RESEARCH ARTICLES
Characterization of patients with renal failure treated at a general hospital emergency department
Eduardo Tavares GomesI; Mônica de Melo Macêdo PapaléoII
I
Nurse, Nursing Specialist in Advanced Life Support from the School of Nursing Nossa Senhora das Gracas, University of Pernambuco. Nursing Specialist in
Cardiology from the Emergency Room of Pernambuco Cardiology Prof. Luiz Tavares da Silva. E-mail: edutgs@hotmail.com
II
Assistant manager nurse at the Emergency Cardiac and Neurological Department of Metropolitan Hospital Metropolitano Oeste Pelopidas Silveira. Clinical
nurse at the Otavio de Freitas Hospital. Nursing Specialist in Nephrology from the Educational Training Center - Faculdade Boa Viagem. E-mail: monicapapaleo@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.5095
ABSTRACT
Health facilities that provide emergency care must be prepared to handle patients in acute renal failure, since early diagnosis, choice of dialysis method, patient preparation and suitable venous access are crucial. This study characterized patients with acute renal failure treated at an general hospital emergency department. This retrospective, quantitative, descriptive study examined data from the medical records of 78 patients treated in July and August 2012 at the Emergency Unit of Otávio de Freitas Hospital, Recife, Pernambuco State. The complaints that bring patients to emergency services can be diverse and unspecific as regards renal pathology, but the post-admission investigation ends by indicating the degree of injury and need for dialysis. A significant number arrive at emergency services already with loss of renal function or end-stage disease, and needing a kidney transplant.
Keywords: Nursing; nephrology; emergency; acute renal failure.
INTRODUCTION
Complications of kidney diseases are frequent causes of care in emergency departments. There are few specialized emergency services or these services rarely have experts available to deal with these complications. This theme is still little researched by nursing1,2.
Kidney diseases are common causes of admission and hospitalization in health services. The diagnosis, choice of dialysis method, patient preparation and appropriate and early venous access are key to effective interventions, preventing serious decompensation of homeostasis. Health facilities providing urgent and general emergency care must be prepared to meet that specific public with well-established protocols and adequate human resources and materials.
Thus, although patients often do not realize that their complaints are of renal origin and resort to general emergency seeking for care, and considering that these complaints are often nonspecific, there is need to further investigate these events and to disseminate symptoms to serve as a warning to professionals and that can direct the planning of health services.
The objective of this study was to describe the sociodemographic and clinical profile of individuals with acute renal failure (ARF) seen in a general emergency.
LITERATURE REVIEW
The incidence of acute renal failure has grown sharply in recent years as a result of two mechanisms: increased prevalence of chronic kidney disease and progress in diagnostic and therapeutic procedures3. The association between the two nosological entities, acute and chronic, has been investigated. The early intervention and diagnosis can bring better results considering that the discovery of the disease in the acute phase could be prevented with well-done tracking3.
Initial signs and symptoms of ARF are nonspecific, hindering early diagnosis 4. In the early stages of the IRA, when the clinical and laboratory manifestations are minimal or absent, the diagnosis may be suggested by the association of nonspecific symptoms (fatigue, anorexia, weight loss, rash, nausea or hemolysis, hypertension, polyuria, nycturia, hematuria or edema). As a result of oliguria and anuria, the main functions of the kidneys, that is, the maintenance of electrolyte and basic acid balance and excretion of nitrogen products become impaired, reflecting in various organs and systems 4,5.
The term uremia describes the process of intoxication and is associated with diverse and heterogeneous symptoms, including itching, neurological manifestations, nausea and vomiting, diarrhea, loss of appetite with anorexia, insomnia and arrhythmias. In addition, uremic patients have increased risk for infections and hematologic complications, and dialysis is mandatory 4.
The reasons for hospitalization of patients include renal and systemic causes associated, such as hypertension, diabetes mellitus, lupus and infection6. The number of new cases estimated for the Northeast region in 2011 was 6,001 patients the incidence rate has been increasing over the years 7. The nurse is responsible for monitoring patients with diabetes and hypertension in primary care, which are the leading causes of kidney disease8.
The impact of the onset of illness in the elderly is intensified by the comorbidities of aging or it is a consequence of aging 9. A study conducted in a nephrology service of the state of Rio de Janeiro shows that 26.6% of admissions were due to post-transplantation complications 10. Another study, in monitoring the progress of renal failure in intensive care units, found that early intervention for critically ill patients was associated with better outcome 5.
Currently, given the continuous and non-continuous dialysis treatment options, specialized nursing must be able to take care of patients undergoing dialysis 11. However, in the initial care, it is important that general and emergency nurses are able to recognize early signs of ARF and have knowledge about the therapeutic approach and systemic repercussions, and above all, the management of vascular access. A recent cohort study found that patients monitored by specialist nurses in nursing periodic consultations had fewer complications, fewer emergency visits and hospital admissions 12.
METHODOLOGY
The present study was held at the General Emergency Service of the Otavio de Freitas Hospital, State Secretariat of Health of Pernambuco. Since 2007, the service has reception and risk classification performed by qualified nurses. The service also has two nurses working at hemodialysis in the emergency room, with six beds each. Regarding hospitalization, renal patients are admitted to another ward with 16 beds. An outsourced specialized clinic is responsible for the care.
It is a descriptive, retrospective study with a quantitative approach. Data were collected from medical records of 78 patients seen in July and August 2012. During that period, 86 cases were assisted, of which eight records were not included for lack of data or incorrect filling that hampered the analysis. To guide data collection, it was designed a suitable instrument for the data source and for the purpose of the research, containing socioeconomic and epidemiological clinical data. Data collection occurred after consideration and approval of the Research Ethics Committee of the hospital - Certificate of Presentation for Ethical Consideration No. 04015612.0.0000.5200 - Opinion REC HOF No. 54385.
From the data collected, blood pressure levels were stratified according to the VI Brazilian Guidelines for Hypertension 13. Renal function was assessed according to the criteria of the Acute Dialysis Quality Initiative (ADQI) that developed, in 2002, the acronym RIFLE that defines three grades of severity of renal impairment - Risk (class R), Injury (Class I) and failure (class F) based on the change in serum creatinine and diuresis - and two development classes (loss - class L - and Final Stage - Class E)14.
Data were analyzed with descriptive epidemiology resource (absolute frequency, relative frequency, etc.) using the statistical software Epi-info and presented in tables.
RESULTS
In the total of 78 records investigated, the average age of patients reached 57.65 ± 18.06 years old, with prevalence of men - 54 (69.23%) - and coming from the metropolitan area of Recife-PE. Only 10 (12.8%) patients were already on dialysis, the average treatment time was of 21.61 ± 16.44 months, according to Table 1.
TABLE 1:
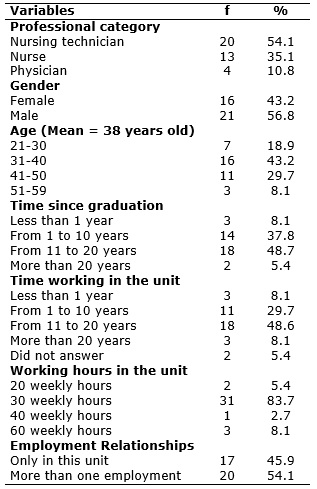
Characterization of professionals from the medical and surgical ICU of a teaching hospital. Goiania, 2011. (N=37)
In the sample, 49 (62.80%) had unchanged hydration status, and only one patient revealed edema. As for blood pressure, 45 (57.69%) had grade-I hypertension at admission, 16 (20.50%) had grade-II hypertension and only one patient with grade-III hypertension. A total of 11 (14.10%) patients were classified as hypotensive at admission, according to Table 1.
As for the urinary elimination, 25 (32.05%) had oliguria, 24 (30.78%) anuria, and only 2 (2.56%), polyuria. Most had spontaneous diuresis - 54 (69.20%) - and use of diapers or urinary device. It was recorded urine with concentrated aspect in 25 (32.10%) patients and hematuria in 31 (39.74%), according to Table 1.
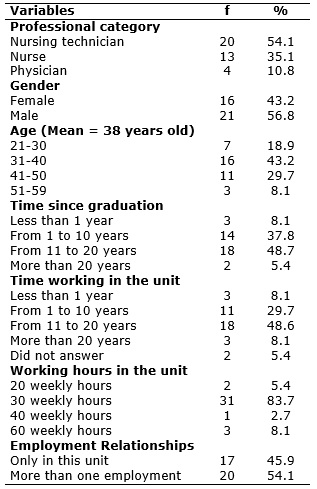
As for the staging of renal failure, considering the volume of diuresis and serum creatine dosage of patients, 19 (24.37%) were classified with renal damage, 30 (38.46%) with renal failure. Of patients, only 2 (2.56%) had loss of kidney function and 12 (15.38%) with end-stage renal disease, according to Table 2.
TABLE 2:
Adverse events occurred in the medical and surgical ICU of a teaching hospital. Goiania, 2011.
After admission and medical diagnosis indicating renal replacement therapy for beginning of treatment, most received central catheter for hemodialysis with triple lumen, deployed mainly in right internal jugular vein in 23 (29.5%) and left internal jugular vein in 14 (17,9%), right iliac fossa of 20 (25.6%) and left iliac fossa of 10 (12.8%) patients. The previously made arteriovenous fistula was used for the treatment of 2 (2.60%) patients who were already on dialysis, according to Table 2.
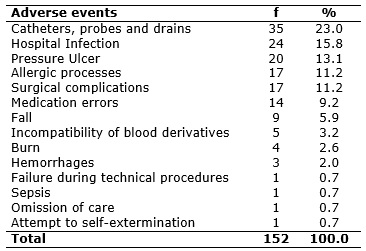
The main complaints that led patients to seek the emergency unit were: abdominal pain - 24 (30.76%), dyspnea - 12 (15.38%), fever - 12 (15.38%) and dysuria - 10 (12, 82%), as shown in Table 3.
TABLE 3:
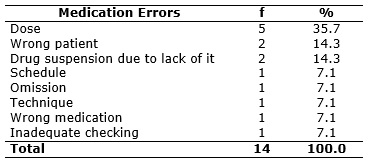
Types of medication errors occurred in the medical and surgical ICU of a teaching hospital. Goiania, 2011.
The medical diagnostic hypotheses at the admission of patients were: ARF - 19 (24.37%), chronic renal failure - 36 (46.15%), high blood pressure - 12 (15.38%), urinary tract infection 8 (10.26%). One (12.38%) patient presented ARF when performing antiretroviral therapy.
DISCUSSION
Early detection of acute impairment of renal function in emergency room visits may trigger a more effective action on patient safety, reducing length of stay in hospital and complications15.
Most patients presented, at admission, the first indicative framework of kidney injury or were unaware of the chronic failure. Patients who had received the diagnosis had an average of less than two years to present complaints characterizing urgent situation, even already being on dialysis.
A study in an emergency unit of England found that 25.4% of admitted patients had acute kidney failure during their stay in hospital, and one third of them had already showed signs and symptoms and laboratory findings that led to the diagnosis on arriving the service.15 Patients tested had higher rate of renal failure (38.46%) than those investigated in England (11.67%), which is probably related to the previous care in primary health care 15.
The average age reported by patients in the study and the higher prevalence of men corroborate other studies 16-21. The age distribution showed no significant difference between elderly and adults.
Blood pressure levels and the hydration status corroborate the findings in other publications9,17-21. A study conducted with intensive care patients had 68.6% of pre-renal causes for patients with no indication for dialysis, and the main was arterial hypertension 22. Hypertension is one of the major modifiable risk factors for various diseases, boosting the group of cardiovascular disease as the leading cause of death in the country 13. In 2011, hypertension was thought to be the main underlying disease for patients on dialysis in the country (35.1%), followed by diabetes (28.4%)7.
Oliguria and anuria, despite not being the main complaints of these patients, had high incidence in the sample, as shown by other research 17. The volume of diuresis is the first criterion for assessment of renal function and is important to the independent staging of the adopted taxonomy and must be controlled rigorously.14 Reduction in volume of diuresis is related to fluid retention, which can exacerbate hypertension and heart failure that may progress to pulmonary edema 4.
Despite not being statistically evaluated, the major complaints may be clinically related to change of fluid and electrolyte balance, more particularly to the sodium and potassium levels and altered blood pH due to the accumulation of nitrogenized excreta. The main complaints were related to other non-specific clinical manifestations, suggesting further epidemiological studies of the association between acute renal failure and other underlying diseases that may cause it. (Table 3) In particular, heart failure, aortic diseases and sepsis, that largely affect older people, can cause renal injury 4.
An international study evaluated retrospectively 5,680 emergency room visits, of which 992 presented sepsis and septic shock. Of these patients, 57.7% developed ARF, which was associated with advanced age, pre-existing renal disease, leukopenia and thrombocytopenia. The group that developed acute renal failure also showed higher mortality and length of hospital stay23.
As for vascular access, another study assessed 23 clinical centers in seven Brazilian states. It showed that for patients with chronic kidney failure, arteriovenous fistulae were chosen by 93.4%24. However, due to the emergency nature of the need for treatment versus the time required for the maturation of the fistula, catheters have been deprecated in 97.4% of cases. This study found that, in the Northeast region, 47% of the catheters were implanted into the internal jugular vein and 33%in the subclavian vein24.
The sample had deployed access, in order of incidence, in jugular veins, femoral veins and subclavian veins. However, other authors point out that the subclavian veins are preferred because of the greater ease of catheter placement24-26. Studies show that the risk of infection increases significantly in central venous catater inserted into the internal jugular vein in relation to insertion into the subclavian vein, which is, in turn, associated with increased risk of non-infectious complications (pneumothorax, hemothorax, venous thrombosis)4,26. Although it is not yet used in the Brazilian services, studies indicate that there may be benefits in the early use of peritoneal dialysis in ARF 27.
Although it was not evaluated in this study, other national research conducted with 129 trauma patients admitted to an emergency unit revealed that 52 (40.31%) developed ARF, of which 19 (36.5%) required dialysis. In this sample, all patients with ARF resulting from trauma died28. In England, a survey with 765 patients of general emergency services pointed out that the ARF is more frequent than the existing literature suggests, reaching 25% of cases of admissions and is associated with increased length of hospital stay, admission chance in intensive care beds and risk of death15. Another publication, comparing patients achieving resolution of ARF within 5 days compared to patients with ARF for a larger time acquired in the hospital, more than six days, revealed that the increase in the resolution time increased significantly the risk of death during hospitalization and in post-discharge, for up to 240 days29.
CONCLUSION
It is useful to understand the manifestations of kidney damage by emergency room nurses, especially those that perform sorting, reception and risk classification. Complaints that motivate patients to seek emergency units can be diverse and unspecific in relation to renal pathology, but the investigation after admission ends for indicating the degree of injury and the need for dialysis. Many patients seek emergency units and receive diagnosis of renal insufficiency, because they have not had chronic kidney disease previously known. A significant group comes to emergency services already with loss of renal function or end stage disease and needing a kidney transplant.
Regarding the assistance, health services with emergency care should recognize the need to provide dialysis promptly, seeking to improve the prognosis. Health facilities should establish an organized network to offer, in the reference and counter-reference system, the necessary care, and each unit must ensure the supply of catheters and quality materials.
The study was limited by the time available for collection, which limited the study sample. Furthermore, it depicts the evidence of only one service. In later studies, the risk factors and other causes that may be related to the event should be evaluated.
REFERENCES
1.Carvalho GMC, Lima FET, Barbosa IV, Melo EM. Estudos brasileiros sobre nefrologia nas teses e dissertações de enfermagem. Rev Bras Enferm. 2010 [citado em 31 jul 2015] 63: 1052-3. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672010000600028&lng=pt. http://dx.doi.org/10.1590/S0034-71672010000600028
2.Pennafort VPS, Furtado AM, Fialho AVM, Moreira TMM, Freitas MC, Queiroz MVO. Produção do conhecimento científico de Enfermagem em Nefrologia. Rev Bras Enferm. 2010 [citado em 31 jul 2015] 63:830-6. Disponível em: http://www.scielo.br/scielo.php?script=sci_pdf&pid=S0034-71672010000500022&lng=en&nrm=iso&tlng=pt
3.Schmidt JJ, Beutel G, Kielstein JT. Diagnosis and pathophysiology of acute renal failure - is prevention possible? Dtsch Med Wochenschr. 2015 [citado em 31 jul 2015]; 140:245-9. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/25704519
4.Patschan D, Muller GA. Acute kidney injury. J Inj Violence Res. 2015 [citado em 31 jul 2015]; 7(1): 19-26. Disponível em: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4288292/pdf/jivr-07-19.pdf
5.Silva VTC. Insuficiência renal aguda em unidade de tratamento intensivo: perfil epidemiológico e validação de índices prognósticos [tese de doutorado] São Paulo: Universidade de São Paulo; 2007.
6.Oliveira FC, Alves MDS, Bezerra AP. Co-morbidades e mortalidade de pacientes com doença renal: atendimento terceirizado de nefrologia. Acta Paul Enferm. 2009 [citado em 31 jul 2015] 22:476-80 Disponível em: http://www.scielo.br/pdf/ape/v22nspe1/03.pdf
7.Sesso RCC, Lopes AA, Thomé FS, Lugon JR, Watanabe Y, Santos DR. Diálise Crônica no Brasil - Relatório do Censo Brasileiro de Diálise, 2011. J Bras Nefrol. 2012 [citado em 31 jul 2015] 34: 272-7. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0101-28002012000300009&lng=pt. http://dx.doi.org/10.5935/0101-2800.20120009
8.Travagim DSA, Kusumota L, Teixeira CRS, Cesarino CB. Prevenção e progressão da doença renal crônica: atuação do enfermeiro com diabéticos e hipertensos. Rev enferm UERJ 2010 [citado em 31 jul 2015] 18: 291-7. Disponível em: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S0104-35522010000200021&lng=pt
9.Ribeiro DF. O cuidador do idoso com insuficiência renal crônica em diálise peritoneal ambulatorial contínua [dissertação de mestrado] Ribeirão Preto (SP): Universidade de São Paulo; 2008.
10.Ribeiro RCHM; Garcia TPR; Bertolin DC; Cesarino CB; Poletti NAA; Rodrigues AMS. Pacientes vítimas de politrauma com insuficiência renal aguda na Unidade de Terapia Intensiva. Acta Paul Enferm. 2008 [citado em 31 jul 2015] 21:216-20. Disponível em http://www.scielo.br/scielo.php?script=sci_pdf&pid=S0103-21002008000500015&lng=en&nrm=iso&tlng=pt
11.Araujo STC; Koeppe GBO. Setor de nefrologia: uma parceria entre ensino e service. Acta Paul Enferm. 2012 [citado em 31 jul 2015] 22:572-6. Disponível em: http://www.scielo.br/pdf/ape/v22nspe1/26.pdf
12.Lee DTF, Choi CK, Chan CW, Chair SY, Chan D, Fung SYK et al. The impact on patient health and service outcomes of introducing nurse consultants: a historically matched controlled study. BMC Health Services Research. 2013 [cited in 2015 Mar 9]; 13:431. Available from: http://www.biomedcentral.com/1472-6963/13/431
13.Sociedade Brasileira De Cardiologia, Sociedade Brasileira De Hipertensão, Sociedade Brasileira De Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq bras cardiol. 2010 [citado 22 jan 2013] 95(1): I-III. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0066-782X2010001700001&lng=pt. http://dx.doi.org/10.1590/S0066-782X2010001700001
14.Kim MH, Koh SO, Kim EJ, Cho JS, Na SW. Incidence and outcome of contrast-associated acute kidney injury assessed with Risk, Injury, Failure, Loss, and End-stage kidney disease (RIFLE) criteria in critically ill patients of medical and surgical intensive care units: a retrospective study. BMC Anesthesiol. 2015 [cited in 9 Mar 2015]; 15: 23. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4360925/
15.Challiner R, Ritchie JP, Fullwood C, Loughnan P, Hutchison A. Incidence and consequence of acute kidney injury in unselected emergency admissions to a large acute UK hospital trust. BMC Nephrology. 2014 [citado em 9 mar 2015]; 15:84. Disponível em: http://www.biomedcentral.com/1471-2369/15/84
16.Santos ER. Lesão renal aguda em terapia intensiva avaliada pelo RIFLE. Rev bras ter intensiva. 2009 [citado em 31 jul 2015]; 21:359-68. Disponível em: http://www.scielo.br/pdf/rbti/v23n3/v23n3a10.pdf
17.Silva Júnior GB, Daher EF, Mota RMS, Menezes FA. Risk factors for death among critically ill patients with acute renal failure. Sao Paulo Med J. 2006 [cited in 2015 Jul 31]; 124(5):257-63. Available from: http://www.scielo.br/pdf/spmj/v124n5/04.pdf
18.Balbi AL, Gabriel DP, Barsante RC, Caramori JT, Martin LC, Barreti P. Mortalidade e prognóstico específico em pacientes com insuficiência renal aguda. Rev Assoc Med Bras. 2005 [citado em 31 jul 2015]; 51: 318-22. Disponível em: http://www.scielo.br/pdf/ramb/v51n6/27532.pdf
19.Pinto OS, Carminatti M, Lacet T, Rodrigues DF, Nogueira LO, Bastos MG et al. Insuficiência renal aguda nefrotóxica: prevalência, evolução clínica e desfecho. J Bras Nefrol 2009 [citado em 31 jul 2015]; 31:183-9. Disponível em: http://www.scielo.br/pdf/jbn/v31n3/v31n3a03.pdf
20.Silvester W, Bellomo R, Cole L. Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med. 2001 [cited in 2015 Jul 31]; 29:19105. Disponível em: http://www.ncbi.nlm.nih.gov/pubmed/11588450
21.Xavier BLS, Santos I, Almeida RF, Clos AC, Santos MT. Características individuais e clínicas de clientes com doença renal crônica em terapia renal substitutiva. Rev enferm UERJ. 2014 [citado em 31 jul 2015]; 22:314-20 Disponível em: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/13683/10474
22.Bernardina LC, Diccini S, Belasco AGS, Bittencourt ARC, Barbosa DA. Evolução clínica de pacientes com insuficiência renal aguda em unidade de terapia intensiva. Acta Paul Enferm. 2008 [citado em 31 jul 2015] 21:174-8. Disponível em http://www.scielo.br/pdf/ape/v21nspe/a07v21ns.pdf
23.Sang Heon Suh, Chang Seong Kim, Joon Seok Choi, Eun Hui Bae, Seong Kwon Ma, Soo Wan Kim. Acute kidney injury in patients with sepsis and septic shock: risk factors and clinical outcomes. Yonsei Med J. 2013 [cited in 2015 Jul 31]; 54:965-72. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3663224/pdf/ymj-54-965.pdf
24.Linardi F, Linardi FF, Bevilacqua JL, Morad JFM, Costa JA, Miranda Júnior F. Acesso vascular para hemodiálise: avaliação do tipo e local anatômico em 23 unidades de diálise distribuídas em sete estados brasileiros. Rev col bras cir. 2003 [citado em 31 jul 2015] 30(3) 183-93. Disponível em http://www.scielo.br/pdf/rcbc/v30n3/a05v30n3.pdf
25.Nasir Mahmood S, Naveed Mukhtar K, Iqbal N, Umair SF. Pre dialysis care and types of vascular access employed in incident hemodialysis patients: A study from Pakistan. Pak J Med Sci. 2013 [cited in 2015 Jul 31] 29:828-31. Disponível em: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3809299/pdf/pjms-29-828.pdf
26.Grothe C, Belasco AGS, Bittencourt ARC, Vianna LAC, Sesso RCC, Barbosa DA. Incidência de infecção da corrente sanguínea nos pacientes submetidos à hemodiálise por cateter venoso central. Rev Latino-Am Enfermagem. 2010 [citado em 31 jul 2015] 18(1) Disponivel em http://www.scielo.br/pdf/rlae/v18n1/pt_12.pdf
27.Yong K, Dogra G, Buodville N, Pinder M, Lim W. Acute kidney injury: controversies revisited. Int J Nephrol. 2011 [cited in 2015 Jul 31] 2011:762634. Disponível em: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108161/pdf/IJN2011-762634.pdf
28.Abreu KLS, Silva Júnior GB, Barreto AGC, Melo FM, Oliveira BB, Mota RMS et al. Acute kidney injury after trauma: prevalence, clinical characteristics and RIFLE classification. Indian J Crit Care Med. 2010 [cited in 2015 Jul 31]; 14(3): 121–8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021827/
29Yoo J, Lee JS, Lee J, Jeon JS, Noh H, Han DC, Kwon SH. Relationship between duration of hospital-acquired acute kidney injury and mortality: a prospective observational study. Korean J Intern Med. 2015 [cited in 2015 Jul 31]; 30:205-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25750562