ORIGINAL RESEARCH
Interruptions in intensive care nursing shift handovers: patient safety implications
Jéssica Grativol Aguiar Dias de OliveiraI; Luana Ferreira de AlmeidaII; Leni Fagundes de Assis HirabaeIII; Karla Biancha Silva de AndradeIV; Claudia Maria da Silva SáV; Vanessa Galdino de PaulaVI
I
Nurse. Specialist in intensive care. University of Rio de Janeiro State.
Brazil. E-mail:
jessicagrativol@hotmail.com
II
Nurse at the University Hospital Pedro Ernesto. Ph.D. Adjunct Professor,
University of Rio de Janeiro Sate. Brazil. E-mail:
luana.almeida3011@gmail.com
III
Specialist of intensive care. Nurse at the University Hospital Pedro
Ernesto, University of Rio de Janeiro Sate. Brazil. E-mail: leni.assis@hotmail.com
IV
Ph.D. Adjunct Professor, University of Rio de Janeiro Sate. Brazil. E-mail: karla.biancha@gmail.com
V
Master. Nurse at the University Hospital Pedro Ernesto, University of Rio
de Janeiro Sate. Brazil. E-mail: enfclaudiamaria@gmail.com
VI
Master in Nursing. Assistant Professor, University of Rio de Janeiro Sate.
Brazil. E-mail: vangalpa@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.33877
ABSTRACT
Objective: to identify factors intervening during shift handovers in an intensive care unit. Method: this cross-sectional, descriptive, observational, quantitative study of 522 shift handovers among nursing personnel was conducted at an intensive care unit of a university hospital in the municipality of Rio de Janeiro, between February and June 2017. Data were collected by observation and recording by researchers using a checklist for the main factors that may interfere with shift changes, and were analyzed by simple descriptive statistics. The study was approved by the research ethics committee. Results: the factors most observed were: alarms ringing (79.6%), parallel conversations (19.3%), and quiet voice of the professional handing over the shift (11.1%). Conclusion: the intervening factors identified were considered to be factors impairing effective communication between the nursing team and aggravating risks to patient safety.
Descriptors: Communication; nursing; intensive care units; patient safety.
INTRODUCTION
The theme of this study is centered on the goal 2 of the National Patient Safety Program, established by the Ministry of Health in 2014 - to improve communication among health professionals. The World Alliance for Patient Safety defines patient safety as reducing the risk of unnecessary harm associated with health care to the least acceptable level1.
In the intensive care unit (ICU), it is essential that communication be effective and leave no gaps because it is a complex environment with a great flow of health professionals and information2. One of the main tools for communication between the team corresponds to the on-duty shift (DS) since this moment favors the organization of information about patients and the management of care during the workday3. The information among professionals should be relevant in the planning of actions and prevention of adverse events, that is, incidents capable of causing harm to health. These incidents should be minimized to ensure safer assistance4,5.
It is known that there are factors capable of negatively interfering with DS and care transitions, such as professional interruptions, non-use of standardized instruments, ringing of alarms, distractions among professionals, parallel conversations, low tone of voice of the professional performing the passage and even the intercurrences during critical patient care. These factors compromise communication among professionals and may contribute to nursing care and planning failures, representing a fragility in health care planning1.
In this sense, this study aimed to identify intervening factors during DS in an ICU of a university hospital in Rio de Janeiro. In Brazil, there are still few studies that evaluate factors that may interfere with the transfer of care during DS. Identifying and disseminating these results may point to opportunities for improvement in critical patient care and assist in planning interventions focused on patient safety.
LITERATURE REVIEW
In the area of health, ineffective communication is among the root causes of more than 70% of errors in care. Due to problems related to patient safety in 2004, the World Health Organization (WHO) created the Global Patient Safety Alliance. It is observed that the lack of integrated communication processes among professionals is a factor that contributes to failures during care and implies patient safety¹.
In the context of effective communication there are processes called: handoff, which in hospitals are passages or episodes in which a patient and his information are changed from professional to professional to ensure the minimum possible error in the treatment of it; and handover, a process involving the transfer of responsibility, the complexity of the type of information to be transmitted and the characteristics of the professionals 6. When barriers exist that influence the quality of handover, the quality of the services decreases, being more susceptible to the occurrence of errors7.
Patient safety is related to quality of care. Regarding to hospitals, it is important to highlight the importance of promoting a safety culture, which is understood as an individual and organizational behavior that seeks to establish a commitment to promote safe practices, avoiding adverse events and, finally, guaranteeing the quality of services8,9. Thus, patient safety can be defined as the establishment of measures aimed at minimizing the risks associated with care. In this line, the safety culture favors the improvement of safe practices, through improvements in communication, teamwork and knowledge sharing10.
A research of three teaching hospitals in Rio de Janeiro identified an incidence of 7.6% of patients with adverse events, 66.7% of which were preventable. In the last decade, this context has encouraged the promotion of different initiatives to ensure safer health care11.
In the hospital context, the DS is considered a tool of communication and organization of nursing work. It is also added that this procedure promotes the identification of problems and needs for subsequent situational analysis that will allow a reorientation of care2.
In addition to the factors previously mentioned, those capable of interfering with DS are excessive or reduced amount of information, omission or transfer of incorrect data, illegible and incomplete records, interruptions and distractions among team members compromise communication between professionals nursing and may contribute to nursing care failures12.
METHODOLOGY
This is a cross-sectional, descriptive, non-participatory, quantitative approach. The research was performed in a general ICU of a large university hospital in the city of Rio de Janeiro. The unit has capacity for ten beds, admits adult individuals, with clinical and surgical profile for observation and treatment of health.
In this sector, DSs occur from night service to day service beginning at 7:00 AM, and from daytime service to night service at 7:00 PM. The unit has six nursing teams divided into two shifts: daytime and night service. During the study period, there were 14 nurses, one head and one daycare worker, 41 nursing technicians, and 15 nursing residents, 7 of the first year and 8 of the second year.
The DSs are performed with the nursing team gathered at the nursing station, which is located near the entrance and exit door of the unit. For the transmission of information during this time, the unit has its own form, prepared in advance by the nurses in the sector studied. This instrument includes information such as the name of the patient, medical diagnosis, daily multi-professional visits, procedures performed and scheduled, level of consciousness, complications with the patient, medications used, ventilatory parameters, characteristics, and presence or absence of tracheal secretion, presence of intestinal function, diuresis record and skin related aspects.
The DSs performed from the night service to the daytime and vice versa, performed by nurses, technicians and nursing residents of the first and second year were included in this study. Those DSs carried out by professors and nursing students were excluded.
Data were collected from February to June 2017, on randomized and interspersed days. The observations were guided through a form in the check-list model. This was divided into two parts: the first part common to all DSs of the ICU, related to general information such as the number of participants at the time, professional category, date, start and end time of the activity and the second part, with main observed intervening factors, capable of generating interferences.
The data were organized and tabulated with the help of the ExcelR program, analyzed by simple descriptive statistics and demonstrated through tables. In accordance with Resolution Number 466 of 2012, of the National Health Council, which provides for ethical and legal aspects for human being research, the project of this study was submitted to the Research Ethics Committee of the institution and approved under the number of the opinion CAAE 64134016.0.0000.5259.
RESULTS AND DISCUSSION
Sixty observations were made, 40 (80%) of which were carried out in the daytime and all were guided by the form elaborated by the researchers, obtaining information of 522 DSs. The mean duration of the DSs was 21 minutes, with a median of 19. The information was transmitted as follows: 53 (88%) by the on-call nurse, 6 (10%) by the on-call nurse with the residents of the second year, and 1 (2%) by first and second-year residents.
It was verified that in 510 DSs (98%), the standardized instrument was used in the studied ICU. However, in 458 (90%) of them, the form was reported incompletely for the team and underutilized. This may have occurred due to their inadequate filling or due to intervening factors such as conversations, alarms, and interruptions of other professionals, among other reasons³. In fact, the transition from care guided by an instrument improves communication among professionals. Therefore, its use is recommended for patient safety.
The partial description of the facts and situations about critical patients can also be explained by the lack of time in the large workload demanded by the unit studied, in the number of nursing staff and/or the possible non-valuation of the information contained in the current instrument of DS by the professional13. Possibly, nurses and/or residents in this context, faced with so many tasks, prioritized more direct and clinical aspects related to the severity and assistance of patients, such as preparation and administration of medications, care with ventilatory support and feeding by probes, to the detriment of records related to patients, also important in communication between the teams.
Among the factors that interfered with DSs, 416 (80%) of them were the alarms of monitors, infusion pumps and mechanical ventilators, which were not attended in 370 (89%) of the cases. This fact contributed to the presence of noise in the unit and may have accentuated communication failures in the nursing professionals about the information about the patients during DS.
Although the ICU health team cares about patient safety issues, it is perceived that there is still little understanding of the importance of alarm systems, since most of them were neglected during the observations. In this context, an important issue to be discussed relates to the fatigue of alarms, termed as a phenomenon that occurs when a large number of alarms cover the clinically significant ones, allowing alarms of clinical relevance to be disabled, silenced and ignored by the team12.
Alarms are common in critical patient units as there are monitoring systems that allow ongoing monitoring of hospitalized patients and faster identification of possible changes. What may be a risk to the patients is the failure to attend to these sound signals and the inadequate intervention in the identified problem14-18. The observed nursing teams, in general, presented minimal response to the alarms; such behavior can become a serious problem for patient safety5-10.
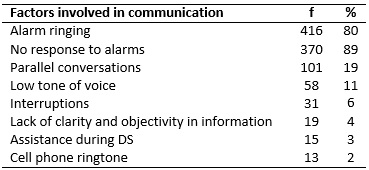
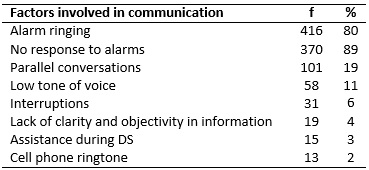
As for the other factors involved in the observed DSs, there were 101 (19%) parallel conversations among the nursing team; in 59 DSs (11%), there was a low tone of voice of the rapporteur who was transmitting the information; in 31 (6%), there were interruptions by other professionals such as physicians, nutritionists and physiotherapists; in 19 (4%), there were lack of clarity and objectivity in the information passed on; in 15 (3%), there was immediate need for nursing care due to intercurrences such as cardiorespiratory arrest, preparation and administration of emergency medications and interventions in situations of hemodynamic instability; and in 13 (2%), the cell phone was ringing, as shown in Table 1.
TABLE 1: Intervening factors in the duty shift. Rio de Janeiro, RJ, Brasil, 2016
In the context investigated, at the time of DS, there is a great flow of professionals from different areas such as doctors, nutritionists, nursing staff, residents and academics, cleaning staff, which can generate dispersion in communication and noises in opening doors.
Studies also point out that insufficient space, which does not adequately support the entire team, absence of professionals, equipment noise, open door and circulation of equipment, patient requests and assistance to them, overcrowding of the unit and performance of procedures, are barriers faced by the nursing team and translate into negative components for DS realization, creating gaps and making communication difficult, and hampering the continuity of care16-18.
CONCLUSION
This study identified several factors that may compromise communication in the nursing professionals, such as - equipment noise, parallel conversations, underutilization of the standardized form, a low tone of voice of the reporter/transmitter, and lack of objectivity in information.
The communication challenges point to the need to reinforce the adequate use of the technology in the unit, stimulate the participation of all the nursing team that transmits and receives information, encourages registration and uses standardized instruments for case shifts, among others. Effective communication among professionals is a topic that is still widely discussed, especially in an environment such as the ICU, which is complex both for the severity of patients and for the use of light and hard technology, aiming at safe and quality care.
The limitations of the study covered the oscillations of DS dynamics in the investigated unit during the period of data collection and the object of study restricted to the nursing team.
REFERENCES
1.Gonçalves MI, Rocha PK, Anders JC, Kusahara DM, Tomazoni A. Patient communication and safety at the admission from neonatal intensive care units. Texto & contexto enferm. (Online). 2016; 25(1): e2310014.
2.Rodriguez L, Oliveira EO, França CS, Andrade TRS, Pontes JS, Aguiar MC, et al. Mapping of the shift from the perspective of the nursing professionals. Enferm. glob. 2013; 31(2): 239-31.
3.Empaire PP, Amara ACKB. What every intensivist should know about the admission in intensive care unit. Rev. Bras. Ter. Intensiva. 2017; 29(2): 121-3.
4. Ministry of Health (Br). National Health Surveillance Agency. Resolution – RDC n° 36 of July 25, 2013. Institutions for patient safety in health services and other measures. Brasilia (DF): ANVISA; 2013.
5.Silva LD. Patient safety in the hospital context. Rev. enferm. UERJ. 2012; 20(3): 291-2.
6.Cohen M, Hilligoss B. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual. Saf. Health Care, Ann Arbor. 2010; 1(1): 109-13.
7.Santos MCD, Andrade AG, Guimarães G, Gomes A. Communication in health and patient safety: problems and challenges. Rev. Port. Saúde Pública. 2010; 10 (1): 47-57.
8.Duarte, SCM, Stipp MAC, Silva MM, Oliveira FT. Adverse events and safety in nursing care. Rev. bras. enferm. (Online). 2015; 68(1): 144-54.
9.Souza RFF, Silva LD. Exploratory study of patient safety initiatives in hospitals in Rio de Janeiro. Rev. enferm. UERJ. 2014; 22(1):22-8.
10.Teodoro WR, Aquino LAM. Analysis of the process of shift in a pediatric inpatient unit. REME rev. min. enferm. 2010; 14(3): 316-26.
11.Gouvêa CSD, Tavassos C. Patient safety indicators for acute care hospitals: systematic review. Cad. Saúde Pública (Online). 2010; 26(6): 1061-78.
12.Broca PV, Ferreira MA. Nursing and communication team: contributions to nursing care. Rev. bras. enferm. (Online). 2012; 65(1): 97-103.
13.Oliveira RM, Leitão MTA, Silva LMS, Figueiredo SF, Sampaio RL, Gondim MM. Strategies to promote patient safety: from identifying risks to evidence-based practices. Esc. Anna Nery Rev. Enferm. 2014; 18(1): 122-9.
14.Franco AS, Bridi AC, Karam MA, Moreira APA, Andrade KBS, Silba RCL. Stimulus-response time to intra-aortic balloon alarms: practices for safe care. Rev. bras. enferm. (Online). 2017; 70(6): 1273- 9.
15.Wong A, Malvestiti AA, Hafner MGS. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review. AMB rev. Assoc. Med. Bras. 2016;62(5): 468-73
16.Pedreirinho A, Godinho H, Pinto M, Correia P, Mendes F, Marques MC. Fatigue alarm in patient safety: systematic review. RIASE revista ibero-americana de salud y envejecimiento. 2016; 2(2):544-62.
17.Albuquerque AM, Barrionuevo EA. On-call shift: optimizing team performance. In: Viana RAPP, Torre M. Intensive care nursing: integrative practices. São Paulo: Manole; 2017; 185-94.
18.Oliveira MC, Rocha RGM. Reflection about shift: implications for continuity of nursing care. Enfermagem Revista (Online). 2016; 19(2): 191-8.