RESEARCH ARTICLES
Perineal lacerations location in vaginal birth among primiparous women
Adriana de Souza CarociI; Maria Luiza Gonzalez RiescoII; Jaqueline Sousa LeiteIII; Natalúcia Matos AraújoIV; Leila Barreto ScarabottV; Sonia Maria Junqueira Vasconcellos de OliveiraVI
IObstetric Nurse. PhD in Nursing. PhD Professor of the Obstetric Couse of the School of Arts, Sciences and Humanities of São Paulo University. Brazil. E-mail: acaroci@usp.br.ABSTRACT: Cross-sectional study, aiming to analyze the distribution of vulvo-perineal lacerations and factors related to its location in the anterior and posterior region of perineum in spontaneous birth. The sample had 317 women who had vaginal delivery without episiotomy and with perineal laceration. Data were collected in two centers of normal birth, in the cities of São Paulo and Itapecerica da Serra, São Paulo State, from 2001 to 2012, and takes part of the database of five sub-projects linked to the project Perineal trauma in normal birth: prevention, morbidity and care. There was predominance of lacerations in the posterior perineum region. There was no statistically significant difference in relation to the location of the perineal laceration and the maternal position during delivery, variety of fetal position in the cephalic presentation, circular umbilical cord and weight of the newborn, but there was significant difference concerning to the kind of pushing.
Keywords: Delivery; perineum; lacerations; obstetric nurse.
INTRODUCTION
There are few women who remain with the perineum intact after a normal childbirth, because most of them undergo to episiotomy or had espontaneous perineal lacerations1.
Problems like pain and Dyspareunia are frequently reported postpartum morbidities resulting from perineal trauma2.
Data from the National Research of Demography and Health allow estimating that, in the first half of the decade of 2000, 71.6% of normal births in Brazil were with episiotomy3.
Among the 6,365 childbirth occurring in the General Hospital of Itapecerica da Serra, São Paulo, between 1999 and 2001, the perineal trauma were in 71.4% of cases (45.5% of spontaneous lacerations and 25.9% of episiotomies). Among primiparas without episiotomy, 50.2% of them had first-degree lacerations and 20% second degree. Parity, gestational age, vitality and weight of the newborn (NB) showed association with the perineal outcome4.
Although several studies in Brazil and abroad regarding the prevalence and factors related to episiotomy, few researches are dedicated to analyze spontaneous perineal lacerations5.6.
The research conducted with 2,883 parturients, between 1995 and 1997, in Sweden, showed that among the 1,296, 34.8% of mothers had first-degree lacerations occurring more frequently in the posterior region of the perineum, followed by the lacerations of labia minora, vestibule and clitoris. The second degree lacerations occurred in 38.5% of primiparous women and distributed on the median line and the left or right side of the posterior perineal region. In addition to the evaluation of the degree and the size of laceration, the study proposes a ranking model, considering the location, the size and shape of the trauma7.
No Brasil, alguns estudos têm descrito a localização das lacerações, porém os fatores e morbidades relacionados à sua distribuição na região vulvo-perineal têm sido pouco analisados6,8-11.
In Brazil, some studies have described the location of lacerations. However the factors and co-morbidities related to its distribution in the vulvo-perineal region have been little analyzed6.8-11.
The objective of the present study was to analyze the distribution of the lacerations in the vulvo-perineal and factors related to its location in the anterior and posterior regions of the perineum in natural childbirth.
LITERATURE REVIEW
The perineum is a losenge area, whose transverse line divides into two triangular regions – anterior and posterior. The anterior region contains the external genitalia, including the major and minor labia, the vaginal vestibule and clitoris, forming the vulva. The posterior region contains the anus. A set of superficial and deep muscles participates in the structures of the perineum. In vaginal birth, during detachment of fetal presentation, these muscle formations if distend, in synergy with the vagina, forming a membranous canal, with a continuity solutions12.
Therefore, the location of lacerations is variable. Those that occur in the previous region of the perineum, labia and clitoris involve vestibular region, while in the posterior region, may reach the vaginal wall, the furcula and the perineal and anal muscles. In general, the lacerations in the previous region are associated with less morbidity and less need for suturing, while in the posterior region occur more complications such as hematoma, fistula and anal sphincter injuries and rectal mucosa. The lacerations in the posterior region are more frequent when the episiotomy is adopted as routine, while their restricted use increases the risk of previous injuries13.
In relation to the depth and the affected tissues, the first-degree lacerations reach only the skin or the mucosa; in second degree, muscle bundles also suffer some solution of continuity. When the laceration reaches the anal sphincter, it is considered of third degree; in case of injury involving rectal mucosa, it is considered of fourth degree14.15.
To describe the first and second degree lacerations, a model that divides the vulvo-perineal region was identified in the literature in three parts, matching the location, size and shape of the laceration. To the lacerations on lips and clitoris, the model presents five schemes, to the perineum, features four schemas and for vagina, also four schemas7.
Another model, more frequently, consider the location in the previous region (clitoris, labia minora and vestibular region left or right) and the posterior region (furcula, midline, left or right side and vaginal wall). As for the degree, the lacerations in the previous region are considered exclusively of first degree, while in the posterior region can vary from first to fourth grades6.8-11.
With regard to clinical implications of the degree and location of perineal trauma, it should be emphasized that the lacerations in the vaginal wall are infrequent, but can pass unnoticed who attends the delivery, by the difficulty of viewing. In the previous region, the lacerations are more shallow, rapid healing, but produce discomfort such as burning on urination. In the posterior region of the perineum, the short and long-term implications such as pain and healing problems, are related to the depth, the affected tissues and blood loss6.
METHODOLOGY
It is a cross-sectional study on the location of perineal lacerations in natural childbirth in women without episiotomy, that met the following criteria: without previous vaginal birth; single-term gestation, with fetus alive in cephalic presentation bent; left side position or birth semi-seated, assisted by obstetric nurse research team without epidural or spinal anaesthesia.
The sample was obtained from the database of five sub-projects6.16-19, linked to the project Perineal trauma in natural childbirth: prevention, morbidity and care, considering the inclusion criteria standardized across all subprojects.
The data were collected in two centers of natural childbirth (CPN) – Amparo Maternal (AM), in the capital of São Paulo, and General Hospital of Itapecerica da Serra (HGIS) in the State of São Paulo in Brazil. The AM is a philanthropic institution, maintained by the Unified Health System (SUS), under management of Santa Catarina Congregation, since 2009. In 2010, the monthly average of births was 580, with 77% of normal deliveries. The normal NBs remain in observation at a nursery unit for about three hours. After evaluation of the doctor neonatologist, the NBs are referred to by their mothers in the housing center (HC). The HGIS belongs to the State Government of São Paulo and is administered by the Social Organization of Health Social Services and Construction Industry of Furniture of São Paulo State-SECONCI. In 2001, the monthly average of births was 403, with 71% of normal deliveries. It works as a reference for the municipalities of Itapecerica da Serra, Juquitiba, Embu-Guaçu and São Lourenço da Serra. The NBs without problems stay with their mother in HC, since birth.
On both services, the childbirth without dystocia are performed by obstetric nurses in CPN, located in the immediate areas, but separated from the birth center. The obstetricians are responsible for the parturient women hospitalization, watch the operative and dystocia birth and evaluate complications detected by obstetric nurses. These services seek to follow the recommendations of the Ministry of Health of Brasil1 during labour and delivery, suppressing the episiotomy, shaving, enema, and intravenous infusion of oxytocin as routine. It is encourages freedom of movement and position of parturient, besides enabling the choice of an carer during labor, delivery and postpartum. The diet is free and non-invasive methods and not for pharmacological pain relief are used. It is observed and stimulates the mother-child interaction in the first half hour of life, starting breastfeeding at that moement, when there are no contraindications.
The data were collected by researchers and by obstetric nurses participating in the research team, from June 2001 to January 2012. Immediately after each birth, the data collection instrument was completed, elaborated and tested for the study. During the pre-test, it was possible to note the acceptance of nurses participants and validate the data collection instrument.
Prior to data collection, the researchers reviewed with obstetric nurses, individually, the possible locations and degrees of perineal laceration14, aiming at standardization of information.
The dependent variable was the location of the perineal laceration. To identify its location, a drawing with the detailing of the regions of the perineum was used, which was reproduced in the form of data collection, considering: the previous region -clitoris; small left and right lip; vestibule left and right; the posterior region – the left and right side midline, wishbone and vaginal wall.
Independent variables were considered: maternal position in childbirth; pull type; variety of position in the cephalic presentation; circular of umbilical cord; weight of the NB.
The data was stored in a database of Excel application and descriptive and inferential statistical analysis were performed. The Chi-square test in two-tailed form, assuming the likelihood of error of the first kind of 5% (value of p < 0.05) was performed.
The research was approved by the Ethics Committee in Research (ECR) of SECONCI (Process s/nº/2001/CEP-SECONCI-SP), of the University Hospital of the São Paulo University (USP) (case 261/02/CEP-HU) and the School of Nursing of the São Paulo University (cases 265/2002/CEP-EEUSP; 654/2007/CEP-EEUSP; 1066/2011/CEP-EEUSP), because the AM has no ZIP CODE. According to ethical principles, the Term of Free and Informed Consent has been obtained in writing of all women; the participation was voluntary, and entirely ensured the right of exclusion from the study at any time.
RESULTS AND DISCUSSION
In the study 317 Primiparous Women participated, who met the criteria for inclusion.
With respect to women, the average age was 21.5 years old (dp=4.4), with minimum of 15 and maximum of 37 years old. Women considered white skin predominated the study -108 (34.1%), followed by the Mullato - 89 (28.1%), black - 42 (13.2%) and Indian - 21 (6.6%) in 57 (18%) cases, this data was not collected.
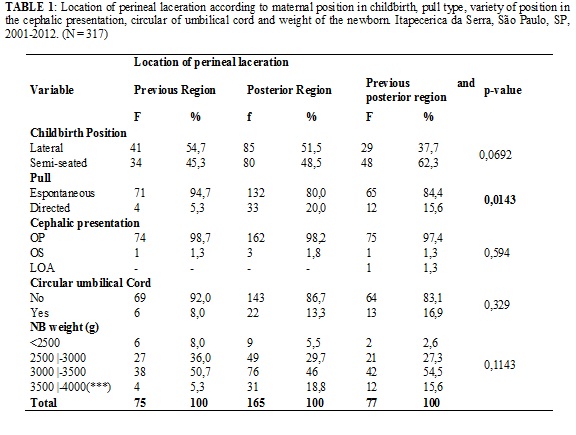
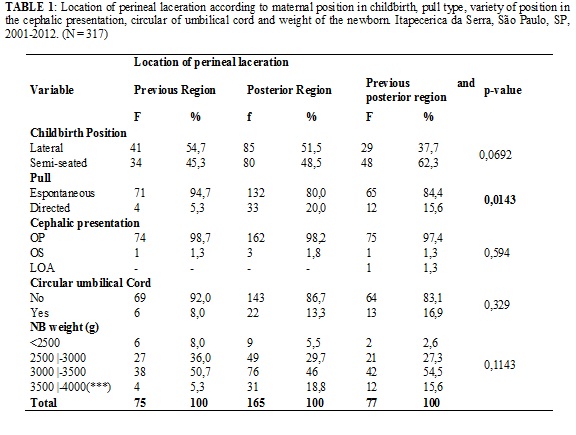
The results indicate that there is no statistically significant difference between the location of perineal laceration and maternal position in childbirth (p = 0.0692), the variety of position in the cephalic presentation (p = 0.594), the presence of circular of umbilical cord (p = 0.329) and the weight of the NB (p = 0.1143), as shown in Table 1.
However, the location of the laceration and the pull type used are not independent, as the value of p = 0.0143, verified by analysis of Chi-square. Among the 268 (84.5%) women who had spontaneous pull, there was a greater number of perineal lacerations than expected in previous region and fewer than expected in the posterior region. The reverse situation occurred for the pull directed, as less lacerations was observed than expected in the previous and more in the posterior region. Significant differences between observed and expected values were not detected for the lacerations that occurred in the previous and posterior perineal region, at the same time, both in births with pull spontaneous or with pull directed.
Since the pull directed was adopted in exceptional cases, there were more perineal lacerations when the pull spontaneous was used, compared to the use of pull directed (268 versus 49, respectively).
TABLE 1: Location of perineal laceration according to maternal position in childbirth, pull type, variety of position in the cephalic presentation, circular of umbilical cord and weight of the newborn. Itapecerica da Serra, São Paulo, SP, 2001-2012. (N = 317)
The first degree perineal lacerations, according to their location in the previous and posterior region of the perineum, are described below. It is worth noting that the total number of perineal lacerations is higher than the number of women who were part of the study, because some had more of a perineal laceration. Thus, among the lacerations of the first degree (354), the previous region predominated (190), distributed in the vestibule (101), labia minora (82) and clitoris (7).
The second degree perineal lacerations are entirely located in the posterior region (left and right side midline, wishbone and vaginal wall). There were 109 second degree lacerations, distributed in the midline and wishbone (92) and left and right side (17).
There are few studies that address the location of perineal lacerations and when this is considered, the main focus is the degree of trauma and the results are analyzed together. In general, research seek evidence related to the following factors that may interfere in the conditions of perineum: delivery location; professional who provides assistance; maternal education; parity; previous perineal scar; infusion of oxytocin, lithotomy position; duration of second stage of labor; pulls directed; perineal protection maneuvers; weight and cephalic perimeter of NB6.7.11.20-22.
The literature also points out, the episiotomy as a factor related to the location and degree of perineal laceration. Randomized controlled and conducted study in eight Argentina's public maternities, with 2,606 women, found that the previous perineal trauma was more frequent in the group with use of selective episiotomy (19.2% versus 8.1% in the group with routine use of episiotomy), while the perineal laceration in the posterior region occurred more in the group with the use of routine episiotomy (88.1% versus 63.1% in the group with the selective use)23.
Although the institutions where this research was performed this procedure is practiced so restricted and only women not undergoing episiotomy have been included, the results differ from both studies, because there was a predominance of lacerations in the posterior region of the perineum (52% in the posterior region, exclusively, and 24.3% in both regions).
Results of research conducted in two hospitals in England, with 5,404 women, indicated a variety of combinations in relation to the location of multiple lacerations in the regular birth. The main locations were in the posterior region of the perineum (50.4%) in the region, the lacerations occurred in labia minora (35.4%) vaginal wall (11%) and clitoris (1.4%). Some lacerations reach the urethra and cervix, most births was semi-seated and sitting positions, the occurrence of episiotomy was 11.1%, the first and second degree lacerations occurred at 66.3% and the third and fourth degrees occurred in 1.4% of women24.
In a study already cited, a model that divides the vulvo-perineal region in four segments, combining location, grade, size and shape of the laceration was used to characterize the perineal trauma. The model presents five schemes to the lacerations on my lips and clitoris and twelve schemes to the posterior perineal region, vagina and anal sphincter, four for each segment. The first-degree lacerations were distributed in the labia minora (included the vestibule), vaginal wall (including wishbone) and clitoris and 33.5% advance, 27.7% and 5.4% of the mothers, respectively. In the posterior perineal, predominated the second-degree lacerations in the midline, which occurred in 36.4% of Primiparous7.
In the present study, also, predominated the lacerations in the posterior region of the perineum (76.3% of women, including those with exclusively lacerations in the posterior region and those with previous and posterior trauma), located mainly in the midline and wishbone.
It is worth noting that the lacerations in the posterior perineum include the vaginal wall and the anal sphincter and this location can hinder the identification of the trauma. It is therefore important that the anal sphincter and the birth canal are inspected carefully, even when the injury is not readily visible6.
In relation to previous region perineal lacerations that occurred in 48% of women, there was a predominance of those located in the vestibule. Although only four women have suffered a laceration clitoris, this place deserves care because it is a very sensitive area and vascularized, and can cause pain and bleeding, both during the suture and the puerperium. In this sense, the repair of lacerations on the previous region requires professional skill and use delicate material, i.e. smaller needles and malleable yarn, of smaller calibre.
Research carried out in a university hospital in Austria, with 1,076 women with vaginal birth, obtained 28% frequency of episiotomies and lacerations of first, second and third degrees in 36.2%, 28.4% and 3.6%, respectively. As for the location, 15.4% of lacerations occurred in the vagina and 20.7% in the lips. The primiparity, absence of episiotomy, larger diameter of the fetal head and the supine position increased the risk of perineal trauma25.
Unlike the results of this study, research conducted in Itapecerica da Serra, SP, with 158 nulliparous compared labor at left side position and semi-seated and obtained advantages with the lateral position in relation to the degree of perineal trauma. The results showed that there were fewer women with episiotomies and more with first degree lacerations (p = 0.031). In relation to the location, the position at birth showed no difference for the paraurethral lacerations, vaginal, on wishbone and perineal body; the only statistically significant difference was observed in the lacerations that occurred in the labia minora (37% in the lateral decubitus and 19.5% in semi-seated; p = 0.015)26.
The variety of position in the cephalic presentation, circular of umbilical cord and weight of NB are analyzed in the literature only in relation to the occurrence and degree of perineal laceration and were not obtained studies that relate these variables to their location. Studies show that the higher weight at birth may increase the frequency and severity of perineal trauma27-29.
As the results show, the lacerations on the previous of the perineum were more frequent among women who underwent spontaneous pull, while those who held the pull directed had more lacerations in the posterior region (p = 0.0143).
Research carried out in a hospital in São Paulo, with 156 mothers with vaginal delivery, identified that the pull was a spontaneous perineal protection factor. Of the 103 women who have that kind of pull, only 26% presented perineal trauma; and 53 women with pull directed, 49% had perineal trauma of second or third degree30.
Study in the USA, with 1,176 women, showed the increased risk of perineal trauma among young first-time mothers who performed on fetal expulsion directed pull (RR = 1.65; 95% CI 1.05 -2.59)31, as well as in the study with 39primiparous, which indicated greater probability of perineal trauma with that kind of pull (92.9% versus 45.5%, respectively) (p < 0.05)32. On the other hand, systematic review of randomized studies comparing the pull directed and spontaneous, during the second period of childbirth, concluded that there was no statistically significant difference in relation to the frequency and severity of perineal trauma33.
CONCLUSION
In view of the results obtained, there were more lacarations in the posterior region of the perineum than on previous region. Perineal laceration's location was not related to the maternal position in childbirth, variety of position in the cephalic presentation, circular of umbilical cord and weight of the NB, but it was related to the type of pull.
There are variations in the classification of conditions of the perineum during childbirth and in the description of the location of perineal lacerations suggesting, therefore, studies and recommendations for their standardization.
As limitation of the present study, it can be considered the impossibility to classify separately those lacerations located the vaginal wall, because that information was not specified in all subprojects. Therefore, the laceration that occurred in the vaginal wall is grouped with those located in the posterior region of the perineum. Also, the lack of a standardized classification between studies to identify the different locations of the lacerations complicates the comparison of the results.
In this sense, as implications for the practice of obstetric nursing and to further research, it is suggested the proposal of a classification model of location of perineal trauma at normal birth.
REFERENCES
1. Brasil. Ministério da Saúde (Br). Secretaria de Políticas de Saúde. Área Técnica de Saúde da Mulher. Parto, aborto e puerpério: assistência humanizada à mulher. Brasília (DF): Editora MS; 2003.
2. Silva NLS, Oliveira SMJV, Silva FMB, Santos JO. Dispareunia, dor perineal e cicatrização após episiotomia. Rev Enferm UERJ. 2013;21: 216-20.
3. Lago TDG, Lima LP. Assistência à gestação, ao parto e ao puerpério: diferenciais regionais e desigualdades socioeconômicas. In: Ministério da Saúde (Br). Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher - PNDS 2006: dimensões do processo reprodutivo e da saúde da criança [Internet]. Brasília; 2009. [citado 28 jan 2013]. Available at: http://bvsms.saude.gov.br/bvs/publicacoes/pnds_crianca_mulher.pdf
4. Riesco MLG, Costa ASC, Almeida SFS, Basile ALO, Oliveira SMJV. Episiotomia, laceração e integridade perineal em partos normais: análise de fatores associados. Rev enferm UERJ. 2011; 19:77-83.
5. Colacioppo PM, Riesco MLG, Colacioppo RC, Osava RH. Avaliação do viés de classificação da laceração perineal no parto normal. Acta Paul Enferm. 2011; 24:61-6.
6. Leite JS. Caracterização das lacerações perineais espontâneas no parto normal [dissertação de mestrado]. São Paulo: Universidade de São Paulo; 2012.
7. Samuelsson E, Ladfors L, Lindblom BG, Hagberg H. A prospective observational study on tears during vaginal delivery: occurrences and risk factors. Acta Obstet Gynecol Scand. 2002; 81:44-9.
8. Costa ASC, Riesco MLG. A comparison of “hands off” versus “hands on” techniques for decreasing perineal lacerations during birth. J Midwifery Womens Health. 2006; 51:106-11.
9. Scarabotto LB, Riesco MLG. Use of hyaluronidase to prevent perineal trauma during spontaneous delivery: a pilot study. J Midwifery Womens Health. 2008; 53:353-61.
10. Costa ASC, Riesco MLG, Oliveira SMJV, Schneck CA, Colacioppo PM. Laceração perineal no manejo ativo versus manejo expectante do feto durante o nascimento. Rev Paul Enfermagem. 2007; 26:17-24.
11. Araújo NM, Oliveira SMJV. The use of liquid petroleum jelly in the prevention of perineal lacerations during birth. Rev Latino-Am Enfermagem. 2008; 16:375-81.
12. Rezende J. Obstetrícia. 9ª ed. Rio de Janeiro: Guanabara Koogan; 2007.
13. Carroli G, Mignini L. Episiotomy for vaginal birth (Cochrane Review). In: The Cochrane Library, Issue 1. Oxford: Update Software, 2012.
14. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GDV et al. Conduta no trabalho de parto e no parto normal. In: Williams obstetrícia. 20ª ed. Rio de Janeiro: Guanabara Koogan; 2000. p.281-98.
15. Kettle C. Anatomy of the pelvic floor. In: Henderson C, Bick D, editor. Perineal care: an international issue. Trowbridge: Quay; 2005. p.18-31.
16. Costa ASC. Proteção perineal e manejo do feto no parto normal: estudo comparativo entre duas técnicas [dissertação de mestrado]. São Paulo: Universidade de São Paulo; 2002.
17. Araújo NM. Uso de vaselina líquida na região perineal durante o parto normal [dissertação de mestrado]. São Paulo: Universidade de São Paulo; 2004.
18. Scarabotto LB. Uso da enzima hialuronidase na prevenção de lacerações perineais no parto normal [dissertação de mestrado]. São Paulo: Universidade de São Paulo; 2004.
19. Colacioppo PM. Uso da hialuronidase na prevenção do trauma perineal no parto normal: ensaio clínico aleatório placebo-controlado duplo-cego [tese de doutorado]. São Paulo: Universidade de São Paulo; 2009.
20. Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy and Childbirth. 2013;13(1):59.
21. Hodnett ED, Downe S, Walsh D. Alternative versus conventional institutional settings for birth (Cochrane Review). In: The Cochrane Library, Issue 8.Oxford: Update Software. 2012.
22. Kopas ML. A review of evidence-based practices for management of the second stage of labor. J Midwifery Women’s Health. 2014; 59:264-76.
23. Argentine Episiotomy Trial Collaborative Group. Routine vs selective episiotomy: a randomized controlled trial. Lancet. 1993; 342:1517-8.
24. Albers L, Garcia J, Renfrew M, McCandlish R, Elbourne D. Distribution of genital tract trauma in childbirth and related postnatal pain. Birth. 1999; 26(1): 11-7.
25. Mayerhofer K, Bodner-Adler B, Bodner K, Rabl M, Kaider A, Wagenbichler P, et al. Traditional care of the perineum during birth. J Reprod Med. 2002; 47:477-82.
26. Schirmer J, Fustinoni SM, Basile, ALO. Perineal outcomes on the left lateral versus vertical semi-sitting birth positions: a randomized study.Acta Paul Enferm. 2011; 24:745-50.
27. Hudelist G, Gelle'n J, Singer C, Ruecklinger E, Czerwenka K, Kandolf O, et al. Factors predicting severe perineal trauma during childbirth: role of forceps delivery routinely combined with mediolateral episiotomy. Am J Obstet Gynecol. 2005; 192:875-81.
28. Riesco MLG, Pereira FG, Colacioppo PM. Uso da anestesia local para episiotomia e reparo do trauma perineal no parto normal: práticas de enfermeiras e médicos. Nursing. 2006; 9:1158-63.
29. Silva FM, Oliveira SM, Bick D, Osava RH, Tuesta EF, Riesco ML. Risk factors for birth-related perineal trauma: a cross-sectional study in a birth centre. J Clin Nurs. 2012; 21:2209-18.
30. Colacioppo PM, Gonzalez RML, Koiffman MD. Use of hyaluronidase to prevent perineal trauma during spontaneous births: a randomized, placebo-controlled, double-blind, clinical trial. J Midwifery Womens Health. 2011; 56:436-45.
31. Albers LL, Sedler KD, Bedrick EJ, Teaf D, Peralta P. Factors related to genital trauma in normal spontaneous vaginal births. Birth. 2006; 33(2):94-100.
32. Sampselle CM, Hines S. Spontaneous pushing during birth relationship to perineal outcomes. J Nurse Midwifery. 1999; 44(1):36-9.
33. Yildirim G, Beji NK. Effects of pushing techniques in birth on mother and fetus: a randomized study. Birth. 2008; 35(1):25-30.