RESEARCH ARTICLES
Sociodemographic and clinical characteristics of institutionalized older adults: contributions to nursing care
Cíntia Lira BorgesI; Maria Josefina da SilvaII; Jorge Wilker Bezerra ClaresIII; Jéssica de Menezes NogueiraIV; Maria Célia de FreitasV
I
Nurse. Master from the Post-graduate Program Clinical Care in Nursing and Health of the State University of Ceará. Member of the Research Group Nursing,
Education, Health and Society. Fortaleza, Ceará, Brazil. E-mail: cintialiraborges@yahoo.com.br
II
Nurse. PhD in Nursing. Associate Professor of the Graduate Program in Nursing and of the Post-graduate Nursing Program of the Federal University of Ceará.
Fortaleza, Ceará, Brazil. E-mail: mjosefina@terra.com.br
IIINurse. Master from the Post-graduate Program Clinical Care in Nursing and Health of the State University of Ceará. Member of the Research Group Nursing,
Education, Health and Society. Fortaleza, Ceará, Brazil. E-mail: jorgewilker_clares@yahoo.com.br
IV
Nurse. Master from the Post-graduate Program Clinical Care in Nursing and Health of the State University of Ceará. Member of the Research Group Nursing,
Education, Health and Society. Fortaleza, Ceará, Brazil. E-mail: jessicademenezesn@gmail.com
V
Nurse. PhD in Fundamental Nursing. Associate Professor of the Graduate Program in Nursing and of the Post-graduate Program Clinical Care in Nursing and
Health of the State University of Ceará. Member of the Research Group Nursing, Education, Health and Society. Fortaleza, Ceará, Brazil. E-mail: celfrei@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2015.4214
ABSTRACT
This cross-cutting, descriptive study described the sociodemographic and clinical characteristics of institutionalized older adults. Fifty-four elderly residents at a long-stay institution in Fortaleza, Ceara State, Brazil, participated by responding to a form in 2011. Study population mean age was 72.4±8.5 years; they were predominantly elderly males (61.1%), single (46.3%), illiterate (46.3%) and retired (77.8%). Institutionalization was expressed as: 51.9% had lived in the institution less than five years; 29.6% were former street dwellers; and 72.2% received no visits. Clinical characteristics included: 81.5% had a chronic disease; 83.3% made continuous use of medication; and blood pressure and blood glucose levels were controlled in 57.4% and 81.1% participants, respectively. Frailty profile was given as 74.1% of the elderly being fragile. These data can support the actions of nurses in promoting more effective and individualized care for institutionalized elderly.
Keywords: Elderly; homes for the elderly; population characteristics; nursing.
INTRODUCTION
Population aging is a hard phenomenon in Brazil and worldwide, with significant impact on economic and health structure of societies, due to the prevalence of chronic-degenerative diseases among the elderly, which increases the demand for health services and specific public policies for this group1.
In addition, there are the contemporary changes in living arrangements that helps reducing the availability of family support and failure to care for the elderly, which has resulted in increased demand for long-term care facilities for the elderly (LTCF) as alternative to housing and permanent care to this age group of the population2.
However, these institutions still represent a challenge, since the inherent changes of aging and the pre-existing diseases may be aggravated by institutionalization, generating different levels of dependency in the elderly. It is noteworthy that even the independent elderly, when institutionalized, can become dependent, due to difficulties to accept and to adapt to new conditions of life, and due to the lack of motivation and encouragement that is common in this environment3.
Knowing the characteristics of the population to whom care is provided is critical to the redirection of health care of institutionalized elderly, subsidizes nursing actions, based on the specific demands of this group, making it possible to develop activities to promote health and prevent diseases, with a view to avoid dependence and functional disability.
Given these considerations, the investigation of the characteristics of the institutionalized elderly is justified by the need to plan and carry out assistance and educational activities within the LTCF, for the prevention of physical and mental dependence in that group. Thus, the study aimed to describe the sociodemographic and clinical characteristics of elderly residents in a LTCF in Fortaleza/CE, Brazil.
LITERATURE REVIEW
The LTCF are governmental or non-governmental residential institutions, aimed both to independent elderly in a situation of lack of income and/or family and to dependent elderly, who need long-term care4.
In European countries, it is observed that about 20% of the elderly population with some disability lives in long-term care facilities5-6. In Brazil, census survey conducted from 2007 to 2009 found that 84,000 seniors live in these institutions, which represents less than 1% of the country's elderly population4.
Short supply of institutions, high costs, prejudices and stereotypes associated with care to elderly preferentially performed by family are among the factors that can explain the low proportion of Brazilian elderly living in LTCF compared to developed countries. However, it is believed that the demand for LTCF tends to grow in coming years, due not only to the contemporary aging population, but also to changes in family arrangements and to poverty that affects a major part of Brazilian families7.
For their full operation, these institutions require a team of nurses, nursing technicians, physician, nutritionist, psychologist, social worker, physical therapist, physical educator and caregivers8. The nurses who work at LTCF develop a joint work with the other members of the multidisciplinary health team, directed to effective care of the elderly, through educational, welfare, management and research activities.
It is noteworthy that the health care to institutionalized elderly is primarily intended to maintain a good health and to postpone the most the active life in this environment, with autonomy and physical, psychological and social independence. Therefore, actively participating in the social context and remaining firm with autonomy is essential for the elderly. Besides, this contributes to the health and well-being9.
In this regard, special attention should be given to the institutionalized elderly in order to prevent functional disability. For this to happen, it is necessary that nurses know the characteristics of the elderly and carry out situational diagnosis studies in order to have essential knowledge to improve care offered within the LTCF through the planning of actions focusing on local demands, which will result in a more effective and individualized performance.
METHODOLOGY
This is a descriptive, cross-sectional study with quantitative approach, carried out at a public LTCF in the city of Fortaleza/CE that is integrated with the Secretariat of Labor and Social Development, which shelters abandoned elderly, victims of violence or in any other socially vulnerable condition.
For the sample, the following inclusion criteria were used: being 60 years old or older, being able to answer questions and being willing to participate. Participants were 54 elderly men and women, in compliance with the pre-established inclusion criteria. We highlight that all participants signed or placed their fingerprints on the Informed Consent Form.
Data were collected during March 2011, after approval of the project by the Research Ethics Committee of the Federal University of Ceara (protocol 164/10).
The collection was performed daily, in the morning and the afternoon, according to the researcher's schedule. Data were obtained by applying structured forms, in a private atmosphere inside the institution, individually, and had an average duration of 20 minutes, besides the search for information in the medical records of the elderly.
For information on the socio-demographic profile of the elderly, the selected variables were gender, age, education, marital status, occupation, time and reason for the institutionalization and social support. For the clinical characteristics of the sample we collected anthropometric physiological and biochemical variables, chronic diseases, use of medication and fragility levels.
The following anthropometric and physiological variables were selected: weight, height, body mass index (BMI) and blood pressure. The glucose level was the biochemical variable analyzed.
For the variables BMI, blood glucose and blood pressure we applied the parameters established in Primary Care Booklet # 19, of the Ministry of Health10, as follows: BMI classified as low weight (≤ 22 kg/m2), normal weight (23-26 kg/m2) or overweight (≥ 27 kg/m 2); glucose levels classified as hypoglycemia (<80 mg/dL), good glycemic control (80-159 mg/dL), acceptable glycemic control (160-179 mg/dL) or poor glycemic control (≥ 180 mg/dL); blood pressure classified as normal (<120 mmHg x 80), pre-hypertension (120-139 x 80-89 mmHg), stage I hypertension (140-159 x 90-99 mmHg) or Stage II hypertension (mm Hg ≥ 160 x 100 ) - it is noteworthy that when the systolic and diastolic pressures are located in different categories the greatest value should be considered for classification of stage.
The information on chronic diseases and use of medications were obtained by collection in the medical records.
The frailty level was measured using the Edmonton Frail Scale (EFS), validated for Portuguese language, and consisting of nine domains, distributed in 11 items with scores from 0 to 17 points; categorizing as no frailty (0-4 points) apparently vulnerable (5-6 points), mild frailty (7-8 points), moderate frailty (9-10 points) or severe frailty (≥ 10 points), and the greater the score, the higher the level of frailty 11.
Data collection was conducted in two stages. First, we performed the survey of demographic data and application of EFS; then the anthropometric, physiological and biochemical evaluation. This evaluation was carried out as follows: body weight in kilograms was measured with barefoot elderly in anthropometric scale (Britania®), duly tested and calibrated, accurate to 0.1 kg, intended exclusively for this research; the height was measured in meters with inelastic measure tape, graduated in 0.5 cm, with barefoot elderly, their heels together and looking at the horizon; capillary blood glucose was measured in mg/dL and verified without the requirement of the elderly to be fasting, and we used glucometer Accu-Check® Active; blood pressure was measured in the right arm in the sitting position.
The results were processed and tabulated in the Statistic Package for Social Science version 19.0. For processing the data, we opted for the use of descriptive statistics, with relative and absolute numbers, presented in the form of table.
RESULTS
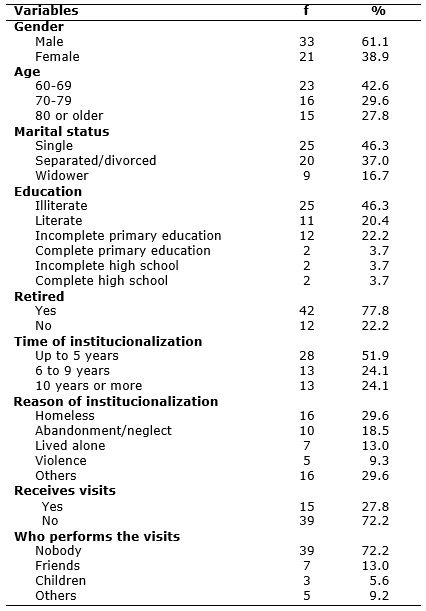
Participants were 54 institutionalized elderly who met the inclusion criteria of the study, 33 (61.1%) men and 21 (38.9%) women. Ages ranged from 60 to 90 years old, averaging 72.4 years old and with standard deviation of 8.5 years old. Regarding marital status, there was a predominance of single participants (46.3%), and there were no cases of elderly people who declared themselves married. Schooling was low; seniors were predominantly illiterate, 25 (46.3%). As regards occupation, 12 (22.2%) were not retired, according to Table 1.
TABLE 1: Distribution of institutionalized elderly, according to sociodemographic characteristics. Fortaleza/CE, Brazil 2011. (N=54)
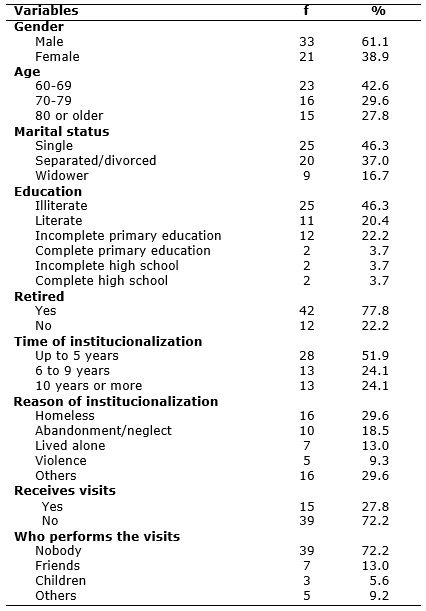
Regarding the characteristics of institutionalization, 28 (51.9%) elderly had been living in LTCF for less than five years. The main reasons given for the institutionalization were: being homeless, 16 (29.6%); and abandonment/family neglect, 10 (18.6%). As for the social support prior to the institutionalization, 39 (72.2%) seniors said they did not receive outside visits, over 15 (27.8%) that had been receiving. Friends are the main visitors for 7 (13%) elderly, according to Table 1.
Clinical characteristics of the institutionalized elderly are listed in Table 2. Regarding the BMI, it was observed that 12 (22.2%) and 11 (20.4%) elderly were classified as low weight and overweight, respectively. Most of the surveyed seniors (81.5%) had at least one chronic disease, with an average of 1.28 illness and standard deviation of 0.94 illness for each elderly. It was identified in the medical records a variety of diseases, and hypertension (45.5%) and diabetes (20.4%) were the most frequent. Despite the higher prevalence of these diseases, both blood pressure and blood glucose were controlled for 31 (57.4%) and 43 (81.1%) elderly, respectively.
TABLE 2: Distribution of institutionalized elderly, according to clinical characteristics. Fortaleza/CE, Brazil, 2011. (N=54)
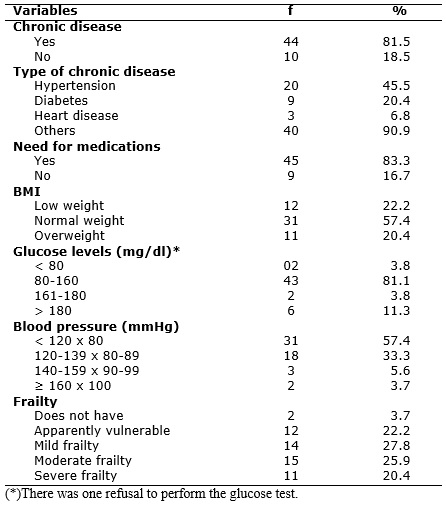
Regarding the consumption of drugs, 45 (83.3%) elderly need continuous use of medication due to existing morbidities, of whom 20 (44.4%) make use of five to eight different drugs, with the highest prevalence for psychotropic and clinical medicines, used for 34 (63%) elderly, each. Regarding the profile of frailty 40 (74.1%) were frail elderly, ranging from mild to severe frailty, and 12 (22.2%) were apparently vulnerable, according to the Table 2.
DISCUSSION
In this research, there was prevalence of men (61.1%), a fact also confirmed in a study with institutionalized elderly in the South the country 12. These data differ from other national13 and international studies14,15 that evidenced a female predominance in this type of facility. This divergence may be related to the fact that the LTCF where this study was developed shelters, in most cases, homeless, indigent, lost and abandoned elderly, with no family and social reference; in Brazil, this situation is experienced predominantly by men16.
With respect to the educational level of the elderly, there is a high prevalence of people with little or no schooling. This finding was expected, since these seniors lived their childhood at a time when education was undervalued17. In addition, many were homeless and/or coming from socially vulnerable communities with precarious social and economic indicators, which justifies the low levels of education.
Socioeconomic aspects are related to the health condition and the pattern of morbidity and mortality of the population and should be considered during the health monitoring and the planning of care strategies by health professionals, particularly by nurses, subsidizing health actions directed to the needs of the institutionalized senior citizens.
Moreover, it is possible to infer that the unfavorable socioeconomic conditions may have contributed to the institutionalization of these elderly, since, currently, this process has been influenced by changes in living arrangements added to the failure of families in caring for their elderly. In this sense, a study found that the presence of family conflicts, financial problems and not having family were the main reasons for the institutionalization of subjects aged 60 years old or older18.
The important quantity of single seniors (46.3%), of former homeless (29.6%) and of victims of abandonment (18.6%), and the reduced number of visits received denote the fragile family and/or social support network of the elderly, which is aggravated by the restriction of social life and by the time of institutionalization.
Social support networks are crucial to improve the quality of life of older people, allowing to establish social relationships and to strengthen the use of coping strategies for the challenges of old age19. Thus, the nurse inserted in this scenario has a fundamental role in building a support structure for the institutionalized elderly, by providing social, emotional and affective support, benefiting the health and physical and mental well-being of the individuals under their care. They should also, whenever possible, seek strategies to reintegrate that aged person to their family nucleus, stimulating the responsibility of care to the elderly by the family.
On the clinical characteristics, it was found that the vast majority of the elderly (81.5%) had at least one chronic disease, most notably cardiovascular diseases, including high blood pressure and diabetes. These findings are similar to other studies with elderly living in LTCF13.
Cardiovascular disease is a high frequent illness condition that endangers population aging, since, in certain situations, it has resulted in the loss of autonomy and/or independence of the elderly. Moreover, it is the leading cause of death among the elderly20. Thus, the presence of hypertension and diabetes in this group deserves attention because of the greater vulnerability to cardio/cerebrovascular complications determined by the association between clinical conditions and other factors accumulated over time.
Although hypertension and diabetes have shown higher percentage in this population, compared to the other mentioned diseases, it has been found that the blood pressure and blood glucose levels, in most cases, were within acceptable limits, which may be result of the use of specific medications to control these morbidities.
It is noteworthy that, in the studied LTCG, control of medication is the responsibility of nursing professionals, including the functionally independent elderly, reinforcing the need to prevent worsening and sequelae of pre-existing conditions, as they can result in permanent functional disabilities.
It was also found the consumption of large amount of medication by the elderly, as they reported presenting morbidities: 45 (83.3%) require continuous use of medication, of which 20 (44.4%) make use of five to eight different drugs.
The practice of polypharmacy is associated with increased risk and severity of adverse reactions, drug interactions, cumulative toxicity, medication errors, reduced adherence to treatment and increased morbidity and mortality. In this context, the nurse must be attentive to the rational use of medicines by the elderly, through the judicious obedience of the prescribed schedule so as to avoid the simultaneous administration of drugs that can interact with each other or with the diet; and to monitor the side effects of drugs related to negative outcomes in order to prevent and minimize adverse events, contributing to the use of medicines in a safer manner by institutionalized elderly21.
The nurse must have knowledge of pharmacology and be able to detect iatrogenic complications in the elderly population. In addition to the appropriate obedience to the schedule of medications, this professional must maintain dialogue with the medical staff in cases of need to change the medication, because the elderly may experience side effects or adverse reactions, and one of the nursing tasks is to observe the occurrence of undesirable effects. Nurses should also always be suspicious of the use of polypharmacy, performing multidimensional assessment of the elderly by detecting needs/health problems that indicate the actual accuracy of the medication; being aware of the schedule of meals and interactions with medications of chronic use, as well as the inclusion of medications, such as antibiotics and anti-inflammatory, and possible interactions.
We highlight the identification, after detected by the nursing diagnoses, of the risk that the drug may be causing the body. For example, the patient with nursing diagnosis of constipation has a number of pharmacological factors associated that can cause this problem. Therefore, it is essential that during the systematization of nursing care and the development of clinical practice, nurses realize the function of these medications and how they may be contributing to the enhancement of negative diagnosis, concurrently, and can interact with the doctor, organizing a care plan in order to replace or avoid that medication for the re-stabilization of the clinical picture.
Paying attention to the damage arising from the continued use of drugs and polypharmacy to the quality of life of the elderly, nurses, during their clinical practice, can develop strategies that enable healthy behaviors and that can possibly decrease the overuse of drugs, with a view to welfare, quality of life, autonomy and improvement of the health status of institutionalized elderly.
In the evaluation of BMI, it was verified important frequency of elderly with imbalance in nutritional status, with percentages of 22.2% for low weight and 20.4% for overweight. Similar results were found in a study of 42 institutionalized elderly in São Paulo that found that 21.4% of the elderly were classified as low weight and 33.4% as overweight22.
The problems associated with the nutritional status of the elderly can accelerate the emergence of weaknesses and vulnerabilities, hindering the recovery of the elderly and reducing significantly their lifetime, especially in the presence of chronic diseases.
Thus, assessment of nutritional status is an important tool for the diagnosis of health and nutrition, promoting educational and dietary guidelines, as well as the monitoring of therapeutic interventions in older people23. Therefore, the nutritional status as an essential element for assessing the health of the elderly should be investigated during the nursing consultation, in order to prevent installation problems due to nutritional deficiencies.
Regarding the profile of frailty, 74.1% and 22.2% of the elderly were frail and apparently vulnerable, respectively. These data confirm the results of a study of 100 elderly patients from a clinic in Rio Grande do Sul State, which identified the presence of some degree of frailty in 84% of the sample 24.
Frailty is defined as a clinical syndrome characterized by decreased reserve and by reduced resistance to stressors, resulting from a cumulative decline in physiological systems (especially neuroendocrine, immune and musculoskeletal), causing vulnerability to adverse conditions among the elderly. Thus, it is considered as a significant risk factor for falling, disability, hospitalization and death among elderly25.
In this context, it is reinforced the importance of multidimensional assessment of the elderly, as a possibility to detect the risk factors for frailty and to act preventively in the emergence and/or worsening of this condition11. It is also noteworthy that the care to frail elderly and to vulnerable elderly should be performed by an interdisciplinary team that must be prepared to identify and intervene in health problems associated with frailty in the elderly, not only aimed at rehabilitation, but mainly at the establishment of preventive and educational measures for the health of institutionalized seniors24.
When the nurse is able to conduct a comprehensive assessment of the elderly in a multidimensional manner, it is possible to prevent the development or worsening of frailty, minimizing hospitalizations and mortality rates in this age group26,27.
From this perspective, nursing care to the institutionalized elderly that are often weakened or going through a weakening process should provide autonomy and independence, which can optimize the provision for resilience, helping to ensure that aged people are active and able to face adversity. Moreover, besides fighting against physical diseases, institutionalized elderly also face with losses of family roles that interfere with their social, mental and psychological dimensions. For this it is possible to develop care plan or implement nursing interventions from prior knowledge of the social and cultural characteristics of elderly residents in LTCF, recognizing their specificities, in order to encourage their independence, respecting their autonomy, their life story, expectations on the institutionalization process and their limitations, and encouraging their integration into the group, which will result in better quality of life for these subjects.
CONCLUSION
The results obtained allowed to know the sociodemographic and clinical characteristics of institutionalized elderly. The findings draw attention to the need for care performed by a multidisciplinary team, especially nurses, who must make use of knowledge about the characteristics of the elderly to promote an individualized, more effective and efficient care.
Importantly, we highlight as a limitation of the study the fact that it was carried out only with functionally independent elderly of a single institution, translating a specific reality. Thus, this methodology can be replicated in other situations and the realization of such studies should be encouraged, including the elderly with different levels of dependency in order to obtain safer and more concrete bases for planning strategies and the comprehensive care for the health of the population living in LTCF.
Finally, we hope that these findings can support the planning of effective and individualized nursing care to institutionalized elderly, based on their real needs and risk factors to health, aiming at physical, mental and social well-being of this group.
REFERENCES
1.Veras R. Envelhecimento populacional contemporâneo: demandas, desafios e inovações. Rev Saude Publica. 2009; 43:548-54.
2.Creutzberg M, Gonçalves LHT, Sobottka EA, Ojeda BS. Long-term care institutions for elders and the health system. Rev Latino-Am Enfermagem. 2007;15:1144-9.
3.Araújo MOPH, Ceolim MF. Avaliação do grau de independência de idosos residentes em instituições de longa permanência. Rev esc enferm USP. 2007;41:378-85.
4.Camarano AA, Kanso S. As instituições de longa permanência para idosos no Brasil. Rev bras estud popul. 2010; 27:232-5
5.Demographic change in the euro area: projections and consequences. European Central Bank Monthly Bulletin. 2006;49-64.
6.Giannakouris K. Ageing characterises the demographic perspectives of the European societies. Eurostat Statistics in focus 72. 2008;1-11.
7.Camarano AA, organizadora. Características das instituições de longa permanência para idosos: região Nordeste. Brasília (DF): IPEA; 2008.
8.Silva BT, Santos SSC. Cuidados aos idosos institucionalizados: opiniões do sujeito coletivo enfermeiro para 2026. Acta Paul Enferm. 2010;23:775-81.
9.Santos SSC, Silva BT, Barlem ELD, Lopes RS. The nurse role in the seniors' long permanence institution. Rev Enferm UFPE online. 2008 [cited 2012 Aug 03];2:291-9. Available from: http://www.ufpe.br/revistaenfermagem/index.php/revista/article/view/351/pdf_386
10.Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Envelhecimento e saúde da pessoa idosa. Brasília (DF): Editora MS; 2006.
11.Fabrício-Wehbe SCC, Schiaveto FV, Vendrusculo TRP, Haas VJ, Dantas RAS, Rodrigues RAP. Cross-cultural adaptation and validity of the Edmonton Frail Scale – EFS in a brazilian elderly sample. Rev Latino-Am Enfermagem. 2009;17:1043-9.
12.Carreira L, Botelho MR, Matos PCB, Torres MM, Salci MA. Prevalência de depressão em idosos institucionalizados. Rev enferm UERJ. 2011;19:268-73.
13.Aires M, Paz AA, Perosa CT. Situação de saúde e grau de dependência de pessoas idosas institucionalizadas. Rev Gaúcha Enferm. 2009;30:492-9.
14.Onder G, Carpenter I, Finne-Soveri H, Gindin J, Frijters D, Henrard JC et al. Assessment of nursing home residents in Europe: the Services and Health for Elderly in Long Term care (SHELTER) study. BMC Health Serv Res. 2012 [cited 2012 aug 30];12:5. Available from: http://www.biomedcentral.com/1472-6963/12/5.
15.Torres Camacho MJ, Vázquez Perozo M, Parellada Sabaté A, González Acosta ME. Disfagia en ancianos que viven en residencias geriátricas de Barcelona. Gerokomos. 2011;22:20-4.
16.Fundação Instituto de Pesquisas Econômicas. Principais resultados do perfil socioeconômico da população de moradores de rua da área central da cidade de São Paulo. Relatório Executivo. São Paulo: FIPE; 2010.
17.Davim RMB, Torres GV, Dantas SMM, Lima VM. Estudo com idosos de instituições asilares no município de Natal/RN: características socioeconômicas e de saúde. Rev Latino-Am Enfermagem. 2004;12:518-24.
18.Rissardo LK, Furlan MCR, Grandizolli G, Marcon SS, Carreira L. Sentimentos de residir em uma instituição de longa permanência: percepção de idosos asilados. Rev enferm UERJ. 2012;20:380-5.
19.Nardi EFR, Oliveira MLF. Conhecendo o apoio social ao cuidador familiar do idoso independente. Rev Gaúcha Enferm. 2008;29:47-53.
20.Romero AD, Silva MJ, Silva ARV, Freitas RWJF, Damasceno MMC. Características de uma população de idosos hipertensos atendida numa unidade de saúde da família. Rev RENE. 2010;11:72-8.
21.Secoli SR. Polifarmácia: interações e reações adversas no uso e medicamentos por idosos. Rev Bras Enferm. 2010;63:136-40.
22.Lehn F, Coelho HDS, Garcia MT, Scabar LF. Estado nutricional de idosos em uma instituição de longa permanência. J Health Sci Inst. 2012;30:53-8.
23.Lacerda NC, Santos SSC. Avaliação nutricional de idosos: um estudo bibliográfico. Rev RENE. 2007;8:60-70.
24.Remor CB, Bós AJG, Werlang MC. Características relacionadas ao perfil de fragilidade no idoso. Sci Med. 2011;21:107-12.
25.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty and comorbidity: implications for improved targeting and a care. J Gerontol Med Sci. 2004;59:255-63.
26.Macedo C, Gazzola JM, Najas M. Síndrome da fragilidade no idoso: importância da fisioterapia. Arq Bras Ciênc Saúde. 2008;33:177-84.
27.Pinto NBF, Vieira LB, Pereira FMV, Reis AMM, Cassiani SHB. Interações medicamentosas em prescrições de idosos hipertensos. Rev enferm UERJ. 2014; 22: 785-91.