RESEARCH ARTICLES
Health professionals' knowledge regarding adverse events in the intensive care unit
Isadora Alves MoreiraI; Ana Lúcia Queiroz BezerraII; Thatianny Tanferri de Brito ParanaguáIII; Ana Elisa Bauer de Camargo SilvaIV; Francino Machado de Azevedo FilhoV
I
Nurse at the University Hospital of Brasilia, Brazil. E-mail: isadora.a.moreira@gmail.com
II
Associate Professor of Nursing School of the Federal University of Goiás. Brazil. E-mail: analuciaqueiroz@uol.com.br
III
Professor of Faculty of Health Sciences at the University of Brasilia. Brazil. E-mail: ttb.paranagua@gmail.com
IV
Professor of the Nursing School of the Federal University of Goiás. Brazil. E-mail: anaelisa@terra.com.br
V
PhD student of the Post-graduate Program in Nursing at the University of Brasilia. Brazil. E-mail: francino21@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.5158
ABSTRACT
This descriptive study to examine health professionals' knowledge of adverse events occurring in intensive care units was conducted with 37 health professionals from two intensive care units at a teaching hospital in Goiania, Goias State. Data were collected from January to March 2011 using a validated, structured instrument, and were treated with descriptive statistical analysis. Of the 37 health professionals, 45.9% were unaware of the significance of adverse events, but recognized them as part of the work process, and reported the occurrence of 152 events during their time working in the unit. Continuing professional development activities and service organization measures were suggested with a view to preventing adverse events. Health professionals should be encouraged to report adverse events, and educational actions should use simulation based on the practical healthcare context as a pathway to safe, quality care.
Keywords: Nursing; intensive care units; patient safety; iatrogenic disease.
INTRODUCTION
In health institutions, procedures involve certain risks that become aggravated in the presence of flaws in the structure and processes of care, making care unsafe and as a result, there is evidence of poor quality in patient care and the occurrence of incidents.
Among the types of incidents, adverse events (AEs) stand out for, necessarily, causing harm to the patient, resulting in significant impact on the health system, including patients, professionals and institutions1.
Although the search for safety in health care is a desire, the occurrence of AE is a reality, even in sectors that provide care to critically ill patients and that require high standard of quality, as in intensive care units (ICUs)2. Worldwide, it is estimated that the AE affect 10% of patients admitted to hospitals and may lead to a temporary weakness and even death 3.
The publication of the report of the Institute of Medicine, To error is human, 1999, showing that every year in the United States, about 98,000 patients die of preventable events during hospitalization4 increased scientific research on patient safety.
Whereas the reduction of the AE implies its understanding and subsequently the preparation of corrective and preventive strategies, promoting quality and safer care, this study aimed to analyze the knowledge of health professionals about the occurrence of adverse events in the intensive care units of a teaching hospital.
LITERATURE REVIEW
Adverse event is defined as injury or unintentional damage, as consequence of the care provided, resulting in temporary or permanent disability or impairment, prolongation of hospital stay or death. What characterizes the AE is the fact that the damage or injury was caused by the care provided and not by the evolution of the underlying disease5.
In ICU the occurrence of AE has special significance because it is a highly complex sector. The prevalence of AE in ICU of university hospitals in Ottawa is estimated at 20% and it is observed that for each five events, one is preventable6.
In Brazil, research shows that over a four-year period, 377 patients were victims of AE, of which 22.3% suffered two or more events, highlighting the need to establish protocols for control and prevention7.
In the Central West region of Brazil, the first studies conducted in the state of Goias showed the occurrence of adverse events related mainly to the medication process8-10.
Other frequently identified AE in ICU are related to failures in prevention and diagnosis of diseases, to the monitoring system and interpretation of monitors by professionals as well as to failures during indication, insertion, maintenance and removal of tubular devices 11.
Regarding nursing care, there is highlight for flaws in medication administration, monitoring of infusion pumps, misuse of materials and therapeutic and diagnostic devices, as well as failures in the nursing notes12.
Considering that the nursing staff totals the largest contingent of workers in hospitals, that the expectation of care provided in the ICU is to ensure the best result within the clinical condition and the severity of patients with the lowest complication rates resulting from procedures performed and that the range of quality of care requires adjustment and control of the processes and structure of the service, there is a need to investigate the perception of the multidisciplinary team that provides care to critical patients13.
From this perspective, knowing the AE enables the identification of latent failures at various stages of the care process, which contributes to the realization of strategies to reduce and intercept these failures, minimizing their impact and leading the professional to a safe practice 14.
METHODOLOGY
Descriptive study, developed in the medical and surgical ICUs of a university hospital in Central West region of Brazil. Currently, the ICU has physical capacity to 14 beds: six beds in the medical ICU and eight beds in the surgical ICU.
All professionals were invited to participate in the study, representing a population of 104, including doctors, nurses and nursing technicians. Professionals who were on leave during the data collection period and those who have not been found after three scheduled visits in ICU were excluded.
Data collection was performed with 37 professionals, from January to March 2011. We used the technique of interview guided by structured instrument, evaluated by experts and submitted to the pilot test.
The instrument consists of three parts. The first investigates characterization data of the participants: age, gender, professional category, time of education and of work (in the profession, institution and unit), working hours and shift work in the institution, employment relationships and continuing education. The second contains questions on knowledge of professionals about the AE, preventive measures and risk management at the unit. The third consists of the types of AE identified by professionals during work in the ICU, the consequences for the patient, clinical and administrative procedures adopted and knowledge of the patient/family about what happened.
The participants' reports were transcribed into a Microsoft Word document to form the corpus of analysis, identified by the letter I, followed by a cardinal number according to the sequence of interviews. Quantitative data were entered into the spreadsheet of Microsoft Excel program version 2007. Then, a descriptive statistical analysis of categorical variables and mean for continuous variables was carried out. Results were presented in tables and discussed based on the literature.
The ethical aspects follow the CNS Resolution 196/96 and the study is linked to the project Analysis of adverse event occurrences in a hospital in the Sentinel Network of Central West Region, under Protocol No. 064/2008.
RESULTS AND DISCUSSION
Characterization of professionals
The study included 37 professionals: 23 from medical ICU and 14 from surgical ICU. Those professionals who have not been found after three attempts were excluded from the study.
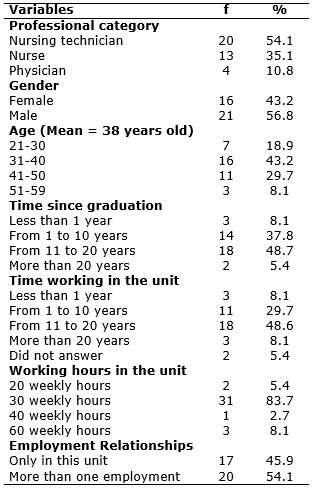
TABLE 1: Characterization of professionals from the medical and surgical ICU of a teaching hospital. Goiania, 2011. (N=37)
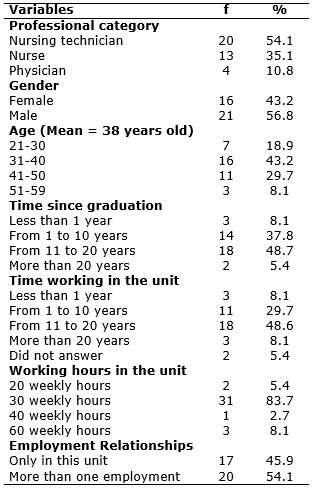
Among professionals, 20 (54.1%) were nursing technicians, followed by nurses with 13 (35.1%) and physicians with 4 (10.8%). Males predominated with 21 (62.2%) and age ranged from 21 to 59 years old, with prevalence of the age group from 31 to 40 years old, in 16 (43.2%) professionals.
The time since graduation was 11 to 20 years for 18 (48.6%) professionals and the time of work in the unit was over 11 years also for 18 (48.6%) workers. The weekly working hours in the unit for some professionals was from 20 to 60 hours and 20 (54%) professionals reported having more than one job.
Knowledge of professionals about adverse events
Professionals showed understanding of the meaning of AE, however, superficially, according to 17 (45.94%) reports, for example:
Something that happens out of the ordinary with the patient (I. 01)
Something occurred that is not foreseen for the patient (I. 16)
Ignorance or even erroneous knowledge was found in 20 (54.05%) of the reports, as an example:
Anything that occurs within the workplace (I.11)
I do not know (I. 09)
The limited knowledge of the professionals on AE highlights the need for management policies and development of strategic action aimed at continuing education of the multidisciplinary team to promote improvements in the quality and safety in the care process. Through in-service education, there is an understanding of the AE thereby facilitating the investigation of the quality of care and also an improvement in the service offered to the patient 12,15.
Investing in continuing education remains directly related to improving the performance of work and may assist in the prevention of AE 16. It should be noted also the importance of bringing to the attention of health professionals the results found in studies about AE, because the understanding of the etiology and of the hospital system contribution presents significant results17.
Reporting of adverse events
Regarding the reporting in the occurrence of AE, only 14 (37.83%) professionals said reporting verbally to the nurse or supervising doctor of the unit. However, none of the professional notifies the Risk Management Service and they do not have systematic guidance for reporting adverse events. However, the same professionals who verbally communicate the AE to the nurse or doctor reported recording the event in the medical record of the patient.
Recording is considered fundamental action in obtaining information of failures and enables the implementation of proactive measures to reduce the number of such occurrences18.
Notes in medical records or in information records of health services have significant value and are sources of research, education and legal documents, considered subject to evaluation of care provided to the patient and of quality of notes prepared by the multidisciplinary team. But it is important to encourage the systematic notification via a standardized instrument and, preferably, electronic, to facilitate and hasten the process of communication and analysis of events occurred19,20 .
Type of adverse events
During the work period in ICU 152 AE experienced by health professionals were reported. The types of AE are described in Table 2.
TABLE 2: Adverse events occurred in the medical and surgical ICU of a teaching hospital. Goiania, 2011.
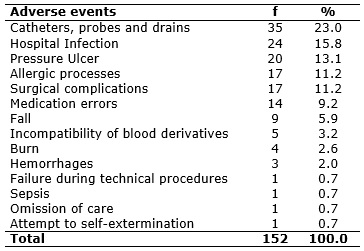
Of the total experienced EA, 35 (23%) were related to tubular devices, being a frequent event in literature10. Since intravenous therapy is one of the procedures most accomplished, insertion, maintenance and improper removal of these devices predisposes the occurrence of AE, being infection and blood extravasation the most frequent11,21. The causes of AE were 17 obstructions, 13 unscheduled removals of the device and five inadequate fixings.
Among the consequences, 14 required monitoring; 16 contributed to or resulted in temporary harm and prolonged hospitalization and four contributed to or resulted in temporary harm, requiring intervention.
Although it seems to be simple, the probing procedure is subject to severe complications, affecting the continuity of care22, just as the improper removal of drains can bring serious risks to the patient and should have careful evaluation by a qualified professional 23.
The decrease in AE related to tubular devices is associated to guidelines to the health team regarding the insertion and maintenance technique, care during transfer of the patient, in addition to guiding patients and families about the importance of maintaining the device 10.
Related to hospital infections, 24 (15.8%) AE were reported, 11 related to surgical site infection, four in post-probing bladder urinary tract, four bloodstream infections by vascular access, two infections at the insertion site of tubular devices, two pneumonias and one non-surgical wound infection.
As for the consequences for the patient, one required monitoring; 15 contributed to or resulted in temporary harm and required intervention, two resulted in permanent damage and prolonged hospitalization, one caused damage and required intervention necessary to sustain life and five resulted in deaths.
Hospital infection, besides prolonging the length of stay, brings serious consequences for the patient and high cost for the health system. Health care facilities should develop protocols of care to the patient, provide material resources and education to all staff to reduce the occurrence of hospital infection and to get better health indicators24.
There were 20 (13.1%) AE related to pressure ulcers that resulted in damage, prolonged hospitalization and required additional intervention to initial treatment.
Pressure ulcers stand out for being preventable events by adopting preventive measures such as monitoring, inspection and skin protection, as well as changing positions of the patient. Health professionals need to be aware of the problems that pressure ulcers can lead to the patient, the family and the hospital. These occurrences prolong hospitalization, hinder the recovery of the patient, increase the risk for developing complications and represent an increase in the physical and emotional suffering of clients by reducing their independence in carrying out the activities, and increase costs 25.
During the study period, 17 (11.2%) allergic processes were reported, of which 12 were related to drugs and five on the use of tape. Dipyrone was the medicine with most reports of allergic process, referring to six cases, followed by Vancomycin, with four. As a consequence of allergic processes, six required monitoring and 11 resulted in temporary harm with intervention.
It is of great importance to report allergic reactions to medical products for risk management service, as it is possible to manage these products by means of pharmacovigilance actions26,27 . These notifications have resulted in the monitoring and evaluation of these products, which contributes to the quality of care.
In surgical complications 17 (11.2%) cases were reported: 11 pneumothorax, four embolism/thromboembolism and one cardiac arrest.
Regarding the consequences, 13 required monitoring, three resulted in permanent damage and prolonged the hospital stay and one resulted in the death of the patient. To avoid complications arising from the estimate of 234 million surgeries performed each year, the World Alliance for Patient Safety has proposed the challenge Safe surgery save lives, which recommends the use of protocols to reduce perioperative morbidity and mortality related to such procedures3.
There were 14 (9.2%) drug-related EA, as shown in Table 3.
TABLE 3: Types of medication errors occurred in the medical and surgical ICU of a teaching hospital. Goiania, 2011.
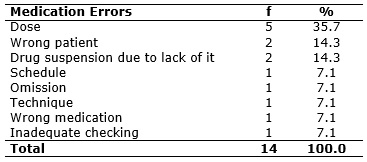
Among the events cited, 9 (64.2%) were related to the five right steps of medication administration (right patient, medication, dose, time and records) which shows that this simple verification process is not being followed. As for the consequences, nine required monitoring and five resulted in temporary harm with intervention.
It is estimated that at least 1.5 million people in the United States are affected by medication errors annually, generating costs of more than $ 3.5 billion3.
Health institutions shall draw up a drug insurance system to assist professionals in the prevention of errors, through measures that facilitate the medication process and hinder error occurrences28.
Professionals reported 9 (5.92%) falls from bed, including seven that required monitoring and two that resulted in temporary harm with intervention. See Table 2.
The fall of the patient is a frequent AE due to various factors such as the lack of necessary supervision and inefficient capacity of the patient to walk without assistance. Its occurrence can cause injuries and damage the physical and emotional integrity of the patient as well as the increase in hospital costs and even death29.
Several measures can be taken to prevent falls from occurring, such as lifting bars on the beds and the application of movement restriction techniques. The restraint in bed is an appropriate measure for agitated patients if carried out properly and does not cause damage and should be evaluated and monitored often by the team to determine whether to proceed with the procedure29.
There were 4 (2.6%) cases of burn, two related to the use of the defibrillator, one using hot compress and one related to electrocautery, as shown in Table 2. The consequences of these events have contributed to or resulted in temporary harm with intervention.
The burn leaves sequels in the injured area and, especially with hot compresses, occur due to professional's inattention to water temperature and exposure time in the patient's skin. Cases of burns related to equipment are also cited by several authors, and the cause must be investigated11,12 to support the development of bundles directed to procedures that may expose the patient to this risk. The bundles have been identified as impact measure that directs the adoption of safe practices and their use should be encouraged in environments that strive for excellence of care30.
There was report of 5 (3.2%) infusions of blood derivatives with blood incompatibility that required monitoring. For the transfusion practice, it is necessary that professionals are qualified and know all incidents related to the procedure, such as blood incompatibility, one of the most serious AE. In addition, documentation of information and clinical data of patient must be organized properly in order to optimize the service, to foreseen the possibility of incidents and also to introduce corrective measures and prevention of errors, which contributes to better safety in the transfusions of blood derivatives31.
Other events were reported, such as 3 (42.9%) hemorrhages, one (14.3%) technical failure during the procedure, one (14.3%) sepsis, one (14.28%) omission of care and one (14.3%) attempt to self-extermination. As for the consequences of these AE, three resulted in temporary harm with intervention, one required monitoring, one resulted in temporary harm with monitoring and two resulted in death.
It appears that the occurrence of AE in ICU is common to health professionals; however, the knowledge on the subject is limited, whereas the report of witnessing the incident is significant.
Approaches for adverse event
Regarding the conducts front the occurrence of AE, 130 (85.5%) resulted in simple measures such as observation and interventions with antibiotics, dressings, monitoring, drainage, drug suspension and use of antihistamine. There was not report of conducts for 22 (14.5%) AE. The communication of the AE to the patient occurred in 67 (44.1%) cases. Patient empowerment to ensure their own safety has been stimulated, and one of the actions includes the communication to the patient so that they assist in decision making, so that the consequences are minimized as best as possible 32.
Among the administrative conducts investigated in this study in relation to the professional involved in the AE, 21 (13.8%) occurrences resulted in verbal warning, clarification and guidance about the error reasons, communication to the supervisor and annotation on patient outcomes.
As managerial and educational conducts in the prevention of 42 (27.6%) AE, it was mentioned continuing education, supervision and guidance of the professional.
As for the existence of AE preventive measures adopted in the institution and in the ICUs, 16 (43.2%) professionals referred the conduction of courses and training with the Hospital Infection Control Committee, and 6 (27.3%) reported administrative measures such as protocol procedures and routines, guidance on flow, preparation and administration of medications among pharmacy and clinical units and the systematization of nursing care.
As suggestions to avoid AE, 23 (62.1%) cited the educational activities, of which 15 (40.5%) were related to the training, mentoring and continuing education and 8 (21.6%) to safety and attention of the professional. As for the service organization, 4 (10.8%) professionals suggested improvement in physical structure and in the information system/internal communication of the unit and institution.
The occurrence of AE interferes with patient safety and can be influenced by management of the service due to failures in the stages of planning, control and supervision of the work as for the demands on the forecast, provision and maintenance of equipment and material resources 33,34.
Knowing these aspects is relevant as a preventive measure, allowing each professional to identify and to evaluate risks as well as to promote collective awareness for safe care20.
Thus, authors emphasize that the practice of educational actions together with the professionals involved directly in care may encourage the improvement of quality care provided to the client and prevent the repetition of the error, developing therefore a safety culture18,35.
The support of the hospital management to patient safety is a necessary dimension to the transformation of care practice, which implies the need for a more proactive attitude on the part of managers and communication between different subsystems that make up the health services36. However, it is emphasized that patient safety should be the responsibility of all professionals involved in the care process, subsidized by development and professional training programs, with education as an essential practice for patient safety37.
CONCLUSION
It was found that professionals have superficial knowledge about the concept of AE, but identify and recognize the event as part of health care when it is not performed with quality.
It showed up underreporting of events in the context of practice and the existence of gaps in the institutional educational processes, demonstrating weaknesses in patient safety.
Authors suggest improvements in the management of work processes and of the organizational system, as well as promotion of foundations for the development of clinical evidence aimed at building knowledge and attitudes for the prevention of AE and promotion of safety culture. Being an environment where activities are complex, managers of ICUs should adopt policies aimed at systematic approach and learning from mistakes in order to train professionals to be proactive in face of the occurrence of events in order to reduce the consequences to the patient.
This study has limitations on the number of professionals, especially medical staff, as few agreed to participate. It is believed that the use of an online method for collecting information can expand the eligible population for future studies, and also support the development of a local information system to facilitate the compilation of the data, to encourage the records of AE by professionals and to assist decision making of managers.
REFERENCES
1.Oliveira RB. Eventos adversos com medicamentos favorecidos pelo sistema de medicação de um hospital público no município do Rio de Janeiro [dissertação de mestrado]. Rio de Janeiro: Universidade Federal do Estado do Rio de Janeiro; 2010.
2.Bohomol E, Ramos LH, D'Innocenzo M. Medication errors in an intensive care unit. J Adv Nurs. 2009;65:1259-67.
3.World Health Organization (WHO). World Alliance for Patient Safety. Global Patient Safety Challenge: 2006-2007. 2006 [cited in 2014 Apr 25] Available from: http://www.who.int/patientsafety/information_centre/WHO_EIP_HDS_PSP_2006.1.pdf.
4.Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system: National Academy Press; 2000.
5.World Health Organization (WHO). Conceptual framework for the International Classification for Patient Safety. Final Technical Report. Geneva, 2009 [cited 2015 Mar 08]. Available from: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf.
6.Forster AJ, Kyeremanteng K, Hooper J, Shojania KG, van Walraven C. The impact of adverse events in the intensive care unit on hospital mortality and length of stay. BMC Health Serv Res. 2008;8:259.
7.Toffoletto MC. Fatores associados aos eventos adversos em unidade de terapia intensiva [tese de doutorado] São Paulo: Universidade de São Paulo; 2008.
8.Silva AEBC, Reis AMM, Miasso AI, Santos JO, Cassiani SHDB. Adverse drug events in a sentinel hospital in the State of Goiás, Brazil. Rev Latino-Am Enfermagem. 2011;19:378-86.
9.Bezerra ALQ, Silva AEBC, Branquinho NCSS, Paranaguá TTB. Análise de queixas técnicas e eventos adversos notificados em um hospital sentinela. Rev enferm UERJ. 2009;17:467-72.
10.Carneiro FS, Bezerra ALQ, Silva AEBC, Souza LP, Paranaguá TTB, Branquinho NCSS. Eventos adversos na clínica cirúrgica de um hospital universitário: instrumento de avaliação da qualidade. Rev enferm UERJ. 2011;19:204-11.
11.Canineu R, Guimarães HP, Lopes RD, Vendrame LS, Fonseca Júnior MA, Lopes AC. Iatrogenia em medicina intensiva. Rev bras ter intensiva. 2006;18:95-8.
12.Beccaria LM, Pereira RAM, Contrin LM, Lobo SMA, Trajano DHL. Eventos adversos na assistência de enfermagem em uma unidade de terapia intensiva. Rev bras ter intensiva. 2009;21:276-82.
13.Belela ASC, Peterlini MAS, Pedreira MLG. Revelação da ocorrência de erro de medicação em unidade de cuidados intensivos pediátricos. Rev bras ter intensiva. 2010;22:257-63.
14.Chaboyer W, Thalib L, Foster M, Ball C, Richards B. Predictors of adverse events in patients after discharge from the intensive care unit. Am J Crit Care. 2008;17:255-63.
15.Vituri DW, Cacciari P, Gvozd R, Kuwabara CCT, Cardoso MGP. Indicadores de qualidade como estratégia para melhoria da qualidade do cuidado em um hospital universitário. Cien Cuid e Saúde. 2010;9(4):782-90.
16.Azevedo Filho FM, Martins IMS, Soares CSRS, Fazendeiro PG, Paranaguá TTB, Bezerra ALQ. Administración de medicamentos: conocimiento de los enfermeros del sector de urgencia y emergencia. Enferm glob. 2012;11:54-69.
17.Szekendi MK, Sullivan C, Bobb A, Feinglass J, Rooney D, Barnard C, et al. Active surveillance using electronic triggers to detect adverse events in hospitalized patients. Qua saf health care. 2006;15(3):184-90.
18.Claro CM, Krocockz DVC, Toffolleto MC, Padilha KG. Eventos adversos em Unidade de Terapia Intensiva: percepção dos enfermeiros sobre a cultura não punitiva. Rev Esc Enferm USP. 2011;45:167-72.
19.Paiva MCMS, Paiva SAR, Berti HW. Eventos adversos: análise de um instrumento de notificação utilizado no gerenciamento de enfermagem. Rev esc enferm USP. 2010;44:287-94.
20.Setz VG, D'Innocenzo M. Avaliação da qualidade dos registros de enfermagem no prontuário por meio da auditoria. Acta Paul Enferm. 2009;22:313-7.
21.Machado AF, Pedreira MLG, Chaud MN. Adverse events related to the use of peripheral intravenous catheters in children according to dressing regimens. Rev Latino-Am Enferm. 2008;16:362-7.
22.Nascimento CCP, Toffoletto MC, Gonçalves LA, Freitas WG, Padilha KG. Indicators of healthcare results: analysis of adverse events during hospital stays. Rev Latino-Am Enferm. 2008;16:746-51.
23.Parra AV, Amorim RC, Wigman SE, Baccaria LM. Retirada de dreno torácico em pós operatório de cirurgia cardíaca. Arq Ciênc Saúde. 2005;12(2):116-9.
24.Bezerra ALQ, Queiroz E, Weber J, Paranagua T. Reacciones adversas: indicadores de resultados según la percepción de las enfermeras de un hospital centinela. Enferm glob. 2012;11:186-97.
25.Silva RCL, Figueiredo NMA, Meirelles IB, organizadores. Feridas: fundamentos e atualizacoes em enfermagem. 3ª ed. São Caetano do Sul: Yendis; 2011.
26.Romeu GA, Távora MRF, Costa AKM, Souza MOB, Gondim APS. Notificacao de reacoes adversas em um hospital sentinela de Fortaleza - Ceara. R Bras Farm Hosp Serv Saúde São Paulo. 2011;2(1):5-9.
27.Organização Mundial da Saúde. Monitorização da segurança de medicamentos: diretrizes para criação e funcionamento de um Centro de Farmacovigilância. Brasília (DF): Organização Pan-Americana da Saúde, 2005.
28.Silva AEBC, Cassiani SHB. Erros de medicação em hospital universitário: tipo, causas, sugestões e providências. Rev bras enferm. 2004;57:671-4.
29.Santos JC, Ceolim MF. Iatrogenias de enfermagem em pacientes idosos hospitalizados. Rev esc enferm USP. 2009;43:810-7.
30.Shimabukuro PMS, Paulon P, Feldman LB. Implantação de bundles em unidade de terapia intensiva: um relato de experiência. Rev Enferm UFSM. 2014; 4(1):227-36.
31.Curcioli ACJV, Carvalho EC. Infusion of hematopoietic stem cells: types, characteristics, adverse and transfusion reactions and the implications for nursing. Rev Latino-Am Enferm. 2010;18:716-24.
32.Lyons M. Should patients have a role in patient safety? A safety engineering view. Qua saf health care. 2007;16(2):140-2.
33.Azzolin G, Peduzzi M. Processo de trabalho gerencial e processo de enfermagem na perspectiva de docentes de enfermagem. Rev Gaúcha Enferm. 2008;28:549-55.
34.Garcia SD, Haddad MCL, Dellaroza MSG, Costa DB, Miranda JM. Gestão de material médico-hospitalar e o processo de trabalho em um hospital público. Rev Bras Enferm. 2012;65:339-46.
35.Oliveira NC, Chaves LDP. Gerenciamento de recursos materiais: o papel da enfermeira de unidade de terapia intensiva. Rev Rene. 2009;10(4):19-27.
36.Mello JF, Barbosa SFF. Cultura de segurança do paciente em terapia intensiva: recomendações da enfermagem. Texto contexto-enferm. 2013; 22: 1124-33
37.Lima FDM. Patient Safety and Interventions for quality in health care. Rev Espaço para a Saúde. 2014;15(3):22-9.