RESEARCH ARTICLES
Comparison of the knowledge of postpartum women regarding breastfeeding
Mariana de Oliveira Fonseca-MachadoI;
Marina Stark Rezende de PaulaII; Bibiane Dias Miranda ParreiraIII; Juliana StefanelloIV;
Flávia Gomes-SponholzV
I RN. Master’s Degree. University of São Paulo. School of Nursing of Ribeirão Preto. Nursing Graduate Program in Public Health. Ribeirão Preto, São Paulo, Brazil. E-mail: mafonseca.machado@gmail.com
II RN. Universidade Federal do Triângulo Mineiro. Nursing Undergraduate Program. Department of Nursing in Community Health Education. Uberaba, Minas Gerais, Brazil. E-mail: ninastark@terra.com.br
III RN. Master’s Degree. Universidade Federal do Triângulo Mineiro. Nursing Undergraduate Program. Department of Nursing in Community Health Education. Uberaba, Minas Gerais, Brazil. E-mail: bibianedias@yahoo.com.br
IV RN. Ph.D. University of São Paulo. School of Nursing of Ribeirão Preto. Department of Mother-Child Nursing and Public Health. Ribeirão Preto, São Paulo, Brazil. E-mail: julianas@eerp.usp.br
V RN. Ph.D. Lecturer. University of São Paulo. School of Nursing of Ribeirão Preto. Department of Mother-Child Nursing and Public Health. Ribeirão Preto, São Paulo, Brazil. E-mail: flagomes@eerp.usp.br
ABSTRACT
The purpose of this study was to compare the knowledge of postpartum women regarding breastfeeding according to sociodemographic, obstetric and personal aspects. This observational cross-sectional study was developed in the rooming-in of a university hospital in Uberaba, Minas Gerais, with 141 women, between July and August of 2010. Data were collected by means of interviews with a validated instrument. Data were analyzed using the univariate analysis, Student’s t-Test for differences between means and Pearson’s correlation analysis. The knowledge regarding breastfeeding was higher in the group of women with nine or more years of education, who attended six or more prenatal visits and received guidance on breastfeeding during pregnancy (p <0.05). Identifying the characteristics of women with greater knowledge on breastfeeding allows to propose educational programs and reorganize health services for the implementation of specific and targeted actions.
Keywords: Breastfeeding; knowledge; women; postpartum period.
INTRODUCTION
Breastfeeding is a safe source of nutrition for human beings in the initial phase of life. Its benefits have been well documented in the scientific literature and efforts to promote this practice are being implemented in several countries1.
The World Health Organization (WHO) advises that human milk must be the only food in the first six months of life of a child and, after this period, it may be complemented with other food, nutritionally appropriate, until the child is two years or older. Despite this recommendation, national studies revealed that, in 2008, the median duration of exclusive breastfeeding (EB) in Brazil was 54.1 days, whereas the duration of complemented breastfeeding was 11.2 months2.
The choice to breastfeed is something complex and involves the knowledge of women regarding this practice, which is permeated with biomedical and cultural concepts, values, beliefs, previous experiences and the interference of family members, community and health professionals3.
The identification of the knowledge of pregnant women and nursing mothers regarding breastfeeding and its determinants allows health professionals to make a new approach of breastfeeding, by entering the multidimensional complex that permeates this practice4. In addition, it contributes to reduce child morbimortality rates, as it interferes in the prevalence and duration of breastfeeding5,6.
Over the last ten years, national5,7-13 and international studies14-16 have analyzed the knowledge of postpartum women regarding breastfeeding. These studies focused mainly on the description of this knowledge and its relationship with variables such as age, education, guidance, experience in breastfeeding, development of a family plan and number of prenatal visits.
However, the knowledge approached in studies developed in Brazil is restricted to punctual and specific questions in breastfeeding8,9,13, leading to a gap in the national scientific production as for the identification of variables related with a knowledge that broadly comprises theoretical and practical aspects of breastfeeding.
In order to study this issue directly, the present study aimed to compare the knowledge of postpartum women regarding breastfeeding according to sociodemographic, obstetric and personal aspects.
THEORETICAL FRAMEWORK
Health promotion is a promising strategy to face health problems affecting individuals and their environment, as well as to achieve better life conditions in general. Its feasibility is granted by public policies, favorable conditions to the development of health and the reinforcement of the capability of individuals and communities. It is based on a broad concept of the health-disease process and its determinants, and proposes the articulation of technical and popular knowledge, reflecting a reaction to the growing medicalization of social life17.
Feeding and nutrition constitute basic requisites for the promotion of health, stating broadly the human potential for growth and development, with quality of life and citizenship. One of the most important occurrences in the Brazilian setting of feeding and nutrition is the continuing dissatisfactory breastfeeding rates, despite the increase observed over the last decades18.
Breastfeeding and, consequently, the knowledge of women regarding this practice, are developed within a sociocultural context. Actions in favor of breastfeeding, either individually or collectively, must take into consideration the combination of nature and culture that comprises this practice19.
In this sense, the identification of the knowledge of postpartum women regarding breastfeeding and its relation with sociodemographic, obstetric and personal aspects may be considered an action for breastfeeding promotion. From this point, other strategies such as public policies; programs; activities; the creation of favorable environments; qualification and information for mothers, parents, family members and communities; and the development of individual skills and pro-breastfeeding attitudes may be promoted, contributing to increase the prevalence and duration of breastfeeding in Brazil.
The promotion of breastfeeding aims to create cultural behaviors and values favorable to this practice, so that it may be assumed as a rule, which depends on national public policies and the recommendations of social and health services20.
METHODOLOGY
This observational cross-sectional study was developed in the rooming-in of a university hospital in the municipality of Uberaba, Minas Gerais, Brazil.
Uberaba is located in the macroregion of Triângulo Mineiro and Alto Paranaíba, and it is the hub city of the health micro and macroregion of Triângulo Sul, comprising 21 municipalities.
The study sample comprised all postpartum women who were hospitalized in this rooming-in, between July and August of 2010, and accepted to participate in the study by signing the Free and Informed Consent Form (FICF). Minors were accompanied by an adult responsible for them, who approved their participation and signed the FICF. The final population totaled 141 women.
Data were collected by means of interview in the first 24 after the delivery, in a calm place and when the women presented appropriate physical and psychological conditions. After data collection, the difficulties and questions of the participants were clarified.
The public domain instrument used was previously tested and validated21, and comprised questions regarding the sociodemographic (age, education, marital status, occupation) and obstetric profile (parity) of the participants; the characteristics of the prenatal care received (number of prenatal visits, guidance on breastfeeding) and their personal experience in breastfeeding (time they breastfed previous children); and the identification of the women’s knowledge regarding breastfeeding.
In order to identify this knowledge, a test with ten true or false questions was used, contemplating the following aspects: self-care with their breasts, conduction of the feeds, ideal moment for the first feed, duration of EB and complemented breastfeeding, milk production, control of lactation and mammary complications. Each correct answer scored one point, so the maximum score was ten. Incorrect answers scored zero.
The variable answer considered was the mean of correct answers in the knowledge test. The explanatory variables were: the time they breastfed previous children, in months; and the sociodemographic, obstetric and prenatal variables, with yes or no answers.
Data were stored in an electronic Excel spreadsheet, and validated by means of duplicate typing. Statistical analysis was performed with the program Statistical Package for Social Sciences (SPSS), version 16.0. Data were presented as absolute and relative frequencies, and as for the quantitative variables, mean values (central tendency measures), standard deviations and minimum and maximum values (variance measures) were calculated. Bivariate analysis was used to identify the relationship between the variable answer and the explanatory variables. The summary measures (means of correct answers) were compared with the different groups of factors defined by the categorical variables, with the application of Student’s t test. Pearson’s linear correlation coefficient (r) was used in the analysis of the correlation between the mean of correct answers and the time of breastfeeding provided to previous children. Data normality was verified by means of the Kolmogorov-Smirnov test. The level of significance of the p-value, adopted for the tests, was α under or equals 0.05.
The research proposal was approved by the local Research Ethics Committee of Universidade Federal do Triângulo Mineiro (Process no. 1152/2008), as per resolution 196/96 of the National Health Council. The study was developed in compliance with ethical standards, respecting human dignity and the use of the FICF.
RESULTS AND DISCUSSION
Profile of the subjects
The age of the study participants varied between 12 and 44 years, mean of 24.7 (SD=6.5) years, with 118 (83.7%) of them being 19 years old or over. These data confirm the findings of studies developed in the states of Rio Grande do Sul22 and Ceará23, in which the mean age of the women was 27.4 and 23.9 years, respectively. Another study developed in the same rooming-in as the present study12, revealed that most of the postpartum women (89.6%) were over 18 years of age.
The studied group was made of 95 (67.4%) women who were married or lived with a partner. Studies developed in rooming-ins of two maternity hospitals in Fortaleza revealed that 80%23 and 75.8%7 of the interviewees were married or lived in common-law marriage.
Regarding education, 87 (61.7%) parturients had nine or more years of education. The participants of studies developed in Saudi Arabia14, India15, and in the Brazilian states of Minas Gerais12, Ceará7,9,23, São Paulo24 and Mato Grosso11 also stated they had studied for nine or more years. However, these findings differ from those identified in a study developed in two hospitals of Viçosa, Minas Gerais5, in which 78% of the participants had eight years of education or less.
As for their position in the work market, 83 (58.9%) participants did not have a paid activity and 58 (41.1%) were formally or informally employed. Similar results were found in studies developed in Ceará7,25, Mato Grosso11 and Bahia26, in which most of the women (73%, 80%, 73% and 55.7%, respectively) did not perform any paid activity either.
As for prenatal care, 140 (99.3%) women stated they attended prenatal visits and, among those, 109 (77.9%) attended six or more visits, which is the minimum number of visits recommended by the Ministry of Health27. Surveys developed in Minas Gerais5, Ceará9,23 and Mato Grosso11 evidenced that more than 90% of the women interviewed attended prenatal visits. On the other hand, in Saudi Arabia, a little more than half the participants received medical care during pregnancy14. A study developed in Rio Grande do Sul22 revealed that 71.7% of the women attended five or more prenatal visits.
From all the women who received prenatal care, 105 (75%) were guided as for breastfeeding in this period, a similar datum to that found in studies developed in Minas Gerais12, Ceará23, São Paulo24, Saudi Arabia14 and Jordan28. The authors believe that this situation represents, somehow, a limitation in the prenatal care offered, since it is expected that all women followed-up during pregnancy receive guidance regarding breastfeeding from health professionals, either individual or collectively.
It is important to highlight that the main source of guidance was the health professional, especially the nurse. In total, 70 (66.7%) participants were guided by this professional, whereas 30 (28.6%) received guidance from physicians, social workers and professors from courses in the health area. There were also 5 (4.8%) interviewees who stated they did not know the professional category of person responsible for this guidance. In Santo André, São Paulo24, most (54.3%) of the participants stated that the professional responsible for guiding them was the nurse, which confirms the finding of the present study and reinforces the role of nursing in the promotion, protection and support to breastfeeding29.
Regarding parity, 59 (41.8%) women were primiparous and 82 (58.2%) were multiparous. Among these, 69 (84.1%) had already breastfed and 13 (15.9%) had no prior experience. The total time through which these 69 women breastfed their children varied between one and 48 months, with mean of 15 (SD=1.1) months. A study developed in Viçosa, Minas Gerais5, showed that 59% of the women had more than one child. On the other hand, another study developed in a maternity hospital in Fortaleza, Ceará23, verified that most (55.8%) of the participants were primiparous.
As for previous experience in breastfeeding, studies developed in Rio Grande do Sul22, India15 and Ireland16 evidenced that most of the women had already breastfed.
The mean time of breastfeeding provided to the previous children of the 69 (84.1%) women, participating in this study and who had prior experience, is distant from the time recommended by the WHO, which is two years or more of complemented breastfeeding. However, it exceeds the national mean (11 months) and that of the capital city of the state of Minas Gerais (10 months)2. In a study developed in the municipality of Horizonte, Ceará25, the time of breastfeeding provided by the participants was nine months, which is less than that found in the present study.
Knowledge regarding breastfeeding
The comparisons between the means of correct answers in the knowledge test of the different groups, defined by the categorical variables, are presented in table 1.
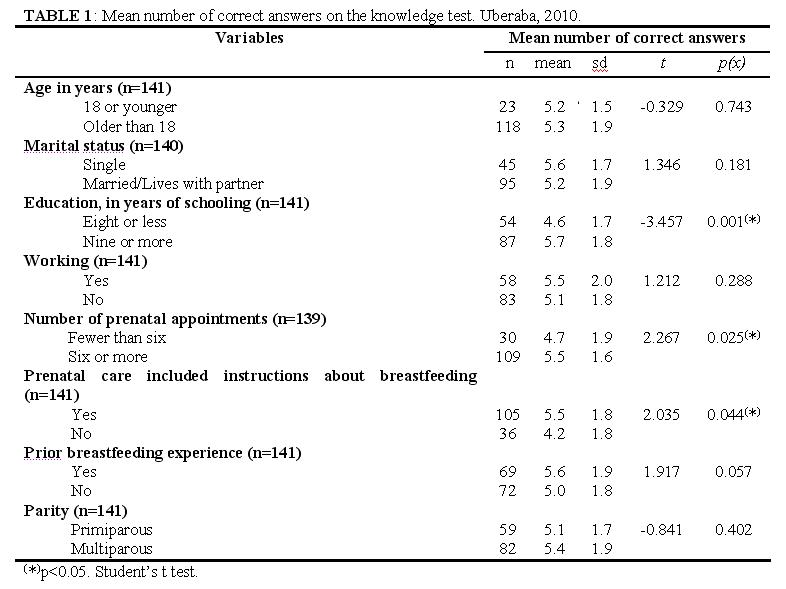
The findings presented in table 1 provide evidence that studying for nine or more years (p=0.001), attending six or more prenatal visits (p=0.025) and receiving guidance regarding breastfeeding during pregnancy (p=0.044) increase the knowledge of women on the subject (p value=0.009).
A study developed in Fortaleza, Ceará, verified that women with eight or more years of education had a greater knowledge regarding the benefits of breastfeeding9. In Ireland, women with less knowledge on breastfeeding had lower educational levels16, whereas in India15 those with greater educational level had a higher score in the knowledge tests, which confirms the findings of the present study.
A lower level of education may be a risk factor to stop breastfeeding early, due to the limitation in knowledge and the poorer ability to understand and absorb, properly, the information received, complicating the effectiveness of educational actions11,30,31. On the other hand, women with greater educational level, especially those with higher education, understand more easily the instructions received and are less influenced by the information of others, rejecting practices that are harmful to breastfeeding. In addition, a greater educational level generates self-confidence and security in women to deal with the common discomforts and complications in the lactation period32,33.
owever, there are divergences in the scientific literature as for the association of the educational level and the prevalence and duration of breastfeeding, reinforcing the fact that the success of this social practice is associated with multiple factors, not only the number of years of education11
.
A study developed in a public maternity hospital in Fortaleza revealed that, among the parturients with more than six prenatal visits, most of them answered specific questions regarding breastfeeding correctly, in the knowledge test9. Another study developed in Nigeria evidences that mothers with four or more prenatal visits were more likely to provide exclusive breastfeeding to their babies34. In Minas Gerais, Brazil, women who received guidance on this matter had a greater chance of answering the question regarding poor milk correctly13. A community-based study developed in India15 revealed that women who received guidance on breastfeeding presented satisfactory knowledge regarding the subject, similar to the findings of the present study.
These findings suggest that health professionals are providing appropriate guidance on breastfeeding during prenatal34. The attendance to six or more prenatal visits assure qualified and humanized care to the pregnant woman and offers important instructions regarding breastfeeding35. Learning the aspects related with the breastfeeding practice is essential so that mother and child can experience this moment effectively and calmly, receiving necessary and appropriate information from the health professional, still during pregnancy36. All pregnant women need information and support in order to develop the skills necessary to breastfeed25. Health education is an important tool that aims to broaden the knowledge of individuals regarding their own health, especially in terms of breastfeeding. Moreover, structured and properly elaborated educational interventions contribute to increase the duration of exclusive breastfeeding7.
The prenatal visit is an important occasion to promote breastfeeding, and it is the professional’s duty to encourage the woman to practice it37. The guidance received by pregnant women during prenatal care improves their knowledge on breastfeeding and, consequently, increases the prevalence of this social practice, especially if provided by a qualified professional38. During pregnancy, the woman has enough time to assimilate the information received and clarify her doubts10.
Pearson’s correlation coefficient allowed to verify a weak correlation (r=0.05) between the mean of correct answers, in the knowledge test, and the time the women breastfed previous children (p=0.710).
A study developed in Ceará evidenced that the knowledge regarding EB was associated with the women’s prior experience in breastfeeding and the duration of breastfeeding provided to their children8. Despite the supposition that the previous experience in breastfeeding increases the knowledge of women on the subject, this was not the reality found by the present study. Some women breastfed their children for longer periods, even though they did not have a greater level of knowledge on breastfeeding. This fact indicates the existence of other factors, besides knowledge, which may contribute to the success and duration of breastfeeding and deserve to be studied in order to understand their relations and implications.
The authors evidenced, in this study, that postpartum women with greater knowledge on breastfeeding had studied for nine or more years, attended six or more prenatal visits and received guidance regarding breastfeeding during pregnancy.
These findings contribute to improve care and research in the health area. The identification of the aspects related with the knowledge of parturients on breastfeeding allows to propose educational programs, to reorganize health services and to implement specific and targeted actions, contributing to keep this practice.
Therefore, during the delivery of care to women in the pregnancy-puerperal cycle, nurses must take into consideration the insertion of the knowledge and practice of breastfeeding in a sociocultural context. Based on this approach, it will be possible to identify the real needs of mother and child and the aspects related with the knowledge of pregnant women and nursing mothers.
REFERENCES
1. Yanikkerem E, Tuncer R, Yilmaz K, Aslan M, Karadeniz G. Breast-feeding knowledge and practices among mothers in Manisa, Turkey. Midwifery. 2009; 25:19-32.
2. Venancio SI, Escuder MM, Saldiva SR, Giugliani ER. Breastfeeding practice in the brazilian capital cities and the Federal District: current status and advances. J Pediatr. 2010; 86:317-24.
3. Junges CF, Ressel LB, Budó MLD, Padoin SMM, Hoffmann IC, Sehnem GD. Perceptions of women in puerperium regarding factors that influence breast feeding. Rev Gaúcha Enferm. 2010; 31:343-50.
4. Almeida JAG, Novak FR. Breastfeeding: a nature-culture hybrid. J Pediatr. 2004; 80:119-25.
5. Percegoni N, Araújo RMA, Silva MMS, Euclydes MP, Tinôco ALA. Knowledge about maternal nursing of mothers attended at two hospitals in the city of Viçosa, Minas Gerais, Brazil. Rev Nutr. 2002; 15: 29-35.
6. Nakano MAS, Reis MCG, Pereira MJB, Gomes FA. Women's social space and the reference for breastfeeding practice. Rev Latino-Am Enfermagem. 2007; 15: 230-8.
7. Azevedo DS, Reis ACS, Freitas LV, Costa PB, Pinheiro PNC, Damasceno AKC. Knowledge of primiparous about the benefits of breastfeeding. Rev RENE. 2010; 11:53-62.
8. Komarsson KAC, Oriá MOB, Dodt RCM, Almeida PC, Ximenes LB. Mother’s knowledge about breastfeeding: a descriptive study. OBJ Nursing. 2008; 7 (2). [citado em 10 fev 2013]. Disponível em: <http://www.objnursing.uff.br/index.php/nursing/article/view/1558>.
9. Silva VMM, Joventino ES, Arcanjo DS, Veras JEGLF, Dodt RCM, Oriá MOB, et al. Postpartum women’s knowledge about breastfeeding - a descriptive study. OBJ Nursing. 2009; 8 (3). [citado em 10 fev 2013]. Disponível em: <http://www.objnursing.uff.br/index.php/nursing/article/view/2452>
10. Saes SO, Goldberg TBL, Ondani LM, Valarelli TP, Carvalho AP. Knowledge about breastfeeding among adolescents and adults puerperae. Rev Paul Pediatr. 2006; 24:121-6.
11. Egues EMS, Kogien M, Teixeira CA. Knowledge over mother`s breastfeeding attended by the children clinic in the city of Cáceres, Mato Grosso, Brazil. Rev Enferm UFPE Online. 2010; 4:1471-6.
12. Fonseca MO, Parreira BDM, Machado DC, Machado ARM. Breastfeeding: knowledge of mothers admitted to the rooming-in of a university hospital. Rev. Cienc Cuid Saúde. 2011; 10:141-9.
13. Campos AAO, Ribeiro RCL, Santana LFR, Castro FAF, Reis RS, Oliveira CA, et al. Practices of breastfeeding: a gap between knowledge and knowledge application. Rev Med Minas Gerais. 2011; 21:161-7.
14. Alwelaie YA, Alsuhaibani EA, Al-Harthy AM, Radwan RH, Al-Mohammady RG, Almutairi AM. Breastfeeding knowledge and attitude among saudi women in central Saudi Arabia. Saudi Med J. 2010; 31:193-8.
15. Kishore MSS, Kumar P, Aggarwal AK. Breastfeeding knowledge and practices among mothers in a rural population of north india: a community-based study. J Trop Pediatr. 2009; 55:183-8.
16. Zhou Qianling, Younger KM, Kearney JM. An exploration of the knowledge and attitudes towards breastfeeding among a sample of chinese mothers in Ireland. BMC Public Health. 2010; 10:722.
17. Buss PM. Promoção da saúde e qualidade de vida. Ciênc saúde coletiva. 2000; 5:163-77.
18. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Política nacional de alimentação e nutrição. 2ª ed. Brasília (DF): Ministério da Saúde; 2008.
19. Araújo RMA, Almeida JAG. Aleitamento materno: o desafio de compreender a vivência. Revista de Nutrição. 2007;20:431-8.
20. Pinto TV. Promoção, proteção e apoio ao aleitamento materno na comunidade: revisão das estratégias no período pré-natal e após a alta. Arquivos de Medicina. 2008;22:57-68.
21. Jones NBO, Cunha EL, Kammler NN, Kruno R. Mothers knowledge about breastfeeding. Rev Gaúcha Enferm. 1993;14:19-24.
22. Passarin GL, Santos JS. Knowledge of breastfeeding mothers in the hospital geral: Caxias do sul. Pediatria (São Paulo). 2009; 31:152-60.
23. Dodt RCM, Oriá MOB, Pinheiro AKB, Almeida PC, Ximenes LB. Epidemiological profile of postpartum women receiving rooming-in care. Rev Enferm UERJ. 2010; 18(3):345-51.
24. Souza N, Bernardes AC. Breastfeeding: prevalence and received information. Rev Port Clin Geral. 2010;26:440-8.
25. Nogueira, CMR. Conhecimento sobre aleitamento materno de parturientes e prática de aleitamento cruzado na unidade hospitalar e maternidade Venâncio Raimundo de Souza - Horizonte – Ceará [dissertação de mestrado]. Rio de Janeiro: Escola Nacional de Saúde Pública Sergio Arouca; 2009.
26. Rodrigues QP, Domingues PML, Nascimento ER. Socio-demographic profile os postpartum national health system users. Rev enferm UERJ. 2011;19:242-8.
27. Secretaria da Saúde (SP). Coordenadoria de Planejamento em Saúde. Assessoria Técnica em Saúde da Mulher. Atenção à gestante e à puérpera no SUS – SP: manual técnico do pré-natal e puerpério. São Paulo: SES/SP; 2010.
28. Khreshe R, Suhaimat A, Jlamdeh F, Barclay L. The effect of a postnatal education and support program on breastfeeding among primiparous women: a randomized controlled trial. Int J Nurs Stud. 2011; 48:1058-65.
29. Chaves MMN, Farias FCSA, Apostólico MR, Cubas MR, Egry EY. Breastfeeding: nurse’s practice under the perspective of the international classification of collective health nursing practices. Rev esc enferm USP. 2011;45:199-205.
30. Carrascoza KC, Costa Junior ÁL, Moraes ABA. The early weaning and extended breastfeeding influent factors. Estud Psicol. 2005; 22:433-40.
31. Joca MT, Oliveira RL, Barbosa RCM, Pinheiro AKB. Understanding maternal breastfeeding through the experience lived by the breastfed baby. Rev RENE. 2005; 6: 48-55.
32. Faleiros FTV, Trezza EMC, Carandina L. Factors influencing breastfeeding decision and duration. Rev Nutricional. 2006; 19:623-30.
33. França GVA, Brunken GS, Silva SM, Escuder MM, Venancio SI. Breast feeding determinants on the first year of life of children in a city of midwestern Brazil. Rev Saude Publica. 2007; 41:711-8.
34. Agho KE, Dibley MJ, Odiase JI, Ogbonmwan SM. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth. 2011; 11:2.
35. Ministério da Saúde (Br). Secretaria de Políticas de Saúde. Programa de humanização do pré-natal e nascimento. Brasília (DF): Ministério da Saúde; 2000.
36. Jones RH. Enfoque Obstétrico. In: Carvalho MRD, Tamez RN, editores. Amamentação: bases científicas. Rio de Janeiro: Guanabara Koogan; 2005. p. 151-65.
37. Ciconi RCV, Venancio SI, Escuder MML. Knowledge assessment of family health program teams on breast feeding in a municipality of São Paulo's metropolitan region. Rev Bras Saude Matern Infant. 2004;4:193-202.
38. Camarotti CM, Nakano AMS, Pereira CR, Medeiros CP, Monteiro JCS. The experience of breastfeeding in a group of teenage mothers. Acta paul enferm. 2011; 24(1): 55-60.
Received: 09.05.2012
Approved: 15.12.2013