ORIGINAL RESEARCH
Prevalence of under-diagnosis of delirium among patients in an intensive care unit
Aline Affonso LunaI; Aline Piovezan Entringer II; Roberto Carlos Lyra da SilvaIII
I
Ph.D. student in Nursing and Bioscience by the Federal University of Rio de
Janeiro State. Brazil. E-mail: aline-luna@hotmail.com
II
Ph.D. student in Children and Women´s Health of the Institute Fernandes
Figueira/Oswaldo Cruz Foundation. Rio de Janeiro, Brazil. E-mail: alineentringer@gmail.com
III
Ph.D. in Nursing. Associate Professor of the Fundamental Nursing Department
of the Federal University of Rio de Janeiro State. Brazil. E-mail: proflyra@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.6238
ABSTRACT
Introduction: delirium is a neurological disorder often presented by severe patients in Intensive Care Units. Objective: to identify the prevalence of delirium among patients admitted to an Intensive Care Unit (ICU) in Rio de Janeiro State. Method: this retrospective, cross-sectional study was conducted in February, March and April 2012. The medical records of 128 hospitalized patients were examined for general patient characteristics and information on level of consciousness and mental state, using a data collection instrument created specifically for the purpose. Results: a confirmed diagnosis was found in only two patients, with a 2% prevalence of delirium. Conclusion: the results point to the need for more extensive discussion of the use of evaluation protocols for diagnosis of delirium by ICU personnel, so that the disease can be detected early for prevention and/or appropriate treatment during hospitalization.
Keywords: Nursing; nursing care; confusion; intensive care.
INTRODUCTION
Delirium is a neurological disorder often manifested by critically ill patients in intensive care units (ICU). Its relevance is not only due to the high incidence but, above all, its influence on morbidity, mortality, and length of hospital stay, resulting in greater social and financial costs of tretment1,2. Its prevalence in patients admitted to the ICU varies between different studies and can affect up to 80% of critically ill patients on mechanical ventilation3.
This study is part of the results of a dissertation defended in nursing in 2013 at the Federal University of the State of Rio de Janeiro (UNIRIO). For this research, the following question was created: What is the prevalence of delirium among patients admitted to the ICU of the State of Rio de Janeiro?
Therefore, the aim was to identify the prevalence of delirium among patients admitted to the ICU of the State of Rio de Janeiro.
LITERATURE REVIEW
Delirium is a state of potentially reversible acute confusion that develops in a short period (hours or days). It occurs as a direct result of a medical condition, intoxication or abstinence, medication, exposure to toxins, or a combination of them4,5. Technological resources such as multi-parameter, respirators, infusion pumps and pulse oximeters with their visual and audible alarms are essential inputs to the process of work teams to alert the patient's clinical changes and malfunctioning of the devices6. However, they can contribute actively to the development of delirium in hospitalized patients.
The clinical picture varies according to the type of delirium are hyperactive or hypoactive. A patient hypoactive presents sleepy while the hyperactive presents an important psychomotor agitation and hallucinations. The most common picture of delirium is hypoactive while the hyperactive is relatively rare, less than 5% 7.
Attention deficit is a most apparent phenomenon, but can be observed other cognitive and behavioral disorders such as loss of memory, hallucinations and agitation. Despite its clinical importance, delirium remains considerably sub-diagnosed, despite its high prevalence in the ICU, in percentages between 25 and 75%, reaching 100% in its hypoactive type 8.
Nursing has a basic role in the assessment and identification of cognitive impairment presented because we believe that the professional team remains 24 hours with the patient, and any oscillation of the mood is easy to identify9. However, sometimes, reading this change does not occur optimally, masking an important diagnosis that can result in serious consequences for hospitalized patients, raising a supporting diagnosis to the real reason for hospitalization.
Delirium , if not diagnosed, usually evolve an unfavorable outcome rather, to the extent that proper treatment and follow-up of the patient ceases to be done. Thus, considering the high morbidity and mortality rates related to delirium, patient safety is very committed, as well as the quality of care in services to society, which implies the effectiveness, safety, and optimization of results10.
METHODOLOGY
This was a retrospective and cross-sectional study in the months of February, March and April 2012. The study involves collecting data on the present result and then look at the past in search of possible causes or antecedents11.
The setting of choice to conduct the research consisted in a general ICU of the State of Rio de Janeiro, comprising 35 beds receiving adult patients with various clinical and surgical pathologies, from intro transfers and inter-hospital.
The sample inclusion criteria include all patients who remained hospitalized for a period exceeding 24 hours, excluding patients under 18 years old, regardless of having records relating to the variables considered in the study or not.
The production data was in July 2012, through a careful analysis of all daily records of physicians and nurses found in the charts of patients who were hospitalized during February to April 2012, obtaining a sample of 128 patients.
An instrument composed of previously selected criteria was used integrating the scale validated in Brazil of the Confusion Assessment Method in the Intensive Care Unit (CAM-ICU)12, aiming to work with the evaluation variables of attention deficit (ability to receive information and run it), level of consciousness (orientation, disorientation or oscillation of this state) and psychomotor status (aggression, agitation, apathy or oscillation of this state). Also, variables were included to meet the factors that enable the identification of diagnostic delirium as the literature describes, such as gender, age, and main disease.
Only the medical records depicting a finding of fluctuation (fluctuation) of the level of awareness and psychomotor change were considered, which caused the patient to be eligible for application range of the CAM-ICU by evaluating the nurses and doctors of the ICU, composing the first criterion evaluated.
It is important to note that the patient needs to present a change of consciousness to assess the scale, which is followed to step two of the scale, which evaluates the patient´s care. In this step, it is read aloud the following letters: SAVEAHAART and asked him to tighten the examiner's hand only when he hears the letter A. It was considered an error when the patient does not shake hands when he hears the letter A and when shakes hands when he hears a different letter. If he presents three errors or more and keeps the altered level of consciousness, the patient already has a diagnosis of delirium.
Otherwise, it was followed the evaluation scale by step regarding the disorganized thinking. In this step, the examiner will make four questions that have no easy answers such as, Are there fish at sea? Moreover, he will also give a command easily executable. If the patient has two or more errors, he has the diagnosis of delirium.
In the scenario where there was data collection, there is no standardization of the use of mental evaluation scales very clear and defined, at the discretion of the professional to use or not and, especially, with the subjectivity to evaluate each.
It is important to note that the sample was not probabilistic intentional, as the records of the patients were selected according to inclusion and exclusion criteria in the defined period.
Data were organized in spreadsheets using Excel 2010® program and later worked statistically through the simple frequency.
The study was consent by the general direction of the hospital to access the files and approved by the Research Ethics Committee of UNIRIO through of the consolidated number 28590 of 05/30/2012. The confidentiality of the data was respected.
RESULTS AND DISCUSSION
The results showed that the age of the 128 patients in the sample was mostly in the range greater than 59 years old (60.9%), some female patients were represented by 48% and males by 52%. Among the main predisposing underlying conditions for the involvement of delirium, it was found that the most prominent were systemic arterial hypertension (SAH) with 41% and metabolic disturbances during hospital stay with 60%. The average hospital stay was 11.7 days.
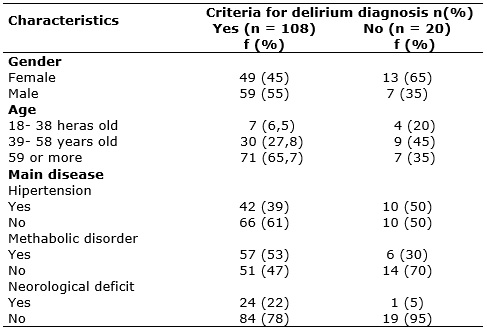
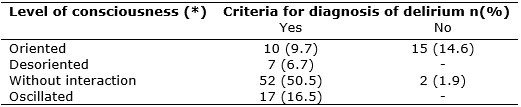
It was identified 65.7% of patients aged over 59 years old who presented clinical criteria for the diagnosis of delirium. As regards the main diseases, a high percentage of patients with metabolic disorder and hypertension, 53%, and 39% respectively with clinical criteria for the diagnosis of delirium. However, according to the total quantity of the sample patients, 108 (84%) had clinical criteria for identification of the diagnosis of delirium, documented by Sub-diagnosis phenomenon, as shown in Table 1.
TABLE 1:
Base chracteristics of the sample. Rio de Janeiro, 2012.
However, through reading and analysis of records of nurses and doctors in the medical records, only 2 (2%) of 128 patients in the sample were only indicated by written confirmation of the diagnosis of delirium, which contradicts the marked findings in Table 1.
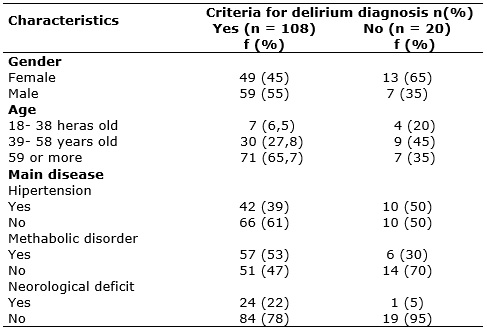
To define the diagnostic criteria, two important variables were analyzed that characterize the level of consciousness and the mental state of the patient. The first was checked through the indicators orientation, disorientation, without interaction, and oscillation of this state. It can be seen a deficiency in the records, which do not show information about the level of awareness of these patients, accounting for 25 (20%) of the total analyzed.
Evaluating the documentation of the level of consciousness changes, there were criteria for identifying the diagnosis of delirium. However, there was 50.5% of patients who had no interaction with the examiner and the environment, as shown in Table 2.
TABLE 2:
Documentation of the level of consciousness changes. Rio de Janeiro, 2012.
(N=103)
(*): The level of awareness was not reported in 25 patients, 22 with
diagnostic criteria and 3 without diagnostic criteria
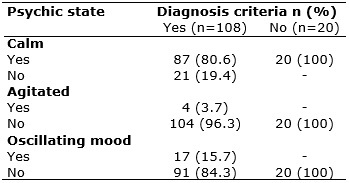
The mental status was investigated through the reports if the patient was calm, agitated or swaying the mood. A Large portion (80.6%) remained calm. However, it is identified that there was an oscillation of the mood in 15.7% of patients about the clinical criteria for the diagnosis of delirium, as seen in Table 3.
TABLE 3:
Documentation of the psychic state variables. Rio de Janeiro, 2012.
The data analyzed come from the records of the medical professional and nurses and revealed a delirium rate of around 2%. Although in this study, the prevalence of delirium can be considered low, given the estimated rates in the referenced literature, it was possible to identify the prevalence of sub-diagnosis in 84% of medical records of patients, according to clinical criteria for delirium, according to the CAM -ICU. In this sense, the study results are not so different to those found in the literature, at least regarding sub-diagnosis, which points out that, despite the high prevalence, delirium is still often sub-diagnosed, with rates that can be higher than 68%1-11.
Other studies also show that the simultaneous existence of documentation with no perception of the phenomenon may indicate less understanding of the specifics of this syndrome by nurses and also often not identified by doctors13,14.
The results also show a higher rate for males, marked by 66 (52%), which converges with literature and other related studies, considering males are more susceptible to the development of the phenomenon, and this fact may be related to any beliefs and stereotypes13.
Age appears as an important factor in the issue of sub-recognition because the as the patient is older, the smallest the sub-diagnosis of delirium12. Possibly, professionals clearly have already decided that this profile of the population may be more susceptible to develop this kind of interlocutory appeal. Although, results do not point to this end in the developed research.
Gathering the age groups (59-79 years old or more) which include the age predisposing to the development of delirium (over 65 years old) by the CAM-ICU scale, there are n=78 (60.9%), where only one had, in fact, the diagnosis. This is a strong point of concern since it is one of the most common complications among hospitalized elderly patients and is associated with increased morbidity and mortality15,16.
It is noted the negligible percentage of patients with neurological disorders with clinical criteria for the diagnosis of delirium (22%), given the possible complications of hypertension and metabolic disorders, not infrequently related to brain injury impairments.
The level of consciousness and psychic condition of the patient is essential information to pervade the diagnosis of delirium by the CAM-ICU scale. The sample points, statistically just over half of the patients who had clinical criteria for the diagnosis of delirium performed without interaction with the environment (48.1%), which brings us to an association with patients who were without delirium or could be with hypoactive delirium, characterized by a decrease in the degree of response, introversion and apathy. Other studies show that the high prevalence of hypoactive delirium in critically ill patients contributes probably to the lack of identification of this syndrome by doctors14.
Although the oscillation level of consciousness has shown timidly, it is still rather worrying, since this instability of orientation/disorientation can compromise the patient hospitalized for the neurological syndrome. Delirium features altered consciousness, manifested by cognitive disorder and orientation disorders, memory, attention, thinking and behavior, involving sensory perception errors17.
Regarding the lack of written information, it was shown that 20% of the records were not of doctors and nurses on the level of patient awareness, even though clinical criteria for the diagnosis of delirium, without any indication that converges for diagnosis syndrome. Another study found in its results that 12.6% of patients did not have any record of the phenomenon or interventions, reinforcing the sub-diagnosis in the documentation13.
Regarding the mental state of the patient, there was a significant percentage of patients who were calm (80.6%), which at first appears to be positive, if it were not a strong indicator of hypoactive subtype, which also relates to the lack of interaction signed the records of the level of consciousness described above. These findings were also highlighted in other studies, showed that there are difficulties in establishing the diagnosis of the clinical situation8, which may be related to its characteristics (fluctuating nature of symptoms and hypoactive subtype) 18,19.
CONCLUSION
Analyzing records of professionals was quite complex and challenging, especially concerning the search for information to bring tangible data and reliable evaluations of patients.
Sub-diagnosis rates of delirium in this study are also very worrying and must be considered since some indicators have been reported in the medical records, not related to a possible delirium picture, which may explain the low prevalence found (2%), unlike what literature indicates.
The results of this research are similar to those found in other studies, which reinforces the understanding that the use of evaluation protocols for the diagnosis of delirium require further dissemination and use among professionals working in the ICU for early identification of grievance for the prevention and/or appropriate treatment during hospitalization, minimizing the vulnerabilities related to patient safety.
REFERENCES
1.Carrasco MG, Hoyl TM, Marin PPL, Hidalgo JA, Lagos CD, Longton CB et al. Subdiagnóstico de delirium em adultos mayores hospitalizados. Rev Méd Chile. 2005;133:1449-54.
2.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753-62.
3.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R et al. Evaluation of delirium en critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001;29:1370-79.
4.Ely, EW. Melhor avaliação e uma melhor gestão da unidade de cuidados intensivos delírio leva a resultados melhores para a unidade de cuidados intensivos sobreviventes: entrevista com um especialista. Medscape Critical Care. 2008.
5.Levkoff SE, Cleary P, Liptzin B, et al: Epidemiology of delirium: An overview of research issues and findings. Int Psychogeriatr. 1991;3:149-167.
6.Oliveira LB, Souza NVM. Estresse e inovação tecnológica em unidade de terapia intensive de cardiologia: Tecnologia dura. Rev enferm UERJ. 2012; 20(4):457-62.
7.Peterson JF, Pun BT, Dittus RS, Thomason JW, Jackson JC, Shintani AK, et al. Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc. 2006;54(3):479-84.
8.Tropea J, Slee J, brand CA, Gray L, Snell T. Clinical practice guidelines for the management od delirium in older people in Australia. Austr J Ageing. 2008;27(3):150-6.
9.Reicha R, Vieira DFVB, Lima LB, Silva ERR. Carga de trabalho em unidade coronariana segundo o Nursing Activities Score. Rev Gaúcha Enferm. 2015set; 36(3):28-35. Doi: http://dx.doi.org/10.1590/1983- 1447.2015.03.51367
10.Oliveira RM, Leitão IMTA, Silva LMS, Figueiredo SV, Sampaio RL, Gondim MM. Estratégias para promover segurança do paciente: da identificação dos riscos às práticas baseadas em evidências. Esc Anna Nery 2014;18(1):122-129.
11.Polit, DF, Beck CT. Fundamentos de pesquisa em enfermagem: avaliação de evidências para a prática de enfermagem. Tradução Denise Regina de Sales; revisão técnica Anna Maria Hecker Luz, Lísia Maria Fensterseifer, Maria Henriqueta Luce Kruse. 7ª Ed. Porto Alegre: Artmed; 2011.
12.Flores DG, Salluh JIF, Pizzol FD, Ritter C, Tomasi CD, Lima MASD, et al. The validity and reliability of the Portuguese versions of three tools used to diagnose delirium in critically ill patients. Clinics. 2011;66(11):1917–22. Doi: 10.1590/S1807-59322011001100011
13.Silva RCG, Paiva e Silva AA, Marques PAO. Análise dos registros produzidos pela equipe de saúde e da percepção dos enfermeiros sobre os sinais e sintomas de delirium. Rev. Latino-Am. Enfermagem [internet]. 2011.19(01): [09 telas].
14.Girard TD, Pandharipande PP, Ely EW. O delirium (síndrome confusional) na unidade de tratamento intensivo. Critical Care. 2008;12(supl.3): S3(dói:10.1186/cc6149).
15.Fernandes CR, Gomes JMA, Moraes RP, Marinho DS, Holanda MA, Oliveira FRA. Avaliação sistemática do delirium e da dor em pacientes criticamente enfermos. Rev Dor. 2009;10(2):158-168.
16.Santos FS. Delirium: Uma síndrome mental orgânica. São Paulo: Atheneu; 2008.
17.American Psychiatric Association. Practice Guideline for the Treatment of Patients with Delirium. Am J Psychiatr-Suppl.1999.156(5):1-20.
18.Michaud L, Büla C, Berney A, Camus V, Voellinger R, Stiefel F, et al. Delirium: guidelines for general hospitals. J Psychosom Res. 2007;62(3):371-83.
19.Carvalho JPLM, Almeida ARP, Flores DG. Escalas de avaliação de delirium em pacientes graves: revisão sistemática da literatura. Rev Bras Ter Intensiva. 2013;25(2):148-154.