RESEARCH ARTICLES
Nursing prostatectomy patients
Daniele Raiane Florentino dos SantosI; Camila Araújo Florêncio de LimaII; Elisandra de Araújo SaldanhaIII; Maria Isabel da Conceição Dias Fernandes CavalcantiVI; Ana Beatriz de Almeida MedeirosV; Ana Luisa Brandão de Carvalho Lira VI
I
Nurse. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: daniele_raiane@hotmail.com
II
Nurse. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: camillabecker_@hotmail.com
II
I
Nurse. Master in Nursing. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: sansaldanha@yahoo.com.br
I
V
Nurse. PhD Student in Nursing. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: bebel_6@hotmail.com
V
Nurse. PhD Student in Nursing. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: abamedeiros@gmail.com
VI
Nurse. PhD. Associate Professor, Department of Nursing. Federal University of Rio Grande do Norte. Natal / Rio Grande do Norte, Brazil. E-mail: analuisa_brandao@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2015.4218
ABSTRACT
This descriptive study aimed to identify the activities of urological nursing professionals in caring for postoperative prostatectomy patients, and to compare them with those described in the literature. It was conducted at a university hospital in northeastern Brazil, in August and September 2011, with 18 nursing professionals, including nurses, nurse technicians and nursing assistants, who answered a questionnaire about their sociodemographic data and the care they provided to postoperative prostatectomy patients. The nursing care was grouped into six categories: postoperative guidance; treatment of urinary incontinence; treatment of erectile dysfunction; treatment of pain; psychological monitoring; and treatment of hyponatremia. It was concluded that nursing professionals, at odds with the literature, emphasized postoperative guidance, treatment of urinary incontinence and pain, and mental health counseling.
Keywords: Nursing care; prostatectomy; postoperative period; practical nursing.
INTRODUCTION
Worldwide, prostate-related diseases, especially cancer and Benign Prostatic Hyperplasia (BPH), have been discussed as an important public health problem. In Brazil, increase in the incidence of these diseases over the years was due to increased expectation of life, to the development of diagnostic techniques and to the progress of the country's information systems1.
Prostate cancer is named as the second most frequent cancer in men, with growing incidence rate worldwide1. BPH is already considered one of the three diseases that contribute most to health expenditure in industrialized countries. In addition, 30 of each 100 thousand men die because of BPH 2.
Treatment for both diseases depends on the patient's clinical picture. Options range from a conservative approach, such as observation and drug treatment, to surgical procedures, which can bring many complications, affecting both the physical and psychological aspect of the individual3.
Among the complications, there is highlight for the urinary incontinence, erectile dysfunction, pain and the formation of clots that can block the indwelling catheters, distend the prostatic capsule and cause bleeding. In addition, after surgery the patient may also experience emotional conflicts, among these fear, helplessness, anger and sadness. These feelings can be intensified by expectations created regarding the possibility of getting cured from a serious illness and doubts about the self-care4.
In this context, it is essential the role of the nursing staff, who must provide care aimed at the physical aspect of the individual and also support and appropriate guidance to ease the uncertainties and possible side effects of the procedure4.
Thus, nursing professionals should guide this patient about the post-surgical care related to urinary catheter, such as warm baths, often washing the penis tip, using ointment and loose clothing. They must also explain about recovery time, the evolution of this period, and warn about the possible complications of surgery, such as urinary incontinence and erectile dysfunction5. Moreover, family and/or patient caregivers should be included in these guidelines on self-care6.
Thus, in view of the increasing number of patients undergoing prostate surgery and the need for an individualized and unique care, it is essential that nursing staff knows about the care provided to patients in the postoperative prostatectomy. Such knowledge can improve the conduct of nurses and guide them to achieve a higher quality of care, capable to meet the needs of this population in a period that demands quite unique attention.
Based on the above, the following question arose: are the care provided by the nursing team to prostatectomized patients at a university hospital in a city in northeastern Brazil in line with those recommended by the literature?
In order to address this question, the aim of this research was to identify the activities of nurses working in the urology unit that provide care to patients in postoperative period of prostatectomy and compare them to what is presented in the literature.
LITERATURE REVIEW
The prostate surgery is commonly recommended to patients with BPH or with prostate cancer. Among the surgical approaches used in the treatment of this gland disorders, there is highlight for transurethral resection (TURP), transurethral incision (TUIP), laparoscopic radical prostatectomy and open surgical removal, which has three different modalities: suprapubic, perineal and the retropubic3.
The TURP is the procedure usually used, considered the gold standard, carried out through endoscopy and does require incision. For this purpose, an optical instrument is introduced through the urethra into the prostate and the gland is removed in small portions. Some of the potential complications of this procedure are erectile dysfunction, retrograde ejaculation and the transurethral resection syndrome, which, although it occurs in 2% of men who undergo this treatment, can cause lethargy, confusion, hypotension, tachycardia, nausea, vomiting, headache, muscle spasms and seizures3,7.
The TUIP, just like the TURP, is performed through an instrument inserted into the urethra until the prostate, where two incisions are made in order to reduce the pressure on the prostatic urethra. It is a procedure performed on outpatient clinics and is characterized by presenting smaller rate of complications than other procedures3.
Laparoscopic radical prostatectomy is a minimally invasive procedure in which patients experience less bleeding, shorter hospitalization and quicker return to usual activities. However, due to the inability of the surgeon to palpate the prostate at the time of surgery, there may be impairment of cavernous nerves, which may cause erectile dysfunction3,8.
In open surgical removal, the prostate is completely removed. For this technique, there are three different methods, namely: suprapubic, perineal and retropubic prostatectomy. These conducts differ from one another with respect to the location of the incision and post-surgical complications3.
In the first method, an incision is made directly into the bladder to remove the gland. Difficult-to-control bleeding may occur as a complication. In the second type, the incision is made in the perineal region, which increases the chances of infection, since the incision is near the rectum. It may also occur incontinence, impotence and rectal injury. In retropubic prostatectomy, the surgeon removes the prostate between the pubic arch and the bladder, without penetrating it. It may occur early infection in the retropubic space as a complication 3.
Added to the complications related to surgical procedures, there are emotional conflicts with which the patient may cope after surgery, such as fear, helplessness, anger and sadness. These feelings have a close relationship with the expectations and doubts arising from the therapy effectiveness and the possible side effects existing 4.
Therefore, keeping in view the occurrence of emotional conflicts and possible complications during the postoperative of prostatectomy, the nursing staff should draw appropriate care to this population in order to minimize these complications and promote recovery of physical and psychological health of patients undergoing this treatment.
Therefore, according to the literature, the nurse must provide care such as: psychological support, in order to identify the needs of patients, providing support and/or referring to other more specialized sectors; guidance on the postoperative and also guidance on surgical recovery, post-surgical care and its possible complications; treatment of erectile dysfunction, of incontinence, of hyponatremia and pain treatment9.
METHODOLOGY
This is a descriptive study conducted in a university hospital located in a city in northeastern Brazil. That is a large public hospital that provides service to the Unified Health System (SUS), and it is a reference hospital of medium and high complexity for the entire state. It has 191 hospital beds, distributed in the sectors of Intensive Care Unit (ICU), transplantation unit and wards.
The study population consisted of all nursing professionals (nurses, nursing technicians and nursing assistants) in the hospital. The sample was composed of nursing professionals who worked in the hospital's urology wards, totaling 18 professionals gathered by consecutive sampling.
Inclusion criteria were: working in nursing care to prostatectomized patients and being working in the months of data collection. It was determined as exclusion criteria the noncompliance with the aforementioned inclusion criteria.
To collect the data it was used a semi-structured questionnaire with open and closed questions concerning sociodemographic data of professionals and patient care provided in the postoperative of prostatectomy. To this end, the variables used were: age, sex, professional training, years of service as a nursing professional and working in the urology unit and whether the professional had received some training.
The other questionnaire variables were the categories related to nursing care in the postoperative of prostatectomy, which were pre-established by the researchers, by means of prior literature search. The categories concerning care were: guidance on the postoperative period; treatment of urinary incontinence; treatment of erectile dysfunction; pain treatment; psychological support; and treatment of hyponatremia.
To this end, nurses were asked about performing any of these care; when the answer was positive, the activities for each category of care were described in full. Data were collected in August and September 2011.
Nursing activities reported by professionals were grouped by similarity of words and meanings of terms and then presented in absolute number of citations. Therefore, such activities were compared to nursing care evidenced by the literature in order to identify different words with similar meanings; this method was used in a similar study10. These terms were subsequently gathered by similarity of content and grouped in the six predetermined categories. It is noteworthy that for each category the absolute and relative numbers of citations of each nursing care provided by the professional were calculated. For this, the data were submitted to descriptive statistical analysis, and the relative and absolute frequencies were exposed, and there may be multiple answers.
In this research the ethical and legal principles to be followed in investigations involving human beings were respected. The study was evaluated by the Ethics Research Committee of the hospital and approved under protocol number 590/11 and Certificate of Presentation for Ethical Consideration No. 0031.0.294.000-11.
RESULTS AND DISCUSSION
Regarding the sociodemographic characterization of the research participants, the ages ranged from 20 to 57 years old, being the age of 41 the most frequent, represented by 3 (16.6%) professionals. About 18 (100%) professionals were female and most of them, 11 (61.1%), worked in the institution as nursing technicians. Mid-level nursing professionals make up a significant and representative number in health institutions, and are therefore responsible for numerous patient care11.
The length of service as a nursing professional ranged from 41 days to 28 years, and there was prevalence of the time of one year, referring to three (16.6%) people. As a professional working in the urology unit, the time ranged from 15 days to 10 years. Most participants, 17 (94.4%), did not receive in-service training.
In the first category, guidance on the postoperative period, the nursing staff reported 15 types of nursing care. Resting was the main advice described by them. In contrast, among 15 types of care cited, only 3 (16.6%) are in agreement with the literature, namely: clarification of postoperative complications, cited by only three professionals, encouraging fluid intake and care with bladder catheter, cited by only two investigated professionals.
The prostate surgery raises many questions and complex issues for the patient and their families because it involves functional, urological and sexual aspects. Therefore, the healthcare team, especially nurses, should conduct orientation and communication methods to facilitate the recovery of patients. The guidelines on the postoperative period for the patient and their companions (spouse/caregiver) are extremely important for proper recovery9.
In addition, the postoperative period of prostatectomy is sometimes difficult to be experienced as the patient may experience complications such as infection, scar tissue blockage, bladder spasms, pain, urinary incontinence and sexual dysfunction. So he and his spouse/caregiver must be clearly informed as they are often focused only in the surgical procedure that is the hope of healing, without regarding to what may come later12.
With respect to fluid intake, in particular water, when it is drank in adequate amount, it prevents the formation of blood clots which, if present, may block the urinary catheter and cause pain. Thus, the patient must be stimulated to increase fluid intake, particularly in the first month after surgery and while there is hematuria13. In addition, adequate water intake prevents dehydration, which is a nursing problem reported by study case with prostatectomized patient14.
It is common that all prostatectomized patients use indwelling urinary catheter (IUC) in the first weeks after surgery. Although this catheter brings benefits, it can cause physical and emotional harm, such as urinary tract infection (UTI), anger and frustration. Thus, nurses should explain how the patient and their caregivers must cope with the IUC and help them to accept it13.
In the second category - treatment of urinary incontinence – the main nursing activity was to provide the patient with the use of diapers. However, this type of activity does not act directly on the cause of the problem, it is only a palliative. In addition, a study on self-perception of the elderly about using diapers when hospitalized showed, as the main feelings related to their use, discomfort, change in self-esteem and aversion to the diaper. In this sense, as a conclusion, the study asserts that the use of diapers involves not only issues related to the need for their use, but also questions about how its use reflects both physically and emotionally in the lives of those who use them15.
In this respect, the nursing staff of this study should reflect and relate better their conducts to their customer profile, having in mind the importance of evaluating with better accuracy the customer context and the existence of other techniques that can be used for this problem, considering the self-esteem problems inherent in this population.
Thus, the care regarding the implementation of perineal exercises, found in the literature as a form of treatment for the problem at hand, was reported by only one nursing professional. These exercises are a non-invasive way to correct urinary incontinence that directly affects the quality of life of prostatectomized individuals 16. The literature states that such exercises are in fact the most efficient option for the treatment of incontinence, as they present positive results in practice 17.
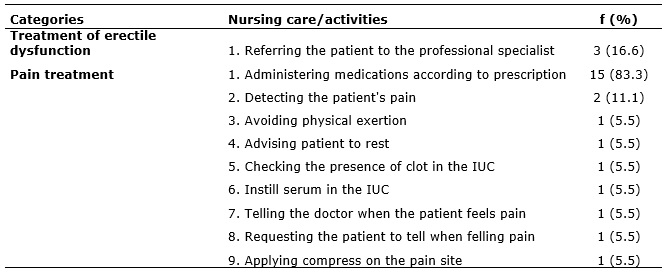
The categories treatment of erectile dysfunction, in which only a type of care was reported, and pain treatment, in which the main nursing care was the medication administration according to the medical prescription, are presented in Table 1.
TABLE 1: Nursing activities/care: treatment of erectile dysfunction and pain management in prostatectomized patients. Natal/RN, 2011.
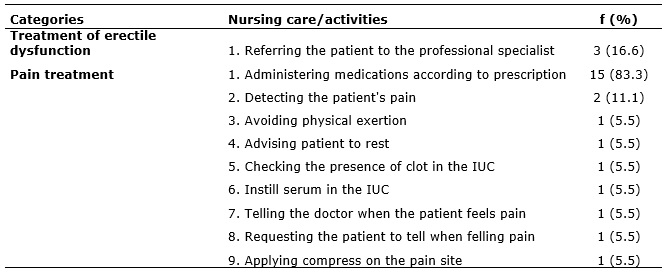
In the category treatment of erectile dysfunction, the only nursing care quoted was referring the patient to the specialist professional. Erectile dysfunction is common in prostatectomized patients, affecting at least half of patients with prostate cancer. This problem usually occurs as a result of damage to nerves and blood vessels wrapped in the prostate. Among the consequences of this physical damage, it is identified depression, anxiety, relationship conflict and loss of self-esteem18, so the nurses must intervene to solve this problem, not only referring the patient to another professional, but assuming their autonomy to intervene.
In this situation, the nursing professional can show their willingness to clarify questions; explaining the nature of erectile dysfunction; advising on possible treatments for the problem, such as the use of phosphodiesterase inhibitors, intraurethral suppositories, penile injection, vacuum device and penile prosthesis; encouraging different forms of satisfaction between the couple, for example, by increasing affectionate expressions without requiring sexual contact9.
The category pain management presented nine types of care cited by professionals participating in this research. Of these, only one was similar to the literature: medication administrations according to medical prescriptions, as reported by 15 (83.3%) participants. According to the literature, it should be administered opioids and/or nonsteroidal anti-inflammatory drugs. However, few studies address the treatment of pain as a nursing activity, which indicates that these professionals may not be considering this common postoperative change as significant13,19. In contrast, pain is an important nursing diagnosis, which is commonly identified in patients undergoing postoperative period and can reverberate on psychological and physiological levels if not healed14.
Categories of psychological support, treatment of hyponatremia and their respective care are described in Table 2.
TABLE 2: Nursing activities/care: psycological support and treatment of hyponatremia in prostatectomized patients. Natal/RN, 2011.
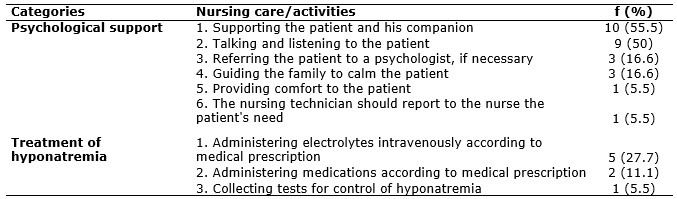
The category psychological support presented six types of care, and the most reported care was providing support to the patient and his companion, by 10 (55.5%) participants. Among the types of care, only one was not cited in the literature: nursing technicians should report to nurses the patient's need. This finding may be related to little distinction between different categories of nursing professionals.
Study on the impact of nursing care in men after prostate treatment indicated that 81% of men surveyed had some unmet care need, and, among these, it was included mainly the support to psychological and sexual health, and related guidelines20. Thus, nursing staff can identify and discuss the psychological support needs of the patient, listen to their troubles and needs, provide emotional support, counseling or referral to other resources and encourage their participation in support groups9.
In a systematic review on how the telephone follow-up to patients after prostatectomy can influence the improvement of the clinical and psychological effects, it was found that this type of monitoring generates benefits to the patient, and therefore is a recommended tool for nurses, in order to improve the quality of life of patients experiencing this context21.
In the second category, related to the treatment of hyponatremia, 5 (27.7%) professionals reported as nursing care the need to administer electrolytes intravenously according to medical prescription. However, in this category, only three activities were cited by professionals. Therefore, the report of few activities for the treatment of hyponatremia was identified, and these were found in only one study in the literature22.
However, hyponatremia is a complication that can occur in the postoperative period of prostatectomy and thus the nursing staff must be able to know the pathophysiology and the signs and symptoms of this change in order to reduce complications and improve patient recovery. In a study on the creation and implementation of an Enhanced recovery after surgery pathways, an internationally implemented tool, with a view to provide guidance to evidence-based decision making, with the ultimate goal to homogenize the assistance without compromising the quality of care in radically prostatectomized patients, it was identified the association between this tool and the reduction of hospital stay and the rates of postoperative complications and readmissions 23. In this sense, the professionals responsible for identifying, preventing and treating complications related to postoperative prostatectomy should look for tools that support their practice.
Study asserts that to prevent such injury, nursing staff should replace, as soon as possible, the catheter irrigation solution by normal saline solution, since excess irrigation during trans and postoperative period is one of the causes of hyponatremia22.
Therefore, from the aforementioned, the nurse should carry out activities aimed at the needs of each patient, providing holistic care, considering the individual as a complex being, inserted in a particular social context.
CONCLUSION
It is concluded that nursing professionals have emphasized the guidelines in postoperative period regarding the treatment of urinary incontinence, pain treatment and psychological support. Some of the mentioned activities composing these types of care were not in agreement with the literature.
This result demonstrates the limited knowledge of these professionals in certain specific aspects of care to prostatectomized patients in postoperative period. This might be result from the reality found in this study, in which most of those nursing professionals interviewed had not received training in urology service. Thus, it is emphasized the importance of specific training to the urology unit and greater knowledge of professionals about the specific needs of this clientele.
Thus, it is of paramount importance to know the activities performed by the nursing team to the patient in postoperative period of prostatectomy, with a view to identify possible shortcomings in their implementation and thus promoting continuing education in order to provide continuous improvement of recommended care for this clientele.
Among the limitations of the study there is highlight for the small sample size and a unique scenario, which prevent the generalization of findings.
REFERENCES
1.Ministério da Saúde (Br). Instituto Nacional de Câncer (INCA). Estimativa 2012: incidência de câncer no Brasil. Brasília (DF): Ministério da Saúde; 2012.
2.Santos A, Gonçalves N, Santos MJ, Rolo F, Macedo A. Avaliação de práticas e conhecimentos dos homens relativamente a doença prostática, em Portugal - Estudo epidemiológico. Acta Urol Belg. 2007; 24 (4): 25-32.
3.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Tratado de enfermagem médico cirúrgica. 12ª ed. Rio de Janeiro: Guanabara Koogan; 2011.
4.Napoleão AA, Caldato VG, Petrilli Filho JF. Diagnósticos de enfermagem para o planejamento da alta de homens prostatectomizados: um estudo preliminar. Rev Eletr Enf. [internet] 2009 [citado em 19 set 2012]; 11 (4): 286-94. Disponível em: http://www.fen.ufg.br/fen_revista/v11/n2/v11n2a08.htm.
5.Burt J, Caelli K, Moore K, Anderson M. Radical prostatectomy: men's experiences and postoperative needs. J Clin Nurs. [internet] 2005 [cited in 2012 Aug 12]; 14: 883-90. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2702.2005.01123.x/pdf.
6.Vianna MC, Napoleão AA. Reflexões sobre cuidados de enfermagem para a alta de pacientes prostatectomizados. Ciênc cuid saúde. 2009; 8 : 269-73.
7.Portes TA, Bernardo PLA, Faccio Júnior FN. Ressecção transuretral da próstata (RTUP): complicações transoperatórias e pós-operatórias em hospital universitário. Arqu Ciênc Saúde. 2004; 11: 199-204.
8.Nunes P, Rolo F, Mota A. Prostatectomia radical e atividade sexual. Acta Urol. 2004; 21(1): 15-31.
9.Santos DRF, Silva FBBL, Saldanha EA, Lira ALBC, Vitor AF. Cuidados de enfermagem ao paciente em pós-operatório de prostatectomia: revisão integrativa. Rev Eletr Enf. [internet] 2012 [citado em 19 set 2012]; 14 (3): 690-701. Disponível em: http://www.fen.ufg.br/fen_revista/v14/n3/pdf/v14n3a27.pdf.
10.Napoleão AA, Carvalho EC. Aplicabilidade de intervenções prioritárias da NIC para o diagnóstico de enfermagem desobstrução ineficaz de vias aéreas. Cogitare enferm. 2007; 12 (1): 9-19.
11.Abraão SR, Bezerra ALQ, Branquinho NCSS, Paranaguá TTB. Caracterização, motivação e nível de satisfação dos técnicos de enfermagem de um hospital universitário. Rev enferm UERJ. 2010; 18 :253-8.
12.Phillips C, Gray RE, Fitch MI, Labrecque M, Fergus K, Klotz L. Early postsurgery experience of prostate cancer patients and spouses. Cancer Pract. 2000; 8 (4): 165-70.
13.Mata LRF, Carvalho EC, Napoleão AA. Validação por peritos de intervenções de enfermagem para a alta de pacientes submetidos à prostatectomia. Texto & contexto enferm. 2011; 20: 36-44.
14.Saldanha EA, Fernandes MICD, Medeiros ABA, Frazão CMFQ, Costa IA, Lira ALBC. A teoria de Callista Roy, a NANDA-I e o cuidado ao paciente prostatectomizado. Rev enferm UERJ. 2012; 20:764-70.
15.Alves LAF, Santana RF, Schulz RS. Percepções de idosos sobre a utilização de fraldas durante a hospitalização. Rev enferm UERJ. 2014; 22:371-5.
16.Kim HS. Development and evaluation of self-care agency promoting programme for prostatectomy patients. J Urol Nurs. 2011; 5 (1): 34-44.
17.Honório MO, Santos SMA. A rede de apoio ao paciente incontinente: a busca por suporte e tratamentos. Rev enferm UERJ. 2010; 18:383-8.
18.Schover LR, Kaaij MVD, Dorst EV, Creutzberg C, Huyghe E, Kiserud CE. Sexual dysfunction and infertility as late effects of cancer treatment. Eur J Cancer. 2014;12: 41-53.
19.Mata LRF, Napoleão AA. Intervenções de enfermagem para alta de paciente prostatectomizado: revisão integrativa. Acta Paul Enferm. 2010; 23: 574-9.
20.Cockle-Hearne J, Charnay-Sonnek F, Denis L, Fairbanks HE, Kelly D, Kav S. et al.The impact of supportive nursing care on the needs of men with prostate cancer: a study across seven European countries. Br J Cancer. 2013; 109: 2121–30.
21.Mata LRF, Silva AC, Pereira MG, Carvalho EC. Telephone follow-up of patients after radical prostatectomy: a systematic review. Rev Latino-Am Enferm. 2014; 22:337-45.
22.Eaton J. Detection of hyponatremia in the PACU. J Perianesth Nurs. 2003; 18: 392-7.
23.Abou-Haidar H, Abourbih S, Braganza D, Al Qaoud T, Lee L, Carli F. et al. Enhanced recovery pathway for radical prostatectomy: Implementation and evaluation in a universal healthcare system. Can Urol Assoc J. 2014; 8:11-2.