VRQOL: Vision related to quality of life; VA: Vision acuity
a: predictor effect; b: moderator/interaction effect
FIGURE 1: Hypothetical model of relationship between the variables.
RESEARCH ARTICLES
Vision, quality of life and medication adherence in older adults with diabetic retinopathy
Fernanda Freire JannuzziI; Fernanda Aparecida CintraII; Maria Cecília Bueno Jayme GallaniIII; Andréa Mara Simões TorigoeIV
INurse, Ph.D. in Health Science. Nursing School, State University of Campinas. São Paulo, Brazil. E-mail: fernandafj@yahoo.com.br
IINurse, Ph.D. in Nursing, Associate Professor, Nursing School, State University of Campinas. São Paulo, Brazil. E-mail: fernanda@fcm.unicamp.br
IIINurse, Ph.D. in Nursing, Associate Professor, Nursing School – State University of Campinas. São Paulo, Brazil. Professor, Faculté dês Sciences
Infirmières, Universtié Laval. Québec, Canada. E-mail: maria-cecilia.gallani@fsi.ulaval.ca
IVMedical, Ph.D. in Medical Science, Medical Science School, State University of Campinas. São Paulo, Brazil. E-mail: andreatorigoe@hotmail.com
VArticle extracted from the Master´s Dissertation Vision-related quality of life and medication adherence in elderly patients with retinopathy diabetic presented to the Graduate Program in Nursing,
Medical Science School, State University of Campinas. São Paulo Brazil.
DOI: http://dx.doi.org/10.12957/reuerj.2015.4916
ABSTRACT
This cross-sectional study examined the influence of vision-related quality of life (VRQoL) on medication adherence, and the moderator effect of visual acuity (VA) in the relationship of VRQoL to adherence, in older adults with diabetic retinopathy. The study sample comprised elderly patients taking oral antidiabetic/insulin and antihypertensive drugs. Medication adherence rate, and its association with care taken in drug administration, were assessed. The National Eye Institute Visual Function Questionnaire was used to evaluate VRQoL. Analysis of the joint relationship and bivariate analysis of variance were applied to test the moderator effect of VA in the relationship between VRQoL and adherence. Of the 100 patients tested, 58% classified as adherent. Those with worse VRQoL and severe visual impairment or blindness showed, respectively, 3.34 and 2.95 higher probability of non-adherence. However, the moderator effect studied was not observed. The data confirmed that the effects of VA and VRQoL on adherence were independent of each other. Keywords: Medication adherence; quality of life; diabetic retinopathy; health of older adults.
INTRODUCTION
Some diseases are highlighted by progressive evolution among the ocular disorders commonly manifest in aging, chronicity, and especially by the vision impairment, often irreversible. Diabetic retinopathy (DR) is one of the most prevalent and debilitating microvascular complications that often occurs in patients with diabetes1,2.
Here there are the risk factors to the DR: diabetes type, manifestation time and metabolic control of the disease, hematocrit and hemoglobin levels, glycated hemoglobin, total cholesterol, proteinuria and hypertension3-5.
Most blindness cases in adults and the elderly are related to DR and they can be avoided by applying actions including early diagnosis and the possibility of intervention in the early stages of the disease, as well as glycemic control and blood pressure with healthy lifestyle habits and correct use of prescribed medications. These actions slow the progression of retinal changes without reversing the damage already installed6.
The visual changes from DR have significant impact on quality of life. The process of perception of the signs and symptoms is experienced in a unique, personal way, and requires overcoming attitude and facing losses7.
From this perspective, the identification of factors related to medication adherence in elderly patients with DR enables the planning of action strategies to control the disease, improving visual prognosis and therefore prevention of disabilities that affect health-related quality of life (HRQOL) of these subjects.
Baron and Kenny8 have a moderating effect model between variables of interest, defining the moderating variable as the one that affects the direction and/or strength of the relationship between the predictor or independent variable and the dependent or criteria variable. See Figure 1.
VRQOL: Vision related to quality of life; VA: Vision acuity
a: predictor effect; b: moderator/interaction effect
FIGURE 1:
Hypothetical model of relationship between the variables.
Based on this model, it is assumed that VRQOL is a predictor of medication adherence, whose association is moderated by visual acuity (VA).
The present study aimed to analyze the influence of VRQOL on medication adherence, and the VA moderator effect on VRQOL and adherence in elderly patients with diabetic retinopathy.
LITERATURE REVIEW
The concept of medication adherence can be defined as the use of prescribed medication by at least 80% of its total observing schedules, dose, treatment time, representing the final step of what is suggested as rational medication use9.
For the elderly who often have associated co-morbidities and are subject to multipurpose medication, non-adherence to medication therapy may be a risk for health, by the inadequate control of the disease. In an economic perspective, non-adherence may also involve greater use of health services, additional expenses in hospitalization and use of a medication therapy even more extensive10,11.
The use of medications by the elderly is influenced by factors related to age, such as vision, hearing and memory, and others that include environmental, social and financial support, and perceived needs12. However, there is no evidence in the literature about this association, or the effect of VA and HRQOL, or more specifically related to visual function on medication adherence in elderly patients with retinopathy.
METHODOLOGY
Descriptive/exploratory cross-sectional research, correlational type, held in Ophthalmology Clinic of a university hospital in the state of São Paulo.
The sample was 100 elderly patients with diagnosis of DR, in continuous use of anti-hypertensive medication and/or oral antidiabetics/insulin, monitored in the selected clinic. The subjects with other eye disorder responsible for low vision and those undergoing eye surgeries in less than 30 days of data collection were excluded13.
The sample size was estimated considering the nature of research and the extent of data collection instruments. From the predictor variables (VA for distance and near vision, the association of the both measures of VA and VRQOL), the value of eight subjects per variable was determined with an increase of 50 subjects to this value14.
Data collection was conducted in the period between February and December 2008, through structured individual interviews.
On the eve of data collection, by telephone to patients potentially eligible for the study, it was asked to bring the prescriptions of medications in continuous use, accompanied by bottles or tablets of the respective pills. It intended to ensure the identification of all prescribed medications, as well as the way indicated in the recipe for their use15.
Characterization of the subjects : questionnaire of a sociodemographic data (age, gender, schooling and family income), clinical characterization and reported measure of VA for distance (Optometric Table of Snellen) and for near vision (Jaeger Table) with optical correction if patients do use. The values of this measure were obtained from the charts of the patients, after ophthalmologic evaluation performed in interview date.
The elderly were grouped according to the VA for distance vision (Groups I, II, III and IV), according to the World Health Organization16. In VA for near vision groups A, B and C were created17,18. These ratings suffered small adjustments to this research. In addition to these groups, other two groups were created (1 and 2) with the combination of both distances, in which the group 1 was considered as one with normal or near normal vision for distance and near vision (VA ≥ 20/60 and ≥ J3) and group 2 with low vision for distance and near vision (VA < 20/60 and/or < J3).
The National Eye Institute Vision Function Questionnaire (NEI VFQ-25) was used; an instrument which purpose is to measure the influence of vision in multiple dimensions of HRQOL, emotional well-being and social functioning. It is in a specific questionnaire to be applied in various chronic eye conditions19. The cultural adaptation in Brazil was carried out by Fonseca20. The NEI VFQ-25 consists of 25 items collected in 12 domains or subscales. The total and each domain score ranges on a scale from zero to 100, zero being the worst and 100 the best quality of life.
The measure of medication adherence to oral antidiabetic medication/insulin and anti-hypertensive was considered according to two criteria: proportion and global assessment of adherence.
Proportion of adherence : measured by an instrument composed of four tables comprising: 1. Description of the name, dose, and dosage form of all prescription medication; 2. Description of use of each prescribed medication within 24 hours prior to the interview; 3. Description of their use in the week preceding the interview; and, 4. Description of use in the previous month. Tables 2 and 3, regarding the use of medication in the day and the week before, respectively, aim to get more accurate answers by minimizing the bias of memory21. Adherence was calculated from the doses omitted in the previous month, reported by the patient, using the following calculation: [(prescribed doses - missed doses) x 100 / prescribed doses]22. For calculation, the subjects who used doses superior to those prescribed had their adherence to the prescribed values converted to the corresponding index of less than 100% (since the use of the medication beyond the prescribed means non-adherence)23.
For subjects who used more than one medication, the final ratio of adherence was calculated by the average of each medication adherence percentages. The proportion of adherence was treated as a continuous variable (considering the average proportion of medication use), and as a categorical variable: adequate and inadequate dose, with a cutoff value of 80% adherence.
Global adherence assessment: beyond the medication proportion used, their dosage form were also assessed, that is, the number of medications taken and their association with temporal markers as fasting, breakfast, lunch, dinner. Thus, for global adherence assessment, patients were classified into four groups: I - Dose and care appropriate to the prescription; II - Correct dose and inadequate care; III - Insufficient dose and adequate care; and IV - inadequate dose and care.
The data were initially entered into the Statistical Package for Social Sciences (15.0 for Windows) for the analysis: descriptive, comparison (Chi-square or Fisher´s exact test, Mann-Whitney, Kruskal-Wallis and Spearman correlation coefficient) and joint relationship (logistic regression analysis and univariate model). Bivariate analysis of variance (VRQOLxVA) was performed to test VA moderator effect on the relationship VRQOL - adherence.
The significance level for statistical tests was 5%.
The study was approved by the local Ethics Committee in Research (Opinion Number 777/2007). All enrolled subjects signed the Informed Consent and Informed Term after clarification of the guaranteed anonymity and the freedom to quit at any time.
RESULTS
The subjects were aged 69.5 years old average (± 7.1); most of them were women (62%). Schooling was low, with an average of 4.0 years (± 3.0). All had medical diagnosis of diabetes and 85% of hypertension. Of all medication in continuous use by the elderly 3.3 on average (± 1.5) were intended for the treatment of hypertension and/or diabetes.
Considering the stratification of VA for distance vision, the elderly presented the following distribution: 44% normal or near normal vision; 37% moderate low vision; 17% severe/deep low vision; and 2% near or total blindness. In the near vision stratification, 63% of elderly belonged to the group with normal or near normal vision; 15% were in the low vision group; and 22% had blindness. Considering the combination of the two VA distances, the highest percentage (62%) are concentrated in the group with low vision.
In the implementing of NEI VFQ-25, the highest scores were observed in the Color Vision, Driving and Social Functioning, which reveals a trend to improve VRQOL. The lowest scores were obtained on the subscales General Health and General Vision. Only 10 subjects responded to items included in the Driving. The average total score of the instrument was 71.8 (± 22.7), ranging between 12 and 99.4.
The comparative analysis between the VA (for distance, near and both) and the total score of NEI VFQ-25 instrument showed that individuals with poor vision had lower scores on the assessment of VRQOL. That is, the score obtained in NEI VFQ-25 had significant difference between the groups I, II, III and IV of distance VA (p-value <0.001) between groups A, B and C of near VA (p -value <0.001) as well as in groups 1 and 2 in VA combination for distance and near vision (p <0.001).
Among the elderly patients, 85% used anti-hypertensive medication. All were taking medications for the treatment of diabetes, and 48% were insulin-dependent.
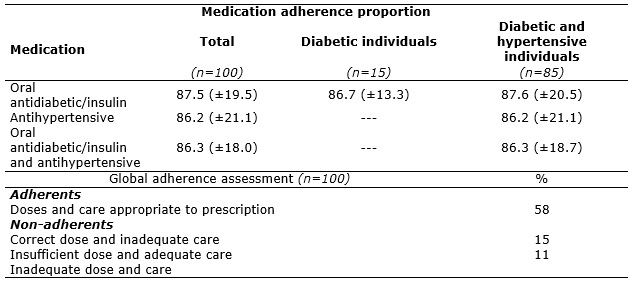
In the month preceding the study, subjects reported use of 86.3% (± 18.0) of the prescribed doses of medication for hypertension and/or diabetes. Few over half of the study group (58%) reported using 80% or more of the prescribed dose and follow the necessary precautions in taking medication (Group I). The other elderly (Groups II, III and IV) were aggregated into a single class. Thus, they constituted two classes: Adherents (n=58), formed by the subjects in Group I and Non-adherents (n=42), with individuals from the other groups. See Table 1.
Table 1:
Medication adherence according to adherence proportion criteria and classification according to adequacy of dose and care. University Hospital, São Paulo
State, 2008.
To identify the possible association between the independent variables (VA and VRQOL) and non-adherence to medication therapy, an exploratory analysis testing the correlation between the variables was performed, as shown in Table 2.
TABLE 2:
Univariate logistic regression analysis for non-adherence medication (n=100).
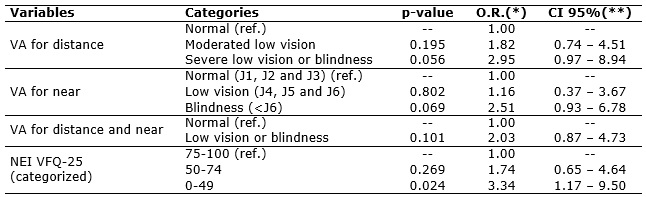
(*) O.R. (Odds Ratio) = Risk ratio for non-adherence medication (n= 42 Non-adherent and n= 58 Adherent). (**)CI 95% = Confidence Interval of 95% for
the risk ratio.
Ref.: category used as reference for analysis.
VA: visual acuity.
The analysis indicates that subjects with worse VRQOL (total score 0-49 in NEI VFQ-25) and those with severe low distance vision or blindness have 3.34 (p = 0.024) and 2.95 (p = 0.056) more likely to non-adherence to medication therapy, when compared to subjects with better VRQOL and distance VA, respectively.
To study the moderating effect of VA (for distance, near and both) in the relationship between VRQOL and non-adherence medication, the procedure described by Cohen & Cohen in 1983 was employed, adding the product (interaction term) of the independent variables and the moderator regression equation. Considering X (VRQOL) as an independent variable, Z (VA) as moderating variable and Y (non-adherence) as the dependent variable, the regression of Y in X, Z and XZ was made. The moderating effect is indicated by the significant effect of XZ, while X and Z are controled8. However, the model used did not confirm the VA moderating effect on the relationship between VRQOL and the adherence.
DISCUSSION
In the sample studied, most of the subjects were concentrated in the group with low vision, in the association of VA measures for far and near. The literature suggests that at any stage of DR can occur significant reduction in VA, caused by macular edema, although it is more frequent in advanced stages 7,24.
It is noteworthy the scores found in NEI VFQ-25 instrument. The highest average and with better quality of life were obtained in: Social Function, Driving and Color Vision, while the lowest were related to General Health and General Vision. Other studies also report higher scores of these domains in patients with different ophthalmic diseases20,25 and in healthy subjects26.
In this study, the worst VRQOL in General Health can be attributed to the clinical condition of the elderly, related to comorbidities, polypharmacy
and other not identified variables in the sample characterization. With respect to score on the subscale
General
Vision,
it can be associated to low VA (for distance and/or near) presented by most elderly. On the other hand, a high score in Driving should be
interpreted with caution. Considering the high number of missing items in this domain, it is observed that among the 100 elderly respondents only 10 who
responded to the questions of this group drive cars and did not perceive difficulty or loss in this activity by VA decrease.
Univariate regression analysis indicated that VRQOL and VA variables (this with borderline statistical significance) as independent predictors of adherence, confirming the central assumption of the analysis performed in this study.
Regarding VRQOL, possibly the subjects that evaluated this construct more positively had the perception of greater autonomy and self-efficacy, resulting from a richer individual repertoire of resources and skills that allow greater independence and security in the handling of medications in use, which could contribute to greater adherence.
Similarly, the VA was also a predictor of adherence. It is possible to observe that the low VA interferes negatively in the operationalization of the use of medication, resulting in several difficulties that may be related since the recognition of the label on tablets, the capsules/pills, even the preparation/implementation of proper dosage, and even in the forms of acquisition of medicines.
Considering both the quality of life as the VA were predictive of adherence, the assessment of quality of life was related to visual function, it can be assumed VA as a moderator variable of the relationship between VRQOL and adherence. Thus, in subjects with worse VA (and therefore with smaller individual resources for the management of medications) would perceive worse VRQOL, which show a positive correlation with non-adherence. The same would not happen to subjects with normal VA.
To verify this supposition, it was held an analysis of VA moderating effect on the relationship between VRQOL and medication adherence. A moderator is a qualitative (in this study, standard or lowered VA) or quantitative variable affecting the direction and/or strength of the relationship between an independent variable, or predictor, and a dependent variable or criteria. In a correlational view, a moderator is a third variable which affects the zero correlation between two other variables, changing the direction of the correlation or substantially reducing the magnitude of this correlation18 .
However, in the analysis of the moderating effect, it was observed that VA does not moderate the relationship between VRQOL and (non)adherence, confirming that the effect of the adherence occurs on both independently.
CONCLUSION
This research is unprecedented in the statement that the VRQOL is a predictor of medication adherence factor in the elderly, that is, the worse the perception of quality of life related to vision, the lower the adherence.
The absence of VA moderating effect means that regardless of the relationship of this variable with VRQOL, it is an important determinant of adherence, that is the perception of vision of impact on quality of life directly affects the adherence for the use of medication. Although the comparative analysis between the VA and the score of the NEI VFQ-25 has shown a positive relationship between these variables, it means that the perception of worsening VRQOL cannot be attributed only to VA, but the other intrinsic and extrinsic factors to the subject not measured in this study. In other words, the relationship between VRQOL and medication adherence is unaffected by VA, but possibly the set of facets that comprise this construct.
For elderly with DR, whose visual prognosis is not always favorable to the maintenance of normal or near normal vision, the VRQOL becomes relevant in this prognosis, given their relation with the adherence to the clinical management of diabetes and hypertension. Besides the limitations commonly manifest in the elderly, which can contribute negatively in VRQOL and therefore, in the adherence with the use of medication.
Therefore, for the nursing educational practice, it is important the interventions aimed at improving adherence among elderly with low VA and among those who reveal worse VRQOL, although not presenting big decreasing of VA.
REFERENCES
1.Fowler MJ. Microvascular and macrovascular complications of Diabetes.Clin Diabetes. 2008;26(2):77-82.
2.Sociedade Brasileira de Diabetes. Diretrizes da Sociedade Brasileira de Diabetes: 2013-2014. São Paulo: AC Farmacêutica; 2014.
3.Jongsareejit A, Potisat S, Krairittichai U, Sattaputh C, Arunratanachote W.The Thai DMS diabetes complications (DD.Comp.) project: prevalence and risk factors of diabetic retinopathy in Thai patients with type 2 diabetes mellitus.J Med Assoc Thai. 2013; 96: 1476-82.
4.Hammes HP.Optimal treatment of diabetic retinopathy.TherAdvEndocrinolMetab. 2013;4 (2):61-71.
5.The UK Prospective Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in patients with type 2 diabetes (UKPDS).BMJ. 1998;317: 703-12.
6.Gross JL, Nehme M. Detecção e tratamento das complicações crônicas do diabetes melito: Consenso da Sociedade Brasileira de Diabetes e Conselho Brasileiro de Oftalmologia.RevAssocMed Bras.1999;45: 279-84.
7.Andrade NHS, Zanetti ML, Santos MA. A percepção visual de pacientes com retinopatia diabética, segundo o referencial de Merleau-Ponty. Rev enferm UERJ. 2008;16: 249-54.
8.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical consideration. J PersSocPsychol. 1986;51:1173-82.
9.Leite SN, Vasconcellos MPC. Adesão à terapêutica medicamentosa: elementos para a discussão de conceitos e pressupostos adotados na literatura.Ciênc Saúde Coletiva. 2003;8: 775-82.
10.Balkrishnan R, Rajagopalan R, Camacho FT, Huston AS, Murray FT, Anderson RT. Predictors of medication adherence and associated health care cost in an older population with type 2 Diabetes Mellitus: a longitudinal cohort study. ClinTher. 2003;25:2958-71.
11.Hughes CM. Medication non-adherence in the elderly. Drugs Aging. 2004;21:793-811.
12.Murray MD, Morrow DG, Weiner M, Clark DD, Tu W, Deer MM et al. A conceptual framework to study medication adherence in older adults.Am J GeriatrPharmacother.2004;2:36-43.
13.Cintra FA, Guariento ME, Miyazaki LA. Adesão Medicamentosa em idosos em seguimento ambulatorial. Ciênc Saúde Coletiva. 2010;15(suppl3):3507-15.
14.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th ed. Boston: Allyn and Bacon; 2001.
15.Chatkin JM, Cavalet-Blanco D, Scaglia NC, Tonietto RG, Wagner MB, Fritscher, CC. Adesão ao tratamento de manutenção em asma (estudo ADERE). J BrasPneumol. 2006;32:277-83.
16.World Health Organization (WHO). CDC. Centers for Disease Control and Prevention.Classifications of Diseases, Functioning, and Disability [online].International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM).ICD-10-CM Files via FTP: 2014. Dtab12.zip. ICD-10-CM Tabular list of diseases and injuries (FY12).H54.7. Unspecified visual loss.p.356. [cited in 2014 Jan 23] Available from: URL:http://www.cdc.gov/nchs/icd/icd10cm.htm
17.Javitt J, Brauweiler HP, Jacobi KW, Klemen U, Kohner S. Cataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria.J Cataract Refract Surg. 2000; 26: 1356-66.
18.Katina JH, Lyra JMAG, Souza CD, Trindade FC. Tratamento cirúrgico da catarata pediátrica. Arq Bras Oftalmol. 2002; 65: 193-7.
19.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-Item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001; 119: 1050-8.
20.Fonseca ICM. Adaptação cultural do National EyeInstitute Visual Functioning Questionnaire (NEI VFQ-25) para idosos brasileiros com baixa visão [dissertação de mestrado]. Campinas (SP): Universidade Estadual de Campinas; 2006.
21.Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D, Frossard PM et al. Factors associated with adherence to anti-hypertensive treatment in Parkinson. PloS ONE.2007;2(3): e280.
22.Ventura-Cerdá JM, Mínguez-Gallago C, Fernández-Vellalba EM, Alós-Almiñana M, Andrés-Soler J. Escalasimplificadaparadetectarproblemas de adherencia (ESPA) al tratamientoantirretroviral. Farm Hosp. 2006;30(3):171-6.
23.Delgado AB, Lima ML. Contributo para a validação concorrente de uma medida de adesão aos tratamentos. PsicSaúde&Doenças. 2001;2 (2):81-100.
24.Chew EY, Klein ML, Ferris III FL, Remaley NA, Murphy RP, Chantry K et al. Association of elevated serum lipid levels with retinal hard exudates in diabetic retinopathy: Early Treatment Diabetic Retinopathy Study (ETDRS) Repot 22. Arch Ophthalmol. 1996;114: 1079-84.
25.Hoeksema L, Los LI.Vision-related quality of life in herpetic anterior uveitis patients. PLoS One. 2014;9 (1):e85224.
26.Globe D, Varma R, Azen SP, Paz S, Yu E, Peston-Martin S et al. Psychometric performance of the NEI VFQ-25 in visually normal Latinos: The Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2003;44: 1470-8.