RESEARCH ARTICLES
Hepatitis B: prevalence of serological markers in emergency nursing professionals
Telma Maria Evangelista de AraújoI; Nayra da Costa e SilvaII
IPh.D. in Nursing. Assistant Professor in Graduation and Master Program in Nursing from the Federal University of Piauí. Director of Vigilance and Health Care of Piauí State. Teresina, Piauí, Brazil. E-mail: telmaevangelista@gmail.com.
IIMaster degree in Nursing. Assistant Professor of Technological Center of Teresina/Federal University of Piauí. Teresina, Piauí, Brazil. E-mail: nayralygil@hotmail.com.
DOI: http://dx.doi.org/10.12957/reuerj.2014.6301
ABSTRACT: This study was quantitative, descriptive and transversal and aimed at evaluating the prevalence of serological markers for Hepatitis B in nursing professionals from the emergency services in Teresina, Piauí, Brazil. It was held from March to May, 2010, with 317 nurses from five public hospitals. Females (94.3%), married (54.6%), nursing technicians (59.9%), and the average employment length of 1-20 years (55.5%) predominated. There was no positivity for HBsAg and HBc total in the population investigated. Anti-HBs was found in greater evidence in nursing technicians and assistants (32.6%) and (31.7%), respectively. There was statistically significant association between anti-HBs and variables, number of vaccine doses and length of employment (p =0.03). The serological control of the Hepatitis B virus is important for the control of disease progression in nursing professionals, but the expansion of access to these measures is a major challenge.
Keywords: Hepatitis B; nursing; prevention; occupational health.
INTRODUCTION
The impact of Hepatitis B in the world has been represented by high morbidity and mortality rates. Estimates indicate that 360 million people are chronically infected and 600,000 people die per year due to acute or chronic consequences of the disease. The prevalence of chronic infection by hepatitis B virus (HBV) is highly variable, being of 0.1% in the United States to 20-30% in some Pacific Island1.
In Brazil, according to the epidemiological bulletin of 2012, the Southeast region concentrated 36.6% of cases, followed by the South, with 31.6% of the notifications, and the national average for hepatitis B cases in Brazil increased from 0.3% in 1999 to 6.9% by 20102.
Besides the prevalence of the disease in the population in general, the risk groups for hepatitis B should be observed with great caution. Epidemiological studies in specific groups consistent with the interest of this article, where the investigation of serological profiles of vulnerable groups as well as risk behavior, can lead to understanding of the factors that induce the disease exhibition3.4.
International Labor Organization data identify 160 million occupational diseases and 250 million accidents at work annually5. Hepatitis B is still the most prevalent disease among healthcare workers and it has contributed to the high rates of occupational diseases, constituting therefore a serious public health problem1.
Only with AIDS, in the decade of 80, there was a concern by the institutions governing the workers´ health, to establish standard precaution measures and rules for the activities in the working environment of health professionals. Research show that HBV circulates at high concentrations in the blood and lowly in other organic fluids, approximately 100 times more infectious than HIV and 10 times more than of Hepatitis C virus (HCV)6.
Within this problematic, the situation of serological professionals working in health services is essential for the prevention and control of HBV in the working environment. Thus, the objective of this study was to evaluate the prevalence of serological markers for hepatitis B in nursing professionals who work emergency services.
LITERATURE REVIEW
Structurally, HBV belongs to the Hepadnaviridae family, having 3,200 pairs of base, having its molecular form consisting of a core of double-stranded DNA and having two important antigens for determining the presence of the virus and the course of the disease, which are the central and surface antigen7.
The man is considered the only reservoir of epidemiological importance and can transmit the disease in several ways: parenteral (transfusion, before the policy of screening in blood banks; sharing needles, syringes or other equipment containing contaminated blood; medical/dental procedures with contaminated blood, tattoos and piercings); sexual (in unprotected intercourse); through continuity solution (skin and mucosa). There is evidence that suggests the possibility of transmission through manicure instruments, sharing toothbrushes, razors or shaving, straw of cocaine, crack pipe, among others1.
In general, the differential diagnosis of Hepatitis B is only possible through detection of serological markers. They are markers for hepatitis B screening: HBsAg (it is the first marker to emerge after HBV infection); Anti-HBc (it is a marker that indicates previous contact with the virus); Anti-HBc IgM (it is a marker of recent infection, therefore, it confirms the diagnosis of acute hepatitis B); Anti-HBs (indicates immunity against HBV); HBeAg (is indicative of viral replication and, therefore, high infectivity) and Anti-HBe (good prognostic marker in acute hepatitis by HBV)8.
The knowledge of the serological markers for hepatitis B is very important, since the serological situation of individuals exposed can determine the natural course of the disease and are essential to the development of strategies for the workers´ health9. Study on occupational exposure to bodily fluids among health workers in Georgia, reinforces the concern over the progression of Hepatitis B in the hospital environment about the vulnerability of the health professional to HBV exposure, where the results of these researches prove the presence of serological markers for hepatitis B in these professionals10.
METHODOLOGY
This is a quantitative, descriptive and transversal research, carried out through a serum-epidemiological investigation accomplished in five hospitals in the Municipal Health Foundation (MHF), providing services of urgent and emergency care to the population, as well as, ambulatory health care services, maternity and supporting the Family Health Strategy.
The population of the research was composed by nursing professionals of urgent and emergency services (n=360), distributed in three categories: nurses, technicians and auxiliaries. The exclusion criterion was the not consent on the participation in the study, being on vacation or on leave during the period of data collection.
The research was conducted according to ethical principles governing research involving human beings, approved by the Research Ethics Committee of the Federal University of Piauí UFPI-(CAAE number 0163.045,000-08).
The data were collected in the period from March to May 2010, through two steps: first, the interview was conducted through a form composed of questions related to the socio-epidemiological characteristics and serological situation of the research participants and in the second stage, serological tests were carried out, according to guidance of the Central Laboratory of Piauí (LACEN). The serological markers were researched with diagnostic purposes of hepatitis B (HBsAg, Anti-HBs, HBc Total), in the collection rooms of each hospital, morning and evening periods, respecting the scale on duty and industrial activities of the subjects of the study. The tests used were: HBsAg (Vikia®), HBc total (IEA WELL), Anti-HBs (IEMA WELL). This study took as case definitions: immune by infection (individuals with Anti-HBc and Anti-HBs positive), immune by the vaccine (individuals with Anti-HBs positive) and without protection (individuals with Anti-HBc and Anti-HBs negative).
The variables raised were: age, gender, marital status, professional category, time of profession, serological markers, time of vaccination and number of doses of vaccines received against hepatitis B.
For data analysis a database was built, which was explored through univariate and bivariate techniques using statistical analyses using the software Statistical Package for the Social Science (SPSS) 17.0. Univariate analysis was conducted through the calculation of descriptive statistics of the variables related to the description of the sample and the hepatitis B serology before to the research. The bivariate analysis, the Pearson Chi-square (χ2) was calculated, aiming to identify possible associations between the dependent variables (results of Anti-HBs and HBc Total) with each independent variable. The null hypothesis was rejected when the p value was less or equal to 0.05. The most significant findings were represented in tables and subsequently were analyzed based on the scientific production of the authors of the subject area.
The population planned to participate in the study was 360 professionals. However, 39 were away for vacation or on leave in the period of data collection, being removed from the research by the exclusion criteria provided in planning. Among the 321, four refused to participate in the research, totaling 317 professionals studied.
RESULTS AND DISCUSSION
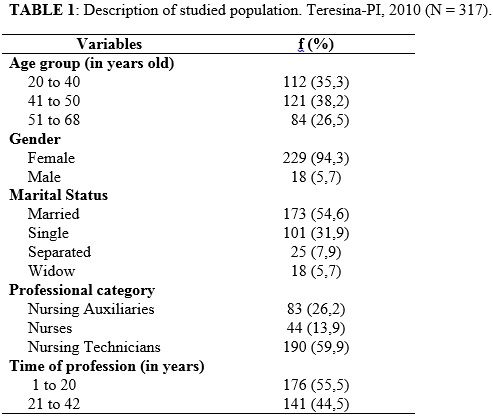
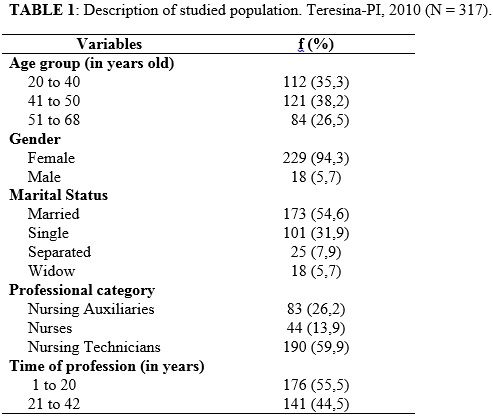
Of the 317 professionals who participated in the study, 121 (38.2%) were between 41 to 50 years old, females predominated with 229 (94.3%) and, with regard to marital status, 173 (54.6%) were married. In the professional category, the nursing technicians represented 59.9% of the sample and the average time of profession was of 1 to 20 years. On the characterization of the study subjects, statistics show that women represent 73.0% of jobs in healthcare. The increased female participation in the nursing work, started in the 70s, with still constant predominance in this sector11.12.
Socio-demographic aspects of study participants are shown in Table 1.
Regardless of level of education, nursing professionals are vulnerable to contamination by various microorganisms in the hospital environment. When comparing the other occupational categories, research are unanimous by showing that the nursing staff suffers an accident with greater frequency in the hospital environment13-15. This fact is similar to this research, in which a significant percentage of nursing professionals reported to have suffered some kind of accident with biological material (47.9%) and the accident with needle was the largest proportion (36.9%).
One of the prophylactic measures in controlling the progression of Hepatitis B is the serological control. Health professionals practicing hospital practices should follow the following: prior immunization with hepatitis B vaccine, serological control of Anti-HBs and to those who have not yet completed the schema against hepatitis is necessary to search for the presence of HBsAg. In case of not reaction condition, they must complete the schema and, after an interval of one to six months, perform the serological control16.17.
When they were investigated about the serology performance at some other moment preceding the research, the professional category of nursing assistants was the predominated in relation to others (91.6%) claiming never to have done this test.
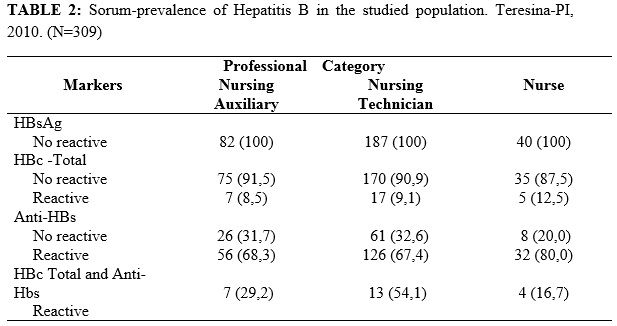
With the results of the serology for hepatitis B obtained in this study, it is verified that none of the professionals presented positivity for HBsAg and only 9.2% were reactive to total Anti-HBc, according to Table 2. This shows that, at some point in life, these participants had contact with the hepatitis B virus, because this marker is positive in the phase between the disappearance of antigens and the appearance of antibodies. Research of serological markers performed with healthcare professionals have found similar results - 9.4% and 8.1%, respectively, on the result of the Anti-HBc total18.19. However, some international studies in countries of high endemicity for HBV, show the presence of HBsAg marker in health professionals20.21.
It is observed that the nonexistence of positive cases of HBsAg in the population investigated can be justified by insufficient sample of carriers individuals, because the global prevalence of HBsAg marker, referring to all the capitals of Brazil and the Federal District is 0.37%, classified as low-endemicity22. However, even in low prevalence, the risk factors of the population investigated with the exposure to biological accidents and incomplete or missing vaccination schedule, are still gaps interfering with the control of the disease.
Another important marker of hepatitis B prevalence, conducted in this research, was the Anti-HBs. It arises after the disappearance of HBsAg and indicates that the individual is immune to infection by the virus or by full immunization. In this study, a significant percentage of respondents (30.3%) was not reactive to this marker.
Similar findings were reported in a research conducted in a private hospital, where 1,115 serologies for Anti-HBs were held in health professionals of low or high risk for the occurrence of occupational accidents23. From the examinations, 729 were reactive and 386 nonreactive, characterizing a serum-positivity of 65.4%. However, a divergent study pointed out that only 2.4% of the surveyed showed positive results for Anti-HBs24.
In the results of serological markers, it was observed that 24 participants, distributed in three occupational categories, presented simultaneously positivity for markers HBc-total and Anti-HBs, demonstrating that they are immune to infection. Immunity naturally acquired is established by the concomitant presence of Anti-HBs and Anti-HBc IgG or total. Eventually, the Anti-HBc might be the only indicator of natural immunity serologically detectable, because over time, the level of Anti-HBs considered protector (10 m IU/ml) may become undetectable. The occurrence of Anti-HBs, as isolated marker of immunity against HBV, naturally acquired is possible, although it is very infrequent. Thus, people with serologic profile HBsAg, Anti-HBc and Anti-HBs negative are susceptible to pathology25.
In this study, there was a statistically significant association between Anti-HBs with the number of doses of hepatitis B vaccine (p=0.03), shown in Table 3. This vaccine offers good protection when administered in doses and especially with appropriate intervals. However, in people with advanced age, the answer is less effective26. Similar research agreed with this one when associates the values of Anti-HBs to the number of doses of the vaccine among health professionals24.
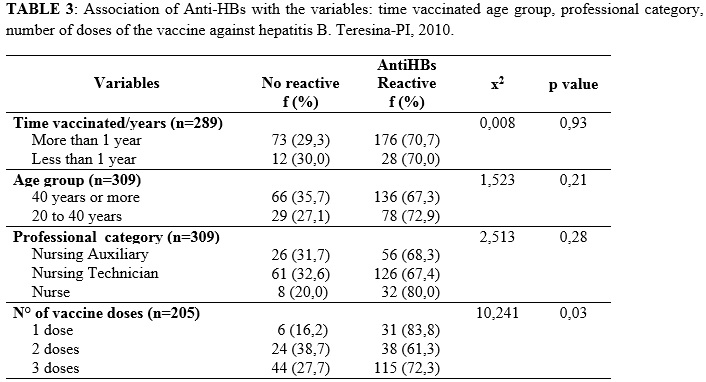
The duration of immunity after vaccination against hepatitis B has been the subject of many researches. Another study demonstrated the decline of Anti-HBs sometime after vaccination. Among adults, Anti-HBs levels decline to less than 10 IU/ml in 7% to 50% of the vaccinated, 5 years after vaccination, and in 30% to 60% of vaccinated between 9 to 11 years after vaccination25.
The immunologic memory has been evidenced by the quick increase in Anti-HBs antibodies, followed by a booster dose administered several years after the primary series, an important fact for keeping protection, even when serum levels of specific antibodies are lo27. Despite having been seen by many scholars of the subject, strengthening the hepatitis B vaccine remains the focus of many debates.
The immune response depends on several factors. The advancing age worsens the response to vaccination due to the decrease of activity of T and B immune cells. This explains the fact that, in this study, 31.9% of surveyed with age above 40 were not reactive Anti-HBs marker18.
Being hepatitis B occupational disease more investigated in nursing professionals, it should be noted that knowledge of the serological situation of these workers constitutes a forms of control and prevention of the disease and these actions should be prioritized in hospital services and not only on the occurrence of occupational exposure28.
CONCLUSION
In the study was noticed that some specific areas such as urgency and emergency services, can encourage occupational exposures of all nature, providing a greater vulnerability to nursing staff.
As to investigated markers in the research, it is highlighted that although there has been found current infection by HBV, a considerable portion of professionals with protective titles unsatisfactory to confer immunity to the disease was detected, a fact that makes them susceptible to future contamination, if not seeking complete immunization or not to adopting the appropriate measures.
As limitations of the study, there are highlighted: the fear of submission to the collection and the results of the serology of nursing professionals, the everyday exhausting of emergency sectors that often hampered the progress of the study. It is hoped that this study will encourage health professionals, in particular, the nursing staff, to a reflection on the progression of Hepatitis B, such as occupational disease, to adopt actions that can minimize the risks in the workplace.
REFERENCES
1.World Health Organization [Internet].Hepatitis B.2014.[citado em 15 out 2014] Disponível em: http://www.who.int/mediacentre/factsheets/fs204/en/
2.Ministério da Saúde (Brasil), Secretaria de Vigilância em Saúde /Departamento de DST, Aids e Hepatites Virais. Boletim epidemiológico Hepatites Virais. Brasília (DF): Ministério da Saúde; 2012.
3.Lopes LPL, Teles SAT, Romão EA, Toffano SEM, Rocha DFNC, Gir E. Vacinação contra Hepatite B em indivíduos renais crônicos em tratamento hemodialítico. Rev enferm UERJ. 2014; 22: 309-13.
4.Rossi GC, Afonso PMD, Oliveira SLGO, Furlan MLS. Hepatites B e C: o conhecimento dos estudantes universitários da área da saúde. Rev enferm UERJ. 2010; 18: 38-41.
5.Gasparini LR. Controle de infecção. São Paulo: Becton Dickinson; 2005
6.Center for Disease Control and Prevention [Internet]. Recommendations for prevention of Hepatitis B and C.2008 [cited in 2014 Jun 2014] Available in: http://www.cdc.gov/hepatitis/HBV/TestingChronic.htm
7.Khouri M, Santos V. Hepatitis B: epidemiological, immunological, and serological considerations emphasizing mutation. Rev Hosp Clín. 2004; 59:97-100.
8.Ministério da Saúde (Brasil), Programa nacional de hepatites virais. Manual de aconselhamento em hepatites virais. Brasília (DF): Ministério da Saúde; 2005.
9.Caetano MM, Beck ST. Importância da detecção de anticorpos anti-HBc na prevenção da transmissão do vírus da Hepatite B (VHB) em bancos de sangue. RBAC. 2006; 38: 235-7.
10.Butsashvili M, Kamkamidze G, Kajaia M, Morse DL, Triner W, DeHovitz L, McNutt LA. Occupational exposure to body fluids among health care workers in Georgia. Occup Med. 2012; 62:620–6.
11.Moraes EL. Relação gênero e raça na política pública de qualificação social e profissional. Brasília (DF): Ministério do Trabalho e Emprego; 2005.
12.Almeida MCP, Robazzi MLCC, Scochi CGS, Bueno SMV, Cassiani SHB, Saeki T, et al. Perfil da demanda dos alunos da pós-graduação scricto sensu da escola de enfermagem de Ribeirão Preto, da Universidade de São Paulo. Rev Latino–Am. Enferm. 2004; 12: 153-61.
13.Ribeiro EJG, Shimizu HE. Acidentes de trabalho com trabalhadores de enfermagem. Rev Bras Enferm. 2007; 60: 535-40.
14.Balsamo AC, Felli VEA. Estudo sobre os acidentes de trabalho com exposição aos líquidos corporais humanos em trabalhadores da saúde de um hospital universitário. Rev Latino-Am. Enferm. 2006; 14: 346-53.
15.Pinho DLM, Rodrigues CM, Gomes GP. Perfil dos acidentes de trabalho no Hospital Universitário de Brasília. Rev Bras Enferm. 2007; 60: 291-4.
16.Araújo TME, Paz EPA, Griep RH. Cobertura vacinal dos profissionais de um curso de especialização em Saúde da Família do Piauí.Esc. Anna Nery. 2006; 10: 95-100.
17.Pinheiro J, Zeitoune RCG. Hepatite B e a saúde do trabalhador de enfermagem. Esc Anna Nery.2008; 12: 258-64.
18.Ciorlia LAS, Zanetta DMT .Hepatitis B in healthcare workers: prevalence, vaccination and relation to occupational factors. Braz J Infect Dis.2005; 9: 384-9.
19.Kondili LA, Ulginaku D, Haidini M, Basho M, Chionne P, Madonna E, et al. Hepatitis B virus Infection in health care workers in Albania: a country still highly endemic for HBV Infection. 2007. [cited in 2010 Jan 01]. Available in: http://www.springerlink.com/content/15v0738329p0058x/
20.Doddaiah V, Janakiram K, Javagal S. Seroprevalence of Hepatitis B virus and Hepatitis C virus in healthcare workers - AIMS, B G Nagara. Am J Life Sci. 2013; 1(4):145-9.
21.Mosendane T, Kew MC, Osih R, Mahomed A. Nurses at risk for occupationally acquired blood-borne virus infection at a South African academic hospital. S Afr Med J. [Internet]. 2012. [cited in 2014 Nov 15] Available in: http://www.samj.org.za/index. php/samj/article/view/4563/392022.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde /Departamento de DST, Aids e Hepatites Virais. Hepatites virais no Brasil: situação, ações e agenda. Brasília (DF): Ministério da Saúde; 2011.
23.Shin BM, Yoo HM, Lee AS, Park SK. Seroprevalence of Hepatitis B virus among health care workers in Korea. J Korean Med Sci, 2006; 21: 58-72[cited in 2014 Nov 08] Available in: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2733980/
24.Silva PA, Fiaccadori FS, Borges AMT, Silva SA, Daher RR, Martins RMB. Seroprevalence of hepatitis B virus infection and seroconvertion to anti-HBsAg in laboratory staff in Goiânia, Goiás. Rev Soc Bras Med Trop. 2005: 38(6): 153-6.
25.Ciorlia LAS, Zanetta DM. Significado epidemiológico dos acidentes de trabalho com material biológico: hepatites B e C em profissionais da saúde. Rev. Bras. Med. Trab.2004; 2: 191-9.
26.Nazar AN. Bastos AP, Pittella AM, Matos HJ. Análise da soropositividade do Anti-HBs em profissionais de saúde. Cad Saúde Colet. 2008; 16: 421-36.
27.Faraht C, Carvalho ES, Weckz L, Carvalho LHFR, Succi LCM. Imunizações: fundamentos e prática. São Paulo: Atheneu; 2000.
28.Toledo AD, Oliveira AC. Situação vacinal e sorológica para hepatite b entre trabalhadores de uma unidade de emergência. Rev enferm UERJ. 2008; 16: 95-100.