RESEARCH ARTICLES
Health technology assessment: use of carboxymethylcellulose 2% in treating leg ulcers
Luciana Miranda RodriguesI; Beatriz Guitton Renaud Baptista de OliveiraII; Selma Rodrigues de CastilhoIII; Débora Omena FuturoIV
I
Master in Health Care Sciences at the Aurora Afonso Costa Nursing School. Specialist in Dermatology Nursing from University Gama Filho. Assistant Professor
at Souza Marques Nursing School. Nurse at the National Institute of Traumatology and Orthopedics. Rio de janeiro Brazil. E-mail: dralumiranda@yahoo.com.br
II
Vice-Coordinator of Academic Master of Health Care Sciences and Professor, Department of Fundamentals of Nursing and Management of Aurora Afonso Costa
Nursing School. Niterói, Rio de Janeiro, Brazil. E-mail: beatrizguitton@globo.com
III
PhD in Biomedical Engineering from the Federal University of Rio de Janeiro. Associate Professor of the Faculty of Pharmacy, Universidade Federal
Fluminense. Niterói, Rio de Janeiro, Brazil. E-mail: selmarc@globo.com
IV
PhD in Natural Products Chemistry from the Federal University of Rio de Janeiro. Associate Professor, Faculty of Pharmacy, Universidade Federal Fluminense.
Niterói, Rio de Janeiro, Brazil. E-mail: dfuturo@vm.uff.br
DOI: http://dx.doi.org/10.12957/reuerj.2015.4110
ABSTRACT
This therapeutic intervention study took the form of an uncontrolled clinical trial. It aimed to evaluate the cost and effectiveness of carboxymethylcellulose 2% in treating leg ulcers. A clinical evaluation instrument was applied to twenty volunteers at a university hospital in Niteroi, Rio de Janeiro State, between January and October 2010. After ninety days of treatment, the results of group A (lesions larger than 15.5 sq.in.) showed 15% reduction in lesion area. In group B (wounds smaller than 15.5 sq.in.), healing was total in 33.3% of cases. The costs were proportional to ulcer area: larger areas entailed higher costs. When this product was compared with other gels on the Brazilian market, the carboxymethylcellulose 2% produced at the university was observed to yield significant cost reductions (p<0.01). In conclusion, carboxymethylcellulose 2% was effective in reducing leg ulcers, increasing tissue granulation area and lowering treatment costs.
Keywords: Nursing; leg ulcer; health care costs; carboxymethylcellulose.
INTRODUCTION
The development of new technologies has provided increased product offering in the market. In the dermatology field it has been found even more products for the treatment of wounds. The emergence of more specific dressings aims to enhance the healing process of the lesions and provide the patient with better conditions of treatment and recovery. However, whereas the wide variety of products enables a better adequacy and handling of many types of wounds it also requires specialized knowledge in the field1,2.
In health care, new procedures and new treatment techniques are incorporated by many professionals often at an accelerated rate and even before sufficient evidence to support its safety and efficacy. In addition, these technologies are not substitutive, but cumulative3, which increase the material resources for patient care, but also significantly increase the cost of treatments.
Concern for the proper management of costs in health care, due to the disproportion between the demand of hospital and health needs and the availability of those resources, has drawn attention to a recent approach, costs related to health care.
The sharp scientific and technological development since the Second World War has contributed to the economic health complex is constituted as one of the largest development sectors. At the same time, the health of individuals and populations is now considered a right to be preserved, which contributed to the expansion of health systems and the medicalization of society4.
Given the above, this study aimed to evaluate the cost and effectiveness of carboxymethylcellulose (CMC) 2% in the treatment of leg ulcers.
THEORETICAL FRAMEWORK
Leg ulcers are considered a major public health problem worldwide, accounting for considerable economic impact, both in the governmental sphere, due to the high expenditure on treatment, and in the personal sphere, due to the physical and social limitations of the patient.
The presence of injury, poor wound healing, the continuing pain and physical limitations as well as various psychosocial problems, such as isolation, lead the patient to loss of self-esteem and removal from work5-7.
The main causes of chronic leg ulcers are venous diseases; 60 to 80% of leg ulcers have venous component8. Research shows that 20% of all diabetics develop lower limb ulcers at some point in their lives and 25% of all hospitalizations that occur with diabetic patients are due to impairment in the lower limbs9. The classic diabetic foot is caused mainly by distal neuropathy. Clinically, they are ulcers that are located in pressure areas, having a keratosis area as halo10. Its main features are the absence of sensitivity and circular edges of most common locations on the plantar surfaces.
Although there are few epidemiological studies on leg ulcers, it is known that these ulcers are very frequent in medical practice and absorb large amounts of health care resources aimed at their management11. The treatment of leg ulcers is quite costly for healthcare institutions, patients and families since the injury is chronic and recurrent 12. About 30% of healed ulcers return within the first year. And due to the increase in life expectancy of the population, its frequency is increasing because the prevalence increases with age, with occurrence rate of more than 4% in people aged 65 years old or older6,11.
In the topical treatment of these lesions, technological advances in dressing field have been considered, with the supply of products that clearly accelerate the healing of wounds and facilitate greatly the patient's life. However, some factors are important in this regard, such as: the financial resources of the patient and/or the health unit, the need for continued use of the dressing, including home visits, and the evaluation of benefits and costs that should be considered when choosing the appropriate dressing type to the nature, location and size of the wound2.
The carboxymethylcellulose hydrogel is a natural polymer used in treating wounds, classified as primary dressing and of excellence for hydration and maintenance of a moist wound environment. It has the characteristic of absorbing, scaling and debriding necrotic and fibrotic tissue. It is available in various forms, that are based on a variety of different polymers13-15.
METHODOLOGY
This is a prospective study, of therapeutic intervention and uncontrolled clinical trial type on the cost and effectiveness of carboxymethylcellulose (CMC) 2% produced a university pharmacy for the treatment of wounds in patients with leg ulcers. It was approved by the Research Ethics Committee of the Universidade Federal Fluminense with No. 0154.0.258.000-08 and occurred from January to October 2010.
A total of 20 volunteers were enrolled in the study, through random probability sampling, chosen from the patients who were already being attended at the Tissue Repair Clinic of the University Hospital in Niteroi/Rio de Janeiro State. The inclusion criteria for the study were volunteers over 18; recommended to use CMC 2%; absence of infectious process in the lesion; with chronic leg injury in one or both lower limbs; with cognitive conditions to follow the recommended guidelines during the study period. The study showed a loss of 20% of the sample group (four volunteers), for reasons that prevented their stay in the study, namely: due to occurrence of local and systemic infection requiring the change of treatment; due to the patient's request, who reported frequent pain complaints; due to change of mental status; due to health complications that required hospitalization and removal from the study. Thus, 16 volunteers were followed during 90 days for data collection.
The product
Carboxymethylcellulose (CMC) 2% was produced at the University Pharmacy of Pharmacy School, Universidade Federal Fluminense, following the formulation of an amorphous and non-sterile gel. Its composition was: 2% CMC, 0.1% methylparaben, 20% propylene glycol and 77.9% purified water in 100g bottles. The production of a non-sterile gel requires means of quality control and effectiveness of the product periodically, thus the CMC 2% underwent Physical-Chemical Control and Microbiological Control. All tests used for the study produced satisfactory results and there was no impediment to its use in the study volunteers.
Effectiveness evaluation
The effectiveness evaluation of CMC gel 2% was held by instrument with clinical data, the measurements of the wounds made every 15 days, through digital photography and tracing of lesions. Wound tracings were made in acetate sheets, and transferred to graph paper, having as parameters the size reduction of the wound and changes in tissue characteristics in four stages: start of treatment, 30 days, 60 days and 90 days. The presence of epithelialization, granulation, slough and necrosis were evaluated using an ordinal scale validated for the study: 0 = 1, 1-25% = 2, 26-40% = 3, 41-75% = 4 and 75-100 = 5.
Evaluation of costs
Spending with materials used in the healing procedure in the clinic and spending with materials delivered to the patient for the home dressing - dressing kit - were recorded. The perspective chosen for the study was the Unified Health System (SUS), as service buyer organization. Only the direct costs covered by the public system were computed. This includes the procedures covered by SUS procedures reimbursement tables, such as: ComprasNet, Procedures Table Management System, Drugs and Orthotics and Prosthetics and special SUS Materials (SIGTAP) and Ministry of Health Prices Bank. Thus, other costs incurred by SUS, such as those related to long-term treatments, the use of medication, social services, management and public campaigns, were not measured in the analysis period.
Statistical analysis
Descriptive and inferential statistical analyses were used. Descriptive analysis was used in the evolution variables of ulcers after 90 days. For inferential statistical analysis, the statistical tests of Friedman, Mann-Whitney and Kruskal-Wallis were used, with p-value less than 0.05 (ρ <0.05) level of statistical significance, and the Pearson's correlation to compare means in reducing areas and cost of treatment analyzed.
RESULTS AND DISCUSSION
Evolution of leg ulcers
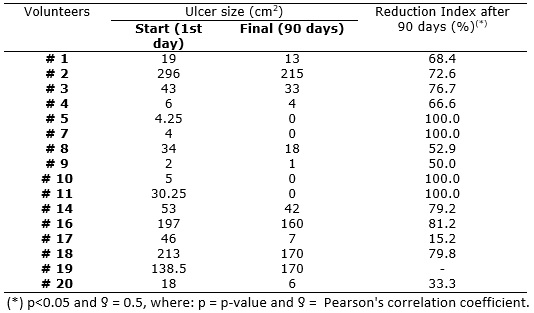
Of the 16 volunteers attended in the Tissue Repair Clinic during the study period, with respect to the evolution of leg ulcers in use of CMC 2%, it was observed that the reduction of injuries was higher in the first weeks of treatment, which indicates good prognosis with the implemented therapy and impact on tissue healing. The area reduction in lesions during each week of follow-up showed strong correlations, since the reductions of leg ulcers had a p-value of 0.0317 and a correlation factor of 0.5 as shown in Table 1. Importantly, of the 16 volunteers studied, 4 (25%) reached the total tissue healing, whereas the other 12 (75%) presented ulcer reduction, but did not reach complete healing of the lesions, remaining with lesional area until the 12th week of treatment.
When comparing the reduction of injuries at the beginning and end of clinical follow-up rate (after 90 days), it was noticed that 14 (93.75%) study volunteers in use of carboxymethylcellulose 2% had their lesion area reduced from 20.19% to 100% of the total area. The mean reduction of all 16 study volunteers was 50.07% ± 37.7, as shown in Table 1. For some scholars16-19, the necessary time for healing a leg ulcer depends on a number of physical factors, including the initial ulcer area, bounded by the edge of the wound, the initial depth of the lesion, the location of the ulcers and the rate of migration of fibroblasts and keratinocytes for the lesional bed.
TABLE 1: Evolution of leg ulcers in volunteers using CMC 2% after 90 days of treatment. Niterói /RJ, 2010.
It found that volunteers that did not have reduction of fibrin, most remained with their lesions open until the 12th week of treatment, which corroborates studies claiming that the identification of fibrin in 50% or more of the wound surface suggests a poor prognosis in wound healing. Patients with unsatisfactory evolution of the wound bed will hardly have their lesions healed, considering that the presence of non-viable tissue, besides favoring infections, does not allow the formation of granulation tissue and proper reepithelization20,21. It is reasonable to assume that a satisfactory evolution observed in the study could be attributed to the CMC 2%, since the gel has the function of reducing fibrin, through autolytic debridement and also promotes epithelization of the wound by maintaining the moist bed wound 5,7,8,22.
Economic evaluation of carboxymethylcellulose 2%
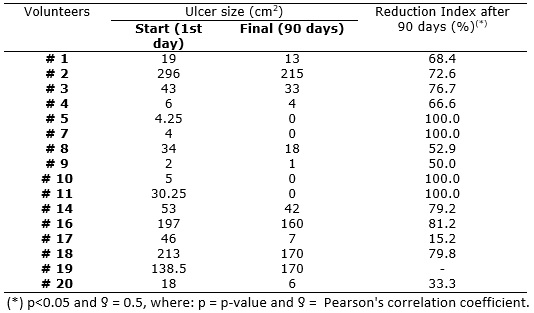
In order to better evaluate the use of CMC 2%, it is introduced the cost reduction relating to the 90 day follow-up of leg ulcers in volunteers according to the size of the area categorized by the study, as follows: area A – larger than 100 cm2 and area B – smaller than 100 cm2. It was noticed that reducing costs was of R$ 14.66 and R$ 43.86 (p <0.0001), respectively. We observed that in group A there was a cost increase in the second month, which correlates with the process of adaptation of the therapeutic product to the patient, as shown in Figure 1.
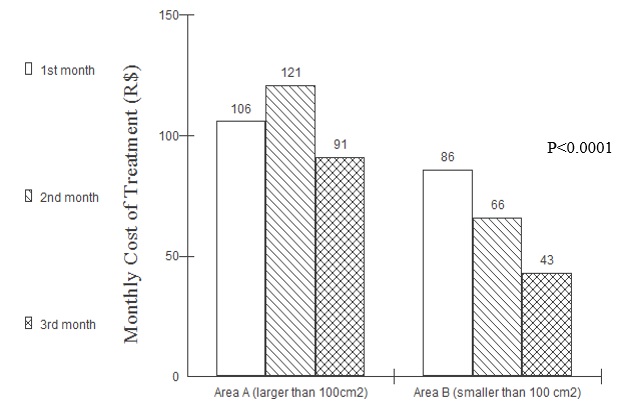
FIGURE1: Comparison of the monthly cost of treatment with CMC 2% according to the size of the lesion area of the volunteers attended during the 90 days of treatment. Niterói/RJ, 2010.
As regards the cost of the treatment with material resources, when analyzing the average price of products used for the treatment of wounds with CMC 2% manipulated in the university pharmacy during one month of treatment, it was reached at an average monthly cost of R$ 70.75 for the group of volunteers from area B and R$ 112.85 for those belonging to area A, as presented in Figure 2. Studies have proven this statement when showed that the total time for healing is one of the factors that most influenced the costs of treatment23.
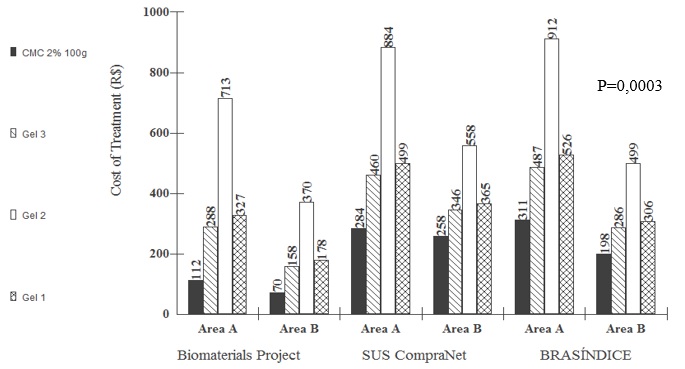
FIGURE2: Comparing the cost of treating leg ulcers with CMC 2% 100g and 100g of proportional gelsin the three levels of the Research Project. Niterói/RJ, 2010.
When the proportional relationship of the quantity of gel of blisters in the samples available on the market, with carboxymethylcellulose 2% of 100 grams, was carried out, it was observed that the values corresponding to the size of the lesion areas varied according to the standard reference of 100 grams of carboxymethylcellulose 2% (p = 0.0003). The results show that even with the proportion of the industrialized gels for the amount of 100 grams, such as carboxymethylcellulose 2%, the values remain above the real value, regardless the size of the affected area, as shown in Figure 2. A study showed that the weekly cost associated with long-term ulcers is more than double the cost related to the treatment of short-term injuries, regardless of the size of the ulcer, which occurred due to the increase of costs with personnel, as a direct result of more frequent and long dressing changes and a long time for healing5,7,24.
CONCLUSION
The study revealed that the treatment of leg ulcers with CMC 2% showed a significant reduction in edema, pain, maceration and also a satisfactory development of the wound bed since it promoted the increase of granulation tissue until its epithelialization.
It was concluded that the use of carboxymethylcellulose 2% gel not only contributed to accelerate the healing process but also to reduce treatment costs when compared with other gels available on the domestic market.
Carboxymethylcellulose 2% masterly manipulated in a university pharmacy represented an alternative for the treatment of leg ulcers in the SUS, since it promoted improvement in healing rates, reduced treatment time and low cost, bringing lower expenses for health services and funding bodies.
The considerable technological growth increases the supply of products for dressing on the market; however, it is important to evaluate the costs and benefits of these products, and particularly the potential for national development as well as providing a systemized care based on the best scientific evidence.
REFERENCES
1.Sevegnani PO, Burim SFF, Filus WA. Custos diretos de curativos em úlcera por pressão: estudo de caso. Bol Enferm. 2007; 1:46-65.
2.Franco D, Gonçalves LF. Feridas cutâneas: a escolha do curativo adequado. Rev Col Bras Cir. 2008; 35:203-6.
3.Ministério da Saúde (Br). Diretrizes metodológicas: estudos de avaliação econômica de tecnologias em saúde. Brasília (DF): Ministério da Saúde; 2009.
4.Ministério da Saúde (Br). Política nacional de gestão de tecnologias em saúde. Brasília (DF): Ministério da Saúde; 2010.
5.Carmo SS, Castro CD, Rios VS, Sarquis MGA. Atualidades na assistência de enfermagem a portadores de úlcera venosa. Rev eletrônica enferm. 2007; 9:506-17.
6.Abbade LPF. Abordagem do paciente portador de úlcera venosa. In: Malagutti W, Kakibara CT. Curativos, estomias e dermatologia: uma abordagem multiprofissional. 2a ed. São Paulo: Martinari; 2011. p.89-100.
7.Barbosa JAG, Campos LMN. Diretrizes para o tratamento da úlcera venosa. Enferm glob. 2010; 20:1-13.
8.Scottish Intercollegiate Guidelines Network (UK). Management of chronic venous leg ulcers. A national clinical guideline [site de internet] 2010. [citado em 28 jun 2013] Disponível em: http://www.sign.ac.uk/pdf/sign120.pdf
9.Borges EL. Feridas – úlceras de dos membros inferiores. Rio de Janeiro: Guanabara Koogan; 2011.
10.Scemons D, Elston D. Nurse to nurse: cuidados com feridas em enfermagem. São Paulo: Mc Graw-Hill; 2011.
11.Silva FAA, Freitas CHA, Jorge MSB, Moreira TMM, Alcântara MCM. Enfermagem em estomaterapia: cuidados clínicos ao portador de úlcera venosa. Rev Bras Enferm. 2009; 62:889-93.
12.Sant'ana SMS, Bachion MM, Santos QR, Nunes CAB, Malaquias SG, Oliveira BGRB. Úlceras venosas: caracterização clínica e tratamento em usuários atendidos em rede ambulatorial. Rev Bras Enf. 2012; 65:637-44.
13.Medeiros WS, Oliveira BGRB, Granjeiro JM. Biomateriais e o corpo. In: Figueiredo NMA, Machado WCA. Corpo e saúde: condutas clínicas do cuidar. Rio de Janeiro: Águia Dourada; 2009. p.89-97.
14.Rodrigues LM, Souza CJ. Assistência de enfermagem em lesões de pele e úlceras por pressão. In: Souza CJ. Manual de rotina em enfermagem intensiva. Rio de Janeiro: Guanabara Koogan; 2010. p.247-302.
15.Iponema E, Costa MM. Úlceras vasculogênicas. In: Silva CRL, Figueiredo NMA, Meireles IB. Feridas: fundamentos e atualizações em enfermagem. São Caetano do Sul: Yendis Editora; 2007. p.381-96.
16.Rabeh SAN, Gonçalves MBB, Caliri MHL, Nogueira PC, Miyazak MY. Construção e validação de um módulo educativo virtual para terapia tópica em feridas crônicas. Rev enferm UERJ. 2012; 20:603-8.
17.Tennvall GR, Hjelmgren J, Oien R. The cost of treating hard-to-heal venous leg ulcers: results from a Swedish survey [site de Internet] 2006. [citado em 28 jun 2015] Disponível em: http://www.worldwidewounds.com/2006/november/Tennvall/Cost-of-treating-hard-to-heal-venous-leg-ulcers.html
18.Abreu AM, Oliveira BGRB, Manarte JJ. Treatment of venous ulcers with an unna boot: a case study. Online Braz J Nurs. 2013; 12(1):198-208.
19.Stephen-Haynes J. Leg ulceration and wound bed preparation: towards a more holistic framework [site de Internet] 2007. [citado em 23 nov 2014] Disponivel em: http://www.worldwidewounds.com/2007/october/Stephenhaynes
20.Dealey C. Cuidando de feridas: um guia para enfermeiras. 3ª ed. São Paulo: Atheneu; 2008.
21.Agency for Healthcare Research and Quality (US). Chronic Venous Ulcers: A Comparative Effectiveness Review of Treatment Modalities [site de Internet] 2012. [citado em 28 jun 2015] Disponível em: http://effectivehealthcare.ahrq.gov/ehc/products/367/995/CVU_AmendedProtocol_20120913.pdf
22.Morley S. Management of chronic venous leg ulcers: a national clinical guideline. Scottish Intercollegiate Guidelines Network [site de Internet] 2010. [citado em 28 jun 2015] Disponível em: http://www.sign.ac.uk/pdf/sign120.pdf
23.Pálsdóttir G. Chronic leg ulcers in Iceland: Prevalence, aetiology and management [site de Internet] 2009. [citado em 28 jun 2015] Disponível em: http://skemman.is/stream/get/1946/2296/7329/1/
24.Australian Wound Management Association Inc (AU). Australian and New Zealand Clinical Practice Guideline for Prevention and Management of Venous Leg Ulcers. New Zealand (Au): Cambridge Publishing; 2011. p.30-61.