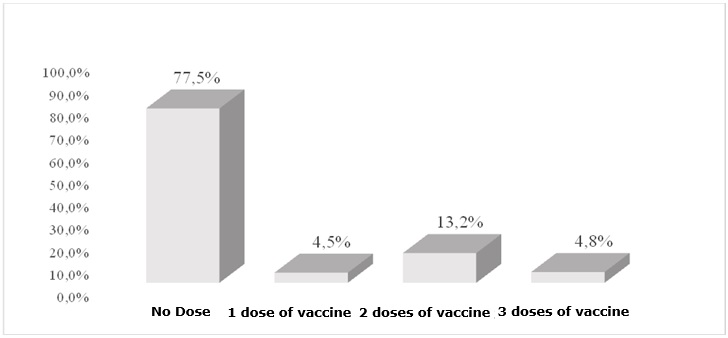
FIGURE 1 : Percentage distribution of postpartum women according to vaccination status against hepatitis B. Teresina - PI, 2011.
RESEARCH ARTICLES
Hepatitis B serologic and vaccination status in postpartum women at a public maternity hospital
Verbênia Cipriano FeitosaI; Telma Maria Evangelista de AraújoII; Inez Sampaio NeryIII; Silvana Santiago da RochaIV
I
Master in Nursing. Federal University of Piaui. Teresina, Piaui, Brazil. E-mail: verbeniafeitosa@gmail.com
II
PhD in Nursing. Federal University of Rio de Janeiro. Anna Nery Nursing School. Professor of the Postgraduate Program Master in Nursing. Federal University
of Piaui. Teresina, Piaui, Brazil. E-mail: telmaevangelista@gmail.com
III
PhD in Nursing. Federal University of Rio de Janeiro. Anna Nery Nursing School. Professor of the Postgraduate Program Master in Nursing. Federal University
of Piaui. Teresina, Piaui, Brazil. E-mail: ineznery.ufpi@gmail.com
IV
PhD in Nursing. Federal University of Rio de Janeiro. Anna Nery Nursing School. Professor of the Postgraduate Program Master in Nursing. Federal University
of Piaui. Teresina, Piaui, Brazil. E-mail: silvanasantiago27@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.6481
ABSTRACT
Hepatitis B is a viral infection notable for high rates of morbidity, chronicity, cirrhosis and hepatocellular carcinoma (HCC). This transversal study to evaluate serologic and Hepatitis B vaccination status in women admitted to a public maternity hospital in Teresina was conducted in January and February, 2011, through interviews of a sample of 377 postpartum women. Poor vaccine coverage was characterized by missed opportunities for immunization: 77.5% of the sample received no dose of the vaccine, even though most had received antenatal care. Hepatitis serology testing had been performed on only 41.9%. However, 77.1% were informed of what vaccines they should receive during the antenatal period. Nurses were the information source most mentioned (by 55%), underlining their key role as health educators in antenatal care. The study found low vaccine and serological coverage, evidencing the inefficiency of antenatal monitoring.
Keywords: Immunization coverage; serology, hepatitis B; puerperium.
INTRODUCTION
Hepatitis B is an infectious disease of viral origin, considered today a major public health problem in Brazil and worldwide. Often, hepatitis B virus carriers do not know they have this condition, which has contributed to the significant increase in the occurrence of vertical transmission, as appropriate steps with the newborn (NB) at birth are not always taken in account.
Development of the vaccine against hepatitis B was one of the greatest scientific achievements of the last three decades. However, morbidity and mortality persists, and it stands out as one of the leading causes of liver disease, associated, in its chronic form, with cirrhosis and hepatocellular carcinoma (HCC). Furthermore, the number of individuals infected with hepatitis B virus (HBV) is about 10 times higher than those with Human Immunodeficiency Virus (HIV)1.
The World Health Organization (WHO) estimates that more than 350 million people are infected worldwide and 200,000 new cases are detected each year in the United States. Of these, only 33-50% are symptomatic. About 5%, or 12.5 million people, were infected, and 10% of them had chronic infection2.
In Brazil, the situation is also worrying. According to the Ministry of Health (MOH), it is estimated that 15% of the population have been exposed to HBV, and 1% of these suffer from chronic hepatitis B. A study carried out before the vaccination policy against hepatitis B virus pointed three virus distribution patterns in Brazil: highly endemic in the Amazon region, part of Espirito Santo State and west of Santa Catarina State; intermediate endemicity, in the Northeast, Midwest and Southeast regions and low endemicity in Southern Brazil. However, after the introduction of the vaccine, this pattern has been changing in all regions of the country. Therefore, the Northeast region was currently considered in low endemic situation3.
The low endemicity in the Northeast region, especially in Piaui, could be related to the low number of notifications, which compromises a real diagnosis of hepatitis B situation in this region. Piaui had, in 2004, 777 confirmed cases of viral hepatitis, being the seventh state in the Northeast in numbers of cases. The etiology of 25% of these cases was indefinite, demonstrating that the surveillance and diagnosis needed to be increased. At that same year, mortality rates for hepatitis B and C in Piaui were lower than the regional and national average. In 2008, 792 cases of viral hepatitis were registered in the Notifiable Diseases Information System (SINAN) of Piaui, and, in 2009, there was a reduction in the number of notifications to 335, and among the confirmed cases, 102 were positive for hepatitis B4. However, a study conducted from 2007 to 2010 found that Piaui presented 746 confirmed cases of acute hepatitis B5. So, the authors of this study questioned the information contained in the SINAN of the Piaui State, in relation to hepatitis B.
Statistics show the importance of adopting strategies for preventing and controlling the spread of HBV. One of the statistics concerns the early initiation of prenatal care, at which serology should be performed. In face of detection of infection, therapeutic measures must be instituted, as well as prophylaxis for the transmission of the infection. In pregnant women, a preventive measure is the request of serologic testing for hepatitis B in the first three months and at 32 weeks of pregnancy and vaccination against hepatitis B in pregnant women at any time in pregnancy6,7.
Vaccination should be a practice incorporated into the daily life of health facilities, and should, therefore, cease to be unique to primary care services to be incorporated in other types of service, for example, maternity wards, so as not to miss any opportunity of vaccination. For hepatitis B to remain under control, it is required a minimum vaccination coverage of 95%8,4.
According to the Piaui State Coordination of Immunization, vaccination coverage of hepatitis B accumulated from 1994 to September 2011 in children under one year old was 95.8%; in children aged 5 to 10 years old, it reached 104.5%; in other age groups, it did not reach the minimum recommended by the National Immunization Program (PNI, in Portuguese). The coverage reached 78.3% of children aged 11 to 14 years old, 44.5% for children aged from 15 to 19 years old and only 30.3% for the age group between 20 to 24 years old9. The low vaccination coverage for hepatitis B in young ones, among these women of child-bearing age, sets a worrying situation in preventing infection at this stage of life. Based on these, this study aimed to evaluate the serological and immunization status for hepatitis B in postpartum women at a public maternity hospital in Teresina.
LITERATURE REVIEW
Hepatitis B is still one of the main causes of liver disease worldwide. It is estimated that around one million people die from complications of liver disease every year. Chronic hepatitis B has proved a complex disease, difficult to deal, due to peculiarities in virus-host relationship, the appearance of mutants, viral heterogeneity and diversity of clinical forms10.
In Brazil, the hepatitis B vaccine was introduced in 1998 when the PNI recommended the universal vaccination of children in the first year of life, since birth. In 2001 the age was increased to 19 years old. Later, in 2009, it was extended to the entire national territory for groups considered most vulnerable, such as pregnant women, health workers, firefighters, police officers, among others. In 2011, it was extended to the age of 24; in 2012, it was extended to 29 years old11. In 2013, it has been further extended, from 30 to 49 years old12.
Currently, PNI offers the hepatitis B vaccine to all the vaccination room of the country. The vaccination schedule for children consists of four doses, with the first (monovalent) given at birth, the second (pentavalent) at two months of age, the third and fourth at four to six months of age13. Each dose is of 0.5 ml in individuals under 20 years old, and of 1ml in individuals over 20 years old, intramuscularly. It should not be made in the buttocks due to the greater amount of adipose tissue, rather, the vastus side thigh in infants and the deltoid muscle in adults are indicated. There is no specific contraindications11.
It is observed that, in Brazil, access to the vaccine and expansion of its offer covered a large portion of the population. However, it is necessary to raise awareness of both the community and the professionals that the elimination of HBV transmission is only possible if really these measures are put in practice in the daily routine of health services and if the population, who is the main beneficiary, do enforce their rights to health, fulfilling their role as a citizen.
METHODOLOGY
It is an epidemiological, cross-sectional and documentary study, conducted by evaluating the prenatal card records, considering the variables related to the hepatitis B vaccine doses. The study population consisted of postpartum women admitted to a public maternity of Teresina, by using random sampling, based on the monthly average of deliveries (n = 950) and a tolerable error of 4% (n = 377). It was adopted as exclusion criteria being without clinical condition to answer questions of interest to the study. Only three were excluded, resulting in 374 women. Data collection occurred from January to February 2011, through interviews and evaluation of prenatal records of each postpartum woman. The instrument was a form containing the following variables: gestational age at first prenatal care visit, location of prenatal care, number of received doses of hepatitis B vaccine, performance of serologic testing for hepatitis B, information of mothers on vaccines and informant source.
Data were entered using the Statistical Package for the Social Sciences (SPSS) software. To seek the association of serology and vaccination for hepatitis B with sociodemographic and perinatal aspects of mothers, the chi-square test was used with the respective value of p and odds ratio.
The Informed Consent Form was offered to mothers to inform them about the risks and benefits, as required by Resolution No. 196/9614. The study was approved by the Research Ethics Committee of the Federal University of Piaui (Certificate of Presentation for Ethical Consideration No. 0281.0.045.000-10).
RESULTS AND DISCUSSION
Of the 374 mothers surveyed, three did not received prenatal care. Adherence to the first consultation was (100%). About professionals who provided prenatal care, 120 (32.09%) women were attended exclusively by nurses, 141 (37.70%) by the doctor and 113 (30.21%) had consultations with doctor and nurses, i.e., the nurse was the nuclear professional in attendance.
This was in agreement with a recommendation of the Ministry of health6, which states that the prenatal and postpartum visits can be performed by doctors or nurses or even be alternated between them. It is noteworthy that, according to the law for professional practice of nursing No. 7498/86 15 and Decree No. 94,406 / 8716, low risk prenatal care can be fully monitored by nurses.
Other studies17 found sufficient data to state that women approve prenatal care performed by nurses, because they say that these professionals serve more calmly, without haste to leave, and provide information with an easier and more comprehensive language for them.
Only 18 (4.8%) mothers received the three doses required for adequate vaccination coverage. The low immunization coverage was characterized by missed opportunities for immunization (MOI), for 289 (77.5%) of them have not received any dose of the vaccine, although most have done the complete pre-natal care, as shown in Figure 1.
FIGURE 1
: Percentage distribution of postpartum women according to vaccination status against hepatitis B. Teresina - PI, 2011.
Studies have shown that the neglect of professionals to observe users' vaccination card, among other negative attitudes, has constituted one of the main causes of MOI and hence contributed to the low vaccination coverage8,18. In the case of pregnant women, the situation is more critical, because the prenatal consultation takes place systematically and interchangeably by the doctor and nurse, which should be a protective factor not to occur MOI. Besides these professionals, the mother is also served by the technical nursing and the community health worker, every time they attend the health unit for the realization of prenatal care.
The use of hepatitis B vaccine in the prenatal care routine is still being used rarely, mainly due to the lack of knowledge of professionals about the associated benefits.
In 2009, the PNI has reinforced the indication of vaccination against hepatitis B in pregnant women who have had negative testing for Hepatitis B Surface Antigen (HBsAg) and those who have lost the opportunity to receive the vaccine in the routine of services. Pregnancy does not contraindicate vaccination; it can be performed at any gestational age11.
The prenatal consultation is an opportune time to do the tracking of HBV infection in order to prevent vertical transmission of infection. In this study, only 155 (41.4%) of the women had had serum testing for hepatitis B. Among those who had performed it, 99.1% showed negative result and 0.9% showed positive result. These data are in line with a study of serological markers of hepatitis B in pregnant women, conducted in Vitoria – ES and in northwest Para, which had rates of 0.9% and 0.5% of positivity19,20, respectively.
Although the prevalence of positivity for hepatitis B was low among the women in this study and in other regions of Brazil, it is important to note that most of them did not perform the specific serology for infection at the time of prenatal care. And adding this to MOI of these pregnant women in prenatal care, there is risk of exposure to infection for their newborns, and consequently of chronicity of the disease21.
Thus, the search for quality of prenatal care requires basic examinations, among there the serology for hepatitis B. And, in this study, there was a statistically significant association in relation to the request of serology for hepatitis B with some prenatal variables, i.e., women who began prenatal care at a gestational age above 14 weeks (OR = 1.54, p <0.01 and CI 1.01 to 2.35) and who did it incompletely (OR = 1.92, p <0.01 and CI 1.23 to 3.01) had a higher chance of not performing serology for HBsAg. And those who underwent prenatal care in a country town of Piaui (OR = 3.27, p <0.01 and CI 2.13 to 5.04) were three times more likely not to perform this examination. It is known that a prenatal care performed in places with inadequate infrastructure will have greater difficulty in maintaining the provision of basic tests. However, a study conducted in a school maternity in the municipality of Rio de Janeiro revealed that almost half of the mothers did not undergo screening for hepatitis B in the prenatal care and most also did not receive information about this test22. Therefore, the low coverage of the serological test for hepatitis B permeates different scenarios of assistance to pregnant women in Brazil, according to Table 1.
TABLE 1:
Simple logistic regression model of performance of HBsAg survey with variables related to prenatal care of mothers of the study. Teresina - PI, 2011
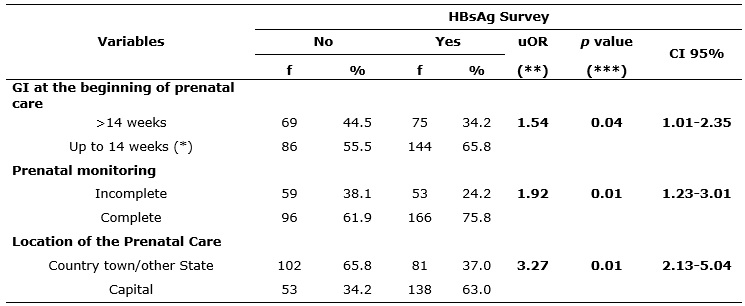
(*)Reference category; uOR = Unadjusted odds ratio (**); CI - confidence interval;
p
value obtained by Chi-square test (***)
Regarding information about the vaccine against hepatitis B, 289 (77.3%) of the mothers were informed about the vaccines that should be given during the prenatal period. Among the informants, nurses were the most cited sources, 159 (55.0%), strengthening their leading role as a health educators in prenatal care.
TABLE 2:
Distribution of postpartum women according to reception information on vaccines in prenatal care and professional who inform them. Teresina-PI, 2011
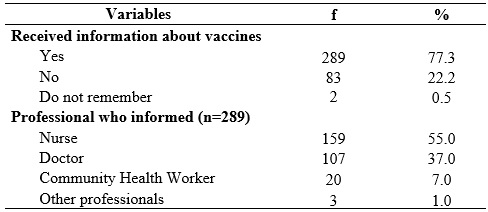
It is observed that women felt free to seek information with the nurse, because usually this professional provides a more comprehensive care during the prenatal care, including health education. The counterpoint was the community health worker, whose primary function is the health education. It was observed the gap left by them in relation to the guidance for vaccination.
Women establish greater trust with the nurse, which makes it easy to ask something they do not understand17. However, the mere reception of information does not guarantee that these will be well assimilated by the group. This underscores the relevance of the nurse to reflect on their position in educational activities, to value the active participation of pregnant women in education and health groups22,23. To this end, it is needed a professional interaction between the pregnant woman and the professional, to develop their confidence, enhance credibility and thus promote a relationship of knowledge exchanges. From this perspective, it is important to consider the nursing consultation as an important space for conducting educational activities24 and call attention to the quality of care, especially by the nurse, who is responsible for hosting in the service's gateway.
The inadequate quality of information filled on the prenatal record card is considered a limitation of the study, but not enough to harm it, since the vaccination status of mothers was raised by his annotation. Thus, they may have received vaccines that were not recorded.
CONCLUSION
The results of this study showed that most mothers had had at least one prenatal consultation. However, it was found low serological and immunization coverage for hepatitis B, pointing out the need for sensitization of all health professionals involved in prenatal care, to get involved on the importance of vaccination, as it is unjustifiable that woman attend the consultation and are not vaccinated at this time.
There are many challenges to equate this problem, which include welfare, social and individual aspects. So, to face them, the actions should be expanded to beyond the health services, with the adoption of a not merely biological approach, but an approach that includes women in their fullness.
It is noteworthy that the nurse, who is the professional inserted in all levels of care for women and children, can and should collaborate in overcoming these challenges. And due to their effective role in prevention and health promotion, they can contribute, individually, in nursing consultations, held at the Family Health Strategy, in home visits, and in activities developed in maternities and childbirth centers, to improve vaccination coverage to users.
Thus, there must be a reflection on how health professionals, managers of health services and the wider community can contribute to the improvement of vaccination coverage and to the request of the serological test for hepatitis B. The community was cited in this triad because authors believe that immunization targets can only be reached if there is a joint effort of society as a whole.
REFERENCES
1.Santos NOS, Romanos MTV, Wigg MD. Introdução à virologia Humana. 2ª ed. Rio de Janeiro: Guanabara Koogan; 2008.
2.Focaccia R, Veronesi R. Tratado de Infectologia. São Paulo: Atheneu; 2009
3.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para o tratamento da hepatite viral crônica B e confecções. Brasília (DF): Ministério da Saúde; 2010.
4.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Sistema nacional de vigilância em saúde: relatório de situação: Piauí. 5ª ed. Brasília (DF): Ministério da Saúde; 2011
5.Araújo TME, Sá LC, Santos AS, Faustino SKM, Tapety FI. Prevalência da hepatite B em usuários do laboratório Central do Piauí. Rev enferm UERJ [Internet]. 2012 [citado em 30 mai 2013]. 20; 229-34. Disponível em: http://www.facenf.uerj.br/v20n2/v20n2a15.pdf
6.Ministério da Saúde (Br). Secretaria de Atenção à Saúde: Departamento de Ações Programáticas Estratégicas: Área Técnica de Saúde da Mulher. Pré-natal e Puerpério: atenção qualificada e humanizada – manual técnico. Brasília (DF): Ministério da Saúde; 2006
7.Hinrichsen SL. DIP. Doenças infecciosas e parasitarias. Rio de Janeiro: Guanabara Koogan; 2005
8.Araújo TME. Vacinação Infantil: conhecimentos, atitudes e práticas da população da Área Norte/Centro de Teresina/PI. [Tese Doutorado]. Rio de Janeiro: Universidade Federal do Rio de Janeiro, Escola de Enfermagem Anna Nery, 2005.
9.Secretaria Estadual da Saúde do Piauí (Sesapi). Coordenação Estadual de Imunização. Série Histórica de vacinação da Hepatite B. Teresina (PI); 2011.
10.Ferreira CT, Silveira TR. Hepatites virais: aspectos da epidemiologia e da prevenção. Rev Bras Epidemiol. [Scielo-Scientific Electronic Library Online] 2006 [citado em 18 maio 2013]. 7:473-87
11.Medeiros, SLC. Soroprevalência da infecção pelo vírus da Hepatite B em usuários de crack no Piauí. [Dissertação de Mestrado]. Teresina: Universidade Federal do Piauí, 2013.
12.Ministério da Saúde (Br). Nota técnica conjunta nº 02/2013 CGPNI/DEVEP e CGDHRV/DST-AIDS/SVS/MS. Ampliação da oferta da vacina hepatite B para a faixa etária de 30 a 49 anos em 2013. Brasília (DF), 2013.
13.Ministério da Saúde (Br). Informe técnico da introdução da vacina pentavalente. CGPNI/DEVEP/SVS/MS. Brasília (DF), 2012.
14.Ministério da Saúde (Br). Conselho Nacional de Saúde – CNS. Diretrizes e Normas Regulamentadoras de Pesquisas Envolvendo Seres Humanos. Resolução nº 196/96. Brasília (DF): Ministério da Saúde; 1996.
15.Brasil. Presidência da República, Lei nº 7498, de 25 de junho de 1986. Dispõe sobre a regulamentação do exercício da enfermagem, e dá outras providências [Internet]. Brasília (DF); 1986. [citado em 30 mai 2013]. Disponível em: http://www.jusbrasil.com.br/ legislação/128195/lei-7498-86
16.Conselho Federal de Enfermagem. Decreto nº 94.406, de 08 de junho de 1987. Regulamenta a lei nº 7.498 e da outras providencias. [Internet]. Brasília (DF); 1987. [citado em 30 mai 2013]. Disponível em: http://www.cofen.gov.br/decreto-n-9440687_4173.html
17.Shimizu HE, Lima MG. As dimensões do cuidado pré-natal na consulta de enfermagem. Rev Bras de Enferm. [internet] 2009 [citado em 18 mai 2013]. 62; 387-92. Disponível em: http://www.scielo.br/scielo.php?pid=S0034-71672009000300009&script=sci_arttext
18.Organização Pan-americana da Saúde. Oportunidade Perdida de Vacinação. Brasília (DF): OPS;1985
19.Figueiredo NC, Page-Shafer K, Pereira F E L, Miranda A E . Marcadores sorológicos do vírus da hepatite B em mulheres jovens atendidas pelo Programa de Saúde da Família em Vitória, Estado do Espírito Santo, 2006.Revista da Sociedade Brasileira de Medicina Tropical [Scielo-Scientific Electronic Library Online] 2005 [citado em 05 set 2013]. 58: 590-5. Disponível em: http://www.scielo.br/prc
20.Ferezin RI, Bertolini DA, Demarchi IG. Prevalência de sorologia positiva para HIV, hepatite B, toxoplasmose e rubéola em gestantes do noroeste paranaense. Rev Bras Ginecol Obstet. [Scielo-Scientific Electronic Library Online] 2013 [citado em 28 mai 2015]; 35:66-70.Disponível em: http://www.scielo.br/prc
21.Piazza MJ, Urbanetz AA, Carvalho NS, Nascimento DJ. Hepatites virais e gestação. Diagn Tratamento. 2010;15(1):12-8. Disponível em: http://files.bvs.br/upload/S/1413-9979/2010/v15n1/RDTv15n1a1054.pdf
22.Silva CF, Araújo CLF, Araújo MM. Oferta do teste sorológico para Hepatite B durante o pré-natal: a vivência das puérperas. Rev enferm UERJ. 2015; 23:58-63. Disponivel: http://www.facenf.uerj.br/v23n1/v23n1a10.pdf
23.Pereira SVM, Bachion MM. Diagnósticos de Enfermagem identificados em gestantes durante o pré-natal. Rev Bras Enferm. [Scielo-Scientific Electronic Library Online] 2005 [citado em 18 mai 2013]. 58:559-64. Disponível em: http://www.scielo.br/prc
24.Rios CTR, Vieira NFC. Ações educativas no pré-natal: reflexão sobre a consulta de enfermagem como um espaço para educação em saúde. Ciênc saúde coletiva. [Scielo-Scientific Electronic Library Online] 2007 [citado em 18 mai 2013]. 12: 477-86. Disponível em: http://www.scielo.br/prc