytime voiding frequency decline, and loss of urine.
For the statistical analysis of the difference of diurnal, nocturnal voiding frequency, pre and post treatment urinary losses and scores of domains of quality of life questionnaire, the Wilcoxon test was done with a significance level of p < 0.05.
RESULTS AND DISCUSSION
The average age of women studied was 62.4 years old. These results are in agreement with the literature, the average age in the studies are among 56.4 or 61.5 years old. Therefore, the more frequently was in women over 50 years old19.20. This is also confirmed in this study, because only a patient was less than 50 years old, and all the others were above this age.
Lifestyle and behavioral interventions in the treatment of UI are associated with higher risk for having symptoms, being obesity a risk factor in men and women, where the increase in intra-abdominal pressure can lead to a chronic stress on the pelvic floor21. This confirms the results obtained through the participants of this research, in which the average body mass index was 27.8 kg/m², with four patients showing overweight and two patients with grade I obesity.
Regarding the time of duration of urinary complaints in women participating in another study, the maximum average was 4.5 years12. In this way, it is observed that the participants in this study were exposed for a longer time with an average of 5.1 years. The reason for the delay in seeking solutions for the various types of UI occurs due to the shame and embarrassment felt by the patients, by ignorance or ability by the health professionals, and during routine medical consultations this matter not usually spoken or investigated22.
In this study, most of the patients were in the climacteric, corroborating other studies published in the literature, indicating that the UI is presented in 35% of women in climacteric23.24. Another risk factor is the gynecological surgical procedures, especially hysterectomy, women undergo more frequently, because the removal of the uterus compromises the proper functioning of the muscles of the pelvic floor, which can cause damage to the support of the bladder and urethra, and be responsible for the increasing prevalence of UI25. In this study, it was identified that 07 women held some sort of gynecological surgery or urology, 06 of them performed a hysterectomy. Based on the obstetric history, it was noted that only one patient had no pregnancy, the others had more than one pregnancy. In relation to childbirth, the participants held one or more vaginal births. Childbirth can lead to some injury to perineum distension consecutive, and may affect the skin element (skin, vaginal mucosa), the fibrous ligament elements, the element of nervous and muscular structures. Many factors, such as the more than one childbirth, macrosomic fetuses, a prolonged phase of labor and the use of instrument for assistance such as forceps, have been linked to increased risk factors for UI26.
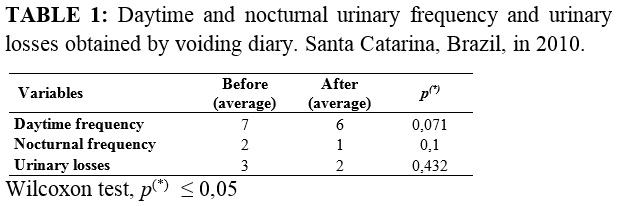
Therefore, when compared with Cesarean delivery, vaginal childbirth alone is not the cause of UI and when associated with injury or trauma to the pelvic floor and other risk factors27. Regarding the perineal outcome in one study, it was observed that from 6,365 vaginal births, 4,542 had some kind of spontaneous laceration or episiotomy28. This study demonstrates the great prevalence of injury in perineum during vaginal birth, considering as a risk factor for the symptoms of UI. This type of lesion increasingly has to be researched, because in one study it was observed 6 months after giving birth vaginally, women still reported pain in the perineum and changes in episiotomy healing29. This study identified reduction of diurnal and nocturnal frequencies after the assitance, with no significant difference. In relation to urinary losses among the participants, these occurred at most seven times before treatment, and at the end, there was a reduction to two losses. From participants, three did not report a loss at the end of treatment and the other five have decreased the amount of loss. These data were collected through the micturitional diary, filled by patients before and after treatment, as shown in Table 1.
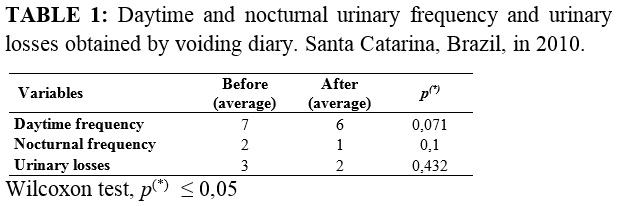
About the data related to urinary loss in the present study, there was a decrease in the frequency of daytime voiding of 5 (62%) of the participants. These results are in agreement with the literature, since it meets, as indexes of improvement, 50% to 70% of the participants, registered in the diary voiding30.
Regarding the nocturia, it is difficult to compare with other results of literature, as there are differences between the characteristics of the samples. In a study related to problems of neurogenic origin, there have been more than 50% on urinary frequency overnight in 20 patients studied, unlike the present study12. In another study, it was observed a reduction of nocturia during treatment, from 2.38 per night for urination to 1.14, being this significant result31.
About electrical stimulation to the UI, it is observed that its use in the posterior tibial nerve produced a significant decrease in some studies described in the literature. These findings are in articles that did not use the same inclusion criteria of this study, but who performed the treatment with patients with UI idiopathic origin11.12.32.
In this study, 05participants presented urine leakage after applying the posterior tibial nerve electrical stimulation, but it was observed an improvement in quantity, of intense to moderate and moderate to light. In this research, self-adhesive electrodes were used, which differs from other studies that conducted the procedure with needle electrodes.
In studies described in literature with 33 participants, with 12 weeks of treatment and after an intervention in 6 and 12 months of treatment, it was verified a sustained improvement of 12 weeks to 6 months for 94% of participants, and 12 months for 96% of the study subjects, not any serious adverse event occurred after the period of one year of treatment33.
In the quality of life questionnaire applied during the study, statistically significant difference was not observed in any of the scores of the nine fields, before and after treatment, as shown in Table 2.
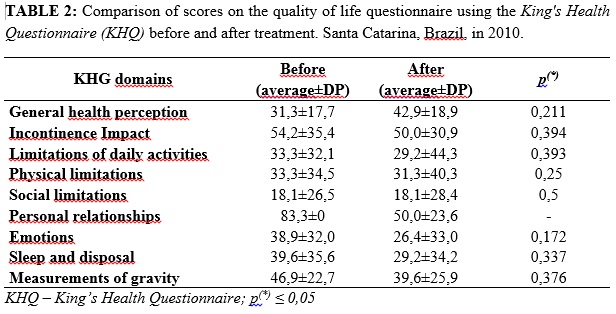
The domain of social limitations did not change after treatment, and in other domains such as, personal relationships, emotions, sleep, mood and gravity measures, there was no significant improvement after treatment. On those results, in a study was observed that as it favors the maintenance of social conviviality, it improves the quality of life of the people, which was not observed in this study34.
In other research with the same questionnaire of this study, in relation to scores of KHQ questionnaire, it was observed that only the general perception domain of health showed no significant variation after application of electrical stimulation. In other domains, there was a significant improvement in the value of scores35. On the other hand, another study showed improvement in the domains of physical limitation and sleep, and in the other domains of the questionnaire KHQ was not observed changes after treatment36.
The impact of UI on the lives of men and women includes adverse effects on social, professional activities, leisure, sexual health and relationships with family members. The results obtained in other studies indicate that the UI impact is greatest for physical health than for mental health21.37. Despite UI being a frequent complaint in women, many end up not reporting to their doctors, hindering the search for specialized services. In this way, adherence to a conservative treatment ends up being low, which limits research and the conservative treatment require a longer time to present the first results and realize more effectively control the incontinence22.
CONCLUSION
Deve-se ressaltar, no entanto, que estes resultados foram obtidos com um universo amostral relativamente pequeno, sendo necessário novos estudos sobre o uso da eletroestimulação no nervo tibial posterior, bem como verificar o tempo de permanência destes resultados.
Treatment with posterior tibial nerve electrical stimulation produced a positive result in the daytime and nighttime voiding frequency, and also to involuntary loss of study participants. Regarding to the quality of life questionnaire, positive changes were obtained, but not statistically significant.
This type of treatment proposed for incontinent patients is feasible, as conservative treatment of urinary incontinence, due to their low cost and the absence of side effects.
It should be emphasized, however, that these results were obtained with a relatively small sampling universe, requiring new studies about the use of electrical stimulation in the posterior tibial nerve, as well as check the length of stay of these results.
REFERENCES
1.Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA) / International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010; 21: 5-26.
2.Felderner Jr PC, Sartori MGFS, Lima GR, Baracat EC, Girão MJBC. Diagnóstico clínico e subsidiário da incontinência urinária. Rev Bras Ginecol Obstet. 2006; 28:54-62.
3. Fujihara A, Ukimura O, Hongo H, Iwata T, Veda T, Matsugasumi T, et al. Urge perception indexo of bladder hypersensitivity. J Urol. 2013; 189:1797-03.
4.Dwyer PL. Differentiating stress urinary incontinence from urge urinary incontinence. Int J Gynecol Obstet. 2004; 86:17-24.
5.Klingler HC, Schmidbauer J, Maeberger M. Use of peripheral neuromodulation of S3 region for treatment of detrusor overactivity: a urodynamic – based study. Urology. 2000; 56:766-71.
6.Arruda RM, Souza GO, Castro RA, Sartoria MGF, Baracat EC, Girões MJBC. Hiperatividade do detrusor: comparação entre oxibutinina, eletroestimulação funcional do assoalho pélvico e exercícios perineais. Estudo randomizado. Rev Bras Ginecol Obstet. 2007; 29:452-8.
7.Brown JS, McNaughton KS, Wyman JF, Burgio KL, Harkaway R, Bergner D, et al. Measurement characteristics of a voiding diary for use by men and women with overactive bladder. Urology. 2003; 61:802-9.
8.Fonseca ESM, Camargo ALM, Castro RA, Sartori MGFS, Fonseca MCM, Lima GR, et al. Validação do questionário de qualidade de vida (King’s Health Questionnaire) em mulheres brasileiras com incontinência urinária. Rev Bras Ginecol Obstet. 2005; 27:235-42.
9.Rett MT, Simões JA, Herrmann V, Gurgel MSC, Moraes SS. Qualidade de vida em mulheres após tratamento da incontinência urinária de esforço com fisioterapia. Rev Bras Ginecol Obstet. 2007; 29:134-40.
10.Tamanini JTN, D’Ancona CAL, Botega NJ, Rodrigues Netto Jr N. Validação do King’s Health Questionnaire para o português em mulheres com incontinência urinária. Rev Saude Publica. 2003; 37:203-11.
11.Amarenco G, Ismael SS, Even-Schneider A, Raibaut P, Demaille-Wlodyka S, Parratte B, et al. Urodynamic effect of acute transcutaneous posterior tibial nerve stimulation in overactive bladder. J Urol. 2003; 169:2210-5.
12.Vandoninck V, Van Balken MR, Agro EF, Petta F, Caltagirone C, Heesakkers JPFA, et al. Posterior tibial nerve stimulation in the treatment of urge incontinence. Neurourol Urodyn. 2003; 22:17-23.
13.Vandoninck V, Van Balken MR, Agro EF, Heesakkers JPFA, Debruyne FMJ, Kiemeney LALM, et al. Posterior tibial nerve stimulation in the treatment of voiding dysfunction: urodynamic data. Neurourol Urodyn. 2004; 23:246-51.
14.Van Balken MR, Vergunst H, Bemelmans BLH. The use electrical devices for the treatment of bladder dysfunction: a review of methods. J Urol. 2004; 172:846-51.
15.Franco MM, Souza FO, Vasconcelos ECLM, Freitas MMS, Ferreira CHJ. Avaliação da qualidade de vida e da perda urinária de mulheres com bexiga hiperativa tratadas com eletroestimulação transvaginal ou do nervo tibial. Fisioter Pesq. 2011; 18:145-50.
16.Booth J, Hagen S, McClurg D, Norton C, MacInnes C, Collins B, et al. A feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care. Am J Med Assoc Dir. 2013; 14:270-4.
17.Moossdorff-Steinhauser HFA, Berghmans B. Effects of percutaneous tibial nerve stimulation on adult patients with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2013; 32:206-14.
18.Van Der Pal F, Van Balken MR, Heesakkers JPFA, Debruyne FMJ, Kiemeney LALM, Bemelmans BLH. Correlation between quality of life and voiding variables in patients treated with percutaneous tibial nerve stimulation. BJU International. 2006; 97:113-6.
19.Brown JS, Bradley CS, Subak LL, Richter HE, Kraus SR, Brubaker L, et al. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med. 2006; 144:715-23.
20.Marchal C, Herrera B, Antuña F, Saez F, Perez J, Castilho E, et al. Percutaneous tibial nerve stimulation in treatment of overactive bladder: when should retreatment be started? Urology. 2011; 78:1046-50.
21.Wyman JF, Burgio KL, Newman DK. Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. Int J Clin Pract. 2009; 63:1177–91.
22.Honório MO, Santos SMA. A rede de apoio ao paciente incontinente: a busca por suporte e tratamentos. Rev enferm UERJ. 2010; 18:383-8.
23.Matheus LM, Mazzari CF, Mesquita RA, Oliveira J. Influência dos exercícios perineais e dos cones vaginais, associados à correção postural, no tratamento da incontinência urinária feminina. Rev Bras Fisioter. 2006; 10:387-92.
24.Guarisi T, Net AMP, Osis MJ, Pedro AO, Paiva LHC, Faúndes A. Incontinência urinária entre mulheres climatéricas brasileiras: inquérito domiciliar. Rev Saude Publica. 2001; 35:428-35.
25.Moller LA, Lose G, Jorgensen T. Risk factors for lower urinary tract symptoms in women 40 to 60 years of age. Obstet Gynecol. 2000; 96:446-51.
26.Higa R, Lopes MHBM, Reis MJ. Fatores de risco para a incontinência urinária na mulher. Rev Esc Enferm. 2008; 42:187-92.
27.Fenner DE, Genberg B, Brahma P, Marek L, Delancey JOL. Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am J Obstet Gynecol. 2003; 189:1543-50.
28.Riesco MLG, Costa ASC, Almeida SFS, Basile ALO, Oliveira SMJV. Episiotomia, laceração e integridade perineal em partos normais: análise de fatores associados. Rev enferm UERJ. 2011; 19:77-83.
29.Silva, NLS, Oliveira SMJV, Silva FMB, Santos JO. Dispareunia, dor perineal e cicatrização após episiotomia. Rev enferm UERJ. 2013; 21:216-20.
30.Van Balken MR, Vergunst H, Bemelmans BLH. Prognostic factors for successful percutaneous tibial nerve stimulation. Eur Urol. 2006; 49:360-5.
31.Bellette PO, Rodrigues-Palma PC, Hermann V, Riccetto C, Bigozzi M, Olivares JM. Posterior tibial nerve stimulation in the management of overactive bladder: a prospective and controlled study. Actas Urol Esp. 2009; 33:58-63.
32.De Gennaro M, Capitanucci ML, Mastracci P, Silveri M, Gatti C, Mosiello G. Percutaneous tibial nerve neuromodulation is well tolerated in children and effective for treating refractory vesical dysfunction. J Urol. 2004; 171:1911-3.
33.MacDiarmid SA, Peters KM, Shobeiri SA, Wooldridge LS, Rovner ES, Leong FC, et al. Long-term durability of percutaneous tibial nerve stimulation for the treatment of overactive bladder. J Urol. 2010; 183:234-40.
34.Moliterno ACM, Faller JW, Borghi AC, Marcon SS, Carreira L. Viver em família e qualidade de vida de idosos da universidade aberta da terceira idade. Rev enferm UERJ. 2012; 20:179-84.
35.Fischer-Sgrott FO, Manffra EF, Busato Junior WFS. Qualidade de vida de mulheres com bexiga hiperativa refratária tratadas com estimulação elétrica do nervo tibial posterior. Rev Bras Fisioter. 2009; 13:480-6.
36. Onal M, Ugurlucan FG, Yalcin O. The effects of posterior tibial nerve stimulation on refractory overactive bladder syndrome and bladder circulation. Arch Gynecol Obstet. 2012; 286:1453-7.
37.Paick JS, Kim SW, Oh SJ, Ku JH. A generic health-related quality of life instrument, the medical outcomes study short form-36, in women with urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2007; 130:18-24.