RESEARCH ARTICLES
Occurrence of adverse events as indicators of quality of care in an intensive care unit
Camila Santos Pires LimaI; Sayonara de Fátima Faria BarbosaII
I
Graduate nurse from the Federal University of Santa Catarina. PhD student of the Post-Graduation in Nursing Program of the Federal University of Santa
Catarina. Member of the Group for Clinical Research, Technologies and Informatics in Health and Nursing. Florianópolis, Santa Catarina, Brazil. E-mail: camilasp87@gmail.com
II
Graduate nurse from the Federal University of Rio de Janeiro. PhD in Health Sciences. Assistant Professor, Department of Nursing at the Federal University
of Santa Catarina. Deputy leader of the Group for Clinical Research, Technologies and Informatics in Health and Nursing. Florianópolis, Santa Catarina,
Brazil. E-mail: sayonara.barbosa@ufsc.br
DOI: http://dx.doi.org/10.12957/reuerj.2015.6076
ABSTRACT
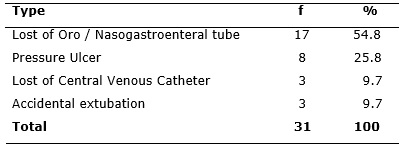
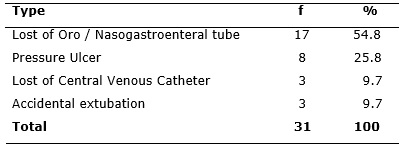
This descriptive, quantitative study in the intensive care unit of a hospital in southern Brazil, evaluated quality of care and patient safety by occurrence of adverse events. Data were collected in August and September 2012 using an instrument for notification of, and observations on, risk factors for adverse events. Of total notifications, 17 (54.8%) were for loss of gastrointestinal probe, 8 (25.8%) for pressure ulcer, 3 (9.7%) for loss of central venous catheter and 3 (9.7%) for accidental extubation. Of the risks observed, 74 (54%) were for pressure ulcer, 32 (23.4%) for loss of gastrointestinal probe, 22 (16%) for loss of central venous catheter and 9 (6.6%) for accidental extubation. This highlighted the importance of monitoring for events by applying quality indicators in order to improve patient safety and care. Keywords: Quality indicators in healthcare; quality; patient safety; intensive care unit.
INTRODUCTION
In recent years, it has been observed a worldwide growing concern for quality in health services, which is defined as the degree in which health services for individuals and populations increase the likelihood of desired outcomes and are consistent with the current professional knowledge1. The search for positive outcomes, patient satisfaction, a free care from harm, compliance with basic safety standards boost the health sector, especially hospitals to develop best practices2. However, this quest for quality improvement is not new because it started being discussed in the United States last century, in 1951, with the creation of the Joint Commission on Accreditation of Hospitals (JCAH) that soon, in 1952, officially delegated the accreditation program to the Joint Commission on Accreditation of Health Care Organizations (JCAHO)3.
In Brazil, the reference body for assessing the quality of services offered to health and deploying the accreditation process is the Organização Nacional de Acreditação (ONA), created in 19994. The ONA offers the Brazilian Manual of Hospital Accreditation, an instrument that serves as a guide for institutions so that they can achieve high quality service standards4. In this sense, nursing services play a fundamental role in the pursuit of that quality in health organizations, given the number of professionals working in institutions and their responsibility in patient care 24 hours a day5. Thus, to improve quality of care, one of the existing ways to assess and contribute to the quality of this service is the implementation of instruments called indicators, which are measurements used to determine, through time, the performance of functions, processes and results of an institution6.
One indicator that has been incorporated as guideline to monitor and evaluate the quality is the rate of adverse events (AE), which are undesirable, preventable and can cause harm to the safety of the patient under the care of health professionals7,8. The use of these indicators enables healthcare professionals to monitor and evaluate the events affecting patients, workers and organizations, pointing out, as a result, whether the processes and organizational results are meeting the needs and expectations of patients9.
The importance of using indicators is evident in various health care settings, however there is a greater need of its establishment in the Intensive Care Unit (ICU) because it is a place recognized as vulnerable to the occurrence of adverse events, due to the complexity of the clinical status of patients and the need for high-risk decisions on an urgent basis10.
The AE have been considered important indicators of quality of health services and the assistance provided, and although they are undesirable, these events are constantly observed in care practice, so it is critical to detect and monitor them through indicators11. In this scenario we developed the present study that aimed to evaluate the quality of care and patient safety through the occurrence of AE. We used the indicators of loss of gastroenteral tube, the incidence of pressure ulcers, accidental extubation and loss of central venous catheter.
LITERATURE REVIEW
The quality goal in the various services offered to society has been increasingly valued with consequent optimization of results. In the scope of health, institutions have incorporated this perspective in order to provide a safe care that meets the population needs12.
Historically, the first efforts regarding the health quality are assigned to Florence Nightingale, who in the mid-nineteenth century had demonstrated the need to statistically analyze hospital activities for the evaluation of results13.
One of the features that express the quality of care is patient safety, which is a critical element for quality and a key principle for patient care 14. Patient safety is part of a set of actions and complex efforts on performance of improvement of environmental safety and risk management, including infection control, safe use of medicines and equipment, safety of clinical practice and care environment15. Speaking on patient safety, we cannot fail to mention the Agency for Healthcare Research and Quality (AHRQ), which was established by the American Congress in 2000 14. Its mission is to improve the quality, safety, efficiency and effectiveness of health care for all Americans, and its main role is to contribute to the reduction of errors in the process of care and to improve patient safety16. The AHRQ believes that patient safety is the lack of potential for damage or absence of occurrence of associated damage to patient care16. It is, therefore, a fundamental component of quality health care 17.
One of the current challenges of healthcare organizations is to improve the quality of care through the implementation of quality indicators, which are screening tools for identifying potential areas of concern with the quality of clinical care and that reflect the quality of care in hospitals 18,19.
Thus, knowing and understanding the AE, their management, control and risk factors allows for the whole multidisciplinary team the implementation of preventive measures and effective treatment, and the scientific evidences are a source of encouragement and means to raise awareness of health professionals to the systemic approach of AE20. In this quest for quality and excellence in care, prevention of AE appears as a major challenge and one of the targets to be met by professionals who offer health care7.
METHODOLOGY
This is a descriptive study with a quantitative approach, developed in adult ICU of a public hospital in southern Brazil. The study population included patients admitted to the ICU. The sample was composed of patients admitted to the ICU during the months of August and September 2012 and included subjects of any age group and sex, who had suffered or had been at risk of being submitted to AE addressed in the study.
For data collection we used a reporting tool and conducted observations of risk factors for AE. A total of 31 occurrences of AE were recorded by nursing professionals, using a reporting tool (founded by the Commitment Program with the Hospital Quality) and deposited in a drop box in the ICU. The researcher and a previously trained professional carried out 102 observations, in the following work shifts and times: Morning - 7:30 a.m./10:30 a.m.; Afternoon – 1:30 p.m./4:30 p.m. and Evening – 7:30 p.m./10:30 p.m., and recorded 137 risks for the occurrence of AE.
Data were analyzed using descriptive statistics and the results are presented in absolute numbers and percentages. This study was conducted in compliance with Resolution No. 1196/96, which incorporates in the perspective of the individual and communities the four basic principles of bioethics: autonomy, non-maleficence, beneficence and justice, and aims to ensure the rights and duties of the scientific community, the research subjects and the State 21. It was started after approval by the Research Ethics Committee (REC), through the opinion No. 27870. From the data analysis the following categories emerged: Indicators of healthcare quality in intensive care and Risks for adverse events in intensive care.
RESULTS AND DISCUSSION
Indicators of healthcare quality in intensive care
A total of 31 AE were reported. The types of event found and their impact are shown in Table 1.
TABLE 1:
Distribution of reports of adverse events, according to the nature and incidence in adult ICU. Florianópolis, SC, 2012.
The night shift had the larger number of AE reports, with 12 (39%) records, followed by the morning shift with 11 (35%) reports and the afternoon shift with 8 (26%) events. So the afternoon shift was considered the safest.
It is noteworthy that in this ICU there is the same number of professionals working in all shifts, but the largest quantity of procedures is performed in the morning shift, such as: bed bath, laboratory and imaging tests. Importantly, although the night and morning shifts had presented greater risks, professionals of these shifts were the ones who most performed records of notifications, which reinforces the commitment of seeking to improve quality of care.
Risks for adverse events in intensive care
Data were obtained through observations of patients at risk of suffering any of the AE studied. Observations were carried out for 30 consecutive days, in the three work shifts (morning, afternoon and evening), corresponding to 102 observations, and a total of 65 patients observed. In 29 of the 102 observations we identified more than one risk for AE. So, there were a total of 137 risks recorded: 74 (54%) for pressure ulcer development, 32 (23.4%) for loss of gastroenteral tube, 22 for (16%) loss of central venous catheter and 9 (6.6%) for accidental extubation. Study patients were at high risk for pressure ulcer development as well as for loss of gastroenteral tube.
The AE reported, with the main causes identified by the ICU professionals and the risks for the occurrence of AE perceived in the observations are analyzed below.
Pressure ulcer
For pressure ulcer development, we identified as causes: impaired physical mobility - 8 (26.7%); unprotected bony prominences - 7 (23.3%); changes in nutrition - 6 (20%); sensory deficit - 6 (20%); patient without highly specific foam mattress - 2 (6.7%); and failure to perform the decubitus change - 1 (3.3%).
The risk for pressure ulcer development was evaluated according to the Braden Scale, which classifies the risks for this AE as: high, medium and low. Figure 1 shows what was verified at the adult ICU.
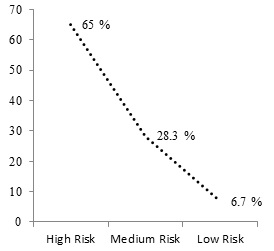
FIGURE 1:
Risk for pressure ulcers, according to Braden Scale in adult ICU. Florianópolis - SC, 2012
Also regarding pressure ulcer, we analyzed the most at risk areas, which are: calcaneal - 27 (36%), sacral - 26 (35.5%), occipital - 13 (18.4%), trochanteric- 4 (5%), malleolar - 3 (4.6%) and other region - 1 (0,5%).
Pressure ulcer in this study was a relevant AE, and the application of the Braden Scale showed that most of the patients had high risk for developing it, as shown in Figure 1. Regarding the location of pressure ulcers, there was predominance in calcaneal and sacral regions, corroborating other studies 23.
The diagnosis of risk for developing a pressure ulcer in a patient must take into consideration the various factors that predispose its formation 24, such as pressure, shear, friction, moisture, poor personal hygiene, improper positioning of the patient and deficiency in changing positions, among others 25.
Among the essential nursing actions to prevent the development of pressure ulcers, we can cite: the mobilization and proper repositioning of the patient every two hours and this changing positions can be intensified according to the patient's risk score, the skin care through the use of appropriate hygiene techniques, the use of mattresses that redistribute pressure on bony prominences, indicating and monitoring of nutritional conditions and fluid intake, etc.24.
Nurses should assess patients and plan care, considering the risk of developing ulcers and the prevention of it by implementing continuous and dynamic measures2, based on scientific evidence26.
Loss of gastroenteral tube
Regarding loss of gastroenteral tube, the following causes were identified: motor restlessness - 10 (25%); inadequate retention of the patient - 10 (25%); confusion - 9 (22.5%); patient handling during procedures - 4 (10%); unidentified - 2 (5%); inadequate fixation of the tube - 1 (2,5%); transfer stretcher/bed, stretcher/chair- 1 (2.5%); tube obstruction - 1 (2,5%); excessive sweating - 1 (2.5%) and; another condition - 1 (2.5%). The cause identified as another condition refers to a situation in which the patient lost the device during changing the endotracheal tube, as the tube was fixed along with that tube.
In most patients more than one risk for loss of gastroenteral tube were identified, and these were: inadequate fixation of the tube - 19 (45.2%); motor restlessness - 6 (14.2%); excessive sweating - 5 (12%); confusion - 4 (9.6%); inadequate retention of the patient - 3 (7%); administration of medication - 2 (4,8%); other condition - 2 (4.8%) and; tube obstruction - 1 (2.4%). Factors that appeared as another condition were: tube traction device and badly positioned tube.
Accidental removal of gastroenteral tube occurs primarily by the patient, by the professional during the conduction of procedures and/or inadequate fixation, tube obstruction and confusion of the patient27. When the patient is unsettled or presenting mental confusion, it is reinforced the use of immobilizers of arms for the patient's physical restraint, if appropriate28.
The exchange of gastroenteral tube fixation is also another fundamental care to avoid loss of this device. It should be performed whenever the tube is loose or dirty, preventing its displacement or removal, promoting health and preventing further damage to the patient2. However, as noted, some patients have excessive sweating, making it difficult to fix the tube and led to the increased nursing supervision for these cases. It is noteworthy in this study that tube obstruction only had one record as risk for loss of gastroenteral tube. The attention of the nursing team before this care is essential, thus preventing the loss of this device.
Loss of central venous catheter
The following problems that lead to loss of central venous catheters were identified: dressing with inadequate fixation - 1 (20%); catheter traction - 1 (20%); inadequate retention of the patient – 1 (20%); patient handling during procedures - 1 (20%) and; excessive sweating - 1 (20%).
As for the identified risk factors, there was more than one risk for the same patient; they were: dressing with inadequate fixation - 10 (40%); another condition - 8 (32%); catheter traction - 2 (8%); inadequate retention of the patient - 2 (8%); excessive sweating - 2 (8%) and; tube obstruction - 1 (4%). The risk factor presented as another condition was excess of cannulas coupled to the catheter, which contributed to its traction.
The incidence of loss of central venous catheter in the study site was low, which can demonstrate the care and attention of the staff to prevent the loss of this device. Studies address the accidental loss of central venous catheter as AE7,20, but do not specify the cause, except for one study, that pointed out as cause the obstruction of the catheter29, which was also found in this study as a risk factor.
Accidental extubation
Professionals identified the following causes for the occurrence of accidental extubation: inadequate retention of the patient 2 - (33.2%); agitation/confusion of the patient 1 - (16.7%); superficial sedation 1 - (16.7%); patient handling during procedures 1 - (16.7%); and inadequate fixation of the endotracheal tube / tracheostomy 1 - (16.7%).
In most patients we observed more than one risk factor for this AE, namely: agitation/confusion of the patient - 6 (37.5%); superficial sedation - 4 (25%); inadequate cuff pressure - 3 (18.75%); inadequate fixation of the endotracheal tube/tracheostomy - 2 (12.5%); and inadequate retention of the patient - 1 (6.25%). Even though accidental extubation occurred in lower incidence in the ICU studies, it is important to consider the complications that it causes the patient, because the occurrence of reintubation can increase mechanical ventilation time and bring serious consequences2. Absence of physical constraints, ratio nurse/patient of 1:3, transport for conduction of tests, superficial sedation and XR in the bed are mentioned as major risk factors for accidental extubation30 and some of these factors were identified in this study. In addition, accidental removal of nasogastric tube is also considered as a risk factor for unplanned extubation31. Another study conducted in intensive care stressed that auto-extubation represents the majority of cases of accidental extubation, where agitation, especially when combined with inadequate sedation and reduced surveillance to the patient is the main risk factors for the occurrence of this event. Inexperienced professionals and inadequate fixation of the tube may also be important, as the use of physical restraint remains controversial32,33.
Physical restraints are commonly used by health professionals to facilitate tolerance of care devices that cause discomfort and prevent premature or precipitate removal of such devices31,34. In recent years, the ethical debates have criticized the use of physical restraints without patient's consent31. Their use is controversial because the contentions may present an ethical dilemma, conflicting with human values and respectful care 34. It is important to limit the use of these devices for clinically appropriate situations, and only when alternative measures to reduce anxiety or agitation of the patient have failed31. Recommendations based on scientific evidence about methods to minimize the use of restraints on patients are still reduced34.
As for the inadequate fixation of the endotracheal tube, it increases the risk for accidental extubation. Standardizing a fixation method results in decreased occurrence of AE. It is also important to develop a screening tool for patients in mechanical ventilation that can identify those at greatest risk for accidental extubation31,34.
Inadequate cuff pressure, despite not having caused any accidental extubation in this study, appeared as a risk factor for this AE. The nursing and physical therapy professionals perform such care in this ICU; thus, we emphasize the importance of verifying the cuff pressure and keep it within normal limits not to cause harm to the patient and to prevent accidental extubation.
Since accidental extubation is an adverse event of care in many hospitals, we see the importance of systematization of nursing actions in effective prevention thereof during handling of critically ill patients, in various situations inherent in the process of care as well as the application of guidelines or protocols for a qualified care grounded on concepts that aim at patient safety35. In addition, identifying risk factors for accidental extubation and minimizing their incidence through prevention strategies are prerequisites for improving the quality of nursing care and patient safety in intensive care33.
CONCLUSION
With this study it was possible to identify the most common risks for the occurrence of AE, and to examine the quality indicators that were more incidents, which are: loss of gastroenteral tube and pressure ulcer development. The results showed the importance in monitoring the AE by applying quality indicators in order to improve safety and patient care. From that point, we reinforce the importance of acting before the problems in search of solutions that provide improvements to clinical practice and that strengthen patient safety in ICUs. It can include the adoption of best practices, based on scientific evidence, conducting training and continuing education to all professionals involved in the care process to the patient.
The study had some important limitations related to the reduced time of data collection and the small sample, which limit the generalization of findings.
REFERENCES
1.World Health Organization. World Alliance for Patient Safety. Summary of the evidence on patient safety: implications for research. The research priority setting working group of the world alliance for patient safety. Geneva: World Health Organization; 2008.
2.Venturi KK. Quality care in ICU: dimensioning nurses and adverse events ratio [dissertation]. Curitiba (PR): Federal University of Paraná; 2009.
3. Novaes AP. Indicators ICU. In: Padilha KG et al, organizers. Nursing in UCI: caring for critically ill patients. Sao Paulo: Manole; 2010.p.1312-21.
4.Organização Nacional de Acreditação[Internet website]. Meet the ONA. [quoted in Oct 10 2012] Available in: https://www.ona.org.br/Pagina/23/Historico.
5.Caldana G, Gabriel CS, Rocha FLR, Bernardes A, Françolin L, Costa DB. Evaluation of the quality of nursing care in private hospital. Rev. Eletr. Enf. 2013;15:915-22.
6.Joint Commission International. Accreditation standards of the Joint Commission International for hospitals. 3rd ed. Rio de Janeiro: Brazilian Accreditation Consortium; 2008.
7. Nascimento CCP, Toffoletto MC,Gonçalves LA, Freitas WG, Padilha KG. Indicators of care outcomes: analysis of adverse events during hospitalization. Rev Latino-Am Enfermagem. 2008; 16: 746-51.
8.Paiva MCMS, Paiva SAR, Berti HW. Adverse events: analysis of a reporting tool used in nursing management. Rev Esc Enferm USP. 2010; 44:287-94
9.Tronchin DMR, Melleiro MM, Takahashi RT. The quality and the evaluation of health and nursing services. In: Kurcgant P. coordinator. Nursing management. Rio de Janeiro: Guanabara Koogan; 2010. p.75-88.
10.Mendes W, Martins M, Rozenfeld S, Travassos C. The assessment of adverse events in hospitals in Brazil. Int J Qual Health Care. 2009; 21:279-84.
11.Pelliciotti JSS, Kimura M. Medication errors and quality of life related to health of nurses in intensive care units. Rev Latino-Am Enfermagem. 2010; 18(6):1062-9.
12.Claro CM, Krocockz DV, Toffolleto MC, Padilha KG. Adverse events at the Intensive Care Unit: nurses' perception about the culture of no-punishment. Rev esc enferm USP. 2011;45:167-72. 13.Frello AT, Carraro TE. Contributions from Florence Nightingale: an integrative review of the literature. Esc Anna Nery. 2013;17:573-9.
14.World Health Organization. Quality of care: patient safety [Internet website]. Report by the Secretariat of the 55th World Health Assembly. [citado em 16 mar 2015] Available in: http://apps.who.int/iris/bitstream/10665/20042/1/eeb11337.pdf?ua=1.
15.World Health Organization. World alliance for patient safety [Internet website]. WHO draft guidelines for adverse event reporting and learning systems. [quoted in Mar 01 2014] Available in: http://www.who.int/patientsafety/events/05/Reporting_Guidelines.pdf.
16.Agency for healthcare research and quality. Quality and Patient Safety [Internet website]. [quoted in Oct 11 2014]. Available in: http://www.ahrq.gov.
17.Paese F. Patient safety culture in primary health care [dissertation]. Florianópolis (SC): Federal University of Santa Catarina; 2010.
18. Ministry of Health (Br). Ordinance No. 538: recognizes the national accreditation organization as the competent institution and authorized to operate the development of hospital accreditation process in Brazil. Brasília (DF): Ministry of Health; 2001.
19.Agency for healthcare research and quality. AHRQ quality indicators: guide to patient safety indicators – version 3.1. 2007 [quoted in Mar 10 2015] Available in: http://www.qualityindicators.ahrq.gov/downloads/modules/psi/v31/psi_guide_v31.pdf .
20.Carneiro FS, Bezerra ALQ, Silva AEBC, Souza LP, Paranaguá TTB, Branquinho NCSS. Adverse events in the surgical clinic of a university hospital: quality assessment tool. Rev enferm UERJ. 2011; 19: 204-11.
21. Ministry of Health (Br). Resolution No. 196 of October 10, 1996: Approves the regulatory guidelines and standards for research involving human subjects. Brasília (DF): Ministry of Health; 1996.
22.Palhares VC, Palhares Neto AA. Prevalence and incidence of pressure ulcers in a intensive care unit. Rev enferm UFPE online.2014;8:3647-53.
23.Rogenski NMB, Kurcgant P. Incidence of pressure ulcers after implementing a protocol prevention. Rev Latino-Am Enfermagem. 2012; 20:333-9.
24.Silva EWNL, Araujo RA, Oliveira EC, Falcão VTFL. Applicability of pressure ulcer prevention protocol in intensive care unit. Rev bras ter intensiva. 2010; 22:175-85.
25.Bereta RP, Zborowski IP, Simão CMF, Anselmo M, Ribeiro S, Magnani LAFN. Clinical protocol for pressure ulcer prevention in critical customers. CuidArte Enferm. 2010; 4:80-6.
26.National Guideline Clearinghouse [Internet website]. Preventing pressure ulcers and skin tears. In: Evidence-based geriatric nursing protocols for best practice [quoted in Mar 15 2015]. Available in: http://www.guideline.gov/content.aspx?id=43935 .
27.Linford L, McGinnis C. Enteral tube dislodgement prevention an recognition. Perspectives. 2011; 9: 2-7.
28.Santos VFR, Figueiredo AEPL. Intervention and activities proposed for the diagnosis of impaired spontaneous nursing-ventilation. Rev Acta Paul Enferm. 2010;23:824-30.
29.Gabriel CS, Melo MRAC, Rocha FLR, Bernardes A, Miguelaci T, Silva MLP. Performance indicators used in public hospital nursing service. Rev Latino-Am Enfermagem. 2011;19: 1247-54.
30.Tanios MA, Epstein SK, Livelo J, Teres D. Can we identify patients at high risk for unplanned extubation? A large-scale multidisciplinary survey. Respir Care. 2010; 55: 561-8.
31.King JN, Elliott VA. Self/unplanned extubation: safety, surveillance, and monitoring of the mechanically ventilated patient. Crit Care Nurs Clin North Am. 2012; 24: 469-79.
32.Ismaeil MF, El-Shahat HM, El-Gammal MS, Abbas AM. Unplanned versus planned extubation in respiratory intensive care unit, predictors of outcome. Egyptian Journal of Chest Diseases and Tuberculosis. 2013; 63: 219-31.
33.Kiekkas P, Aretha D, Panteli E, Baltopoulos GI, Filos KS. Unplanned extubation in critically ill adults: clinical review. Nursing in Critical Care. 2013; 18: 123-34.
34.Luk E, Sneyers B, Rose L, Perreault MM, Williamson DR, Mehta S, et al. Predictors of physical restraint use in Canadian intensive care units. Crit Care. 2014;18.
35.Ramalho JMN, Nascimento LB, Silva GNS, Menezes MS, Nóbrega MML. Accidental extubation and intensive nursing care. Rev enferm UFPE on line. 2014;8:3945-52.