ORIGINAL RESEARCH
Nurses' knowledge of the peripherally inserted central catheter: local realities and global challenges
José Antônio de Sá NetoI; Aline Cerqueira Santos Santana da SilvaII; Amanda Ribeiro VidalIII; Virginia Maria de Azevedo Oliveira KnuppIV; Leila Leontina do Couto BarciaV; Ana Claudia Mateus BarretoVI
I
Nurse. MS. Assistant Professor. College of Nursing, Universidade do Estado
do Rio de Janeiro. Brazil. E-mail: jas.neto2009@gmail.com
II
Nurse Doctor. Adjunct Professor. Universidade Federal Fluminense at Rio das
Ostras University Campus. Brazil. E-mail: alinecer2014@gmail.com
III
Nurse, graduated in Nursing at Universidade Federal Fluminense at Rio das
Ostras University Campus. Brazil. E-mail: amandarvidal@yahoo.com.br
IV
Nurse. PhD. Adjunct Professor. Universidade Federal Fluminense at Rio das Ostras University Campus, RJ.
Brazil. E-mail: virgulaknupp@yahoo.com.br
V
Nurse. PhD. Adjunct Professor. Universidade Federal Fluminense at Rio das
Ostras University Campus, RJ. Brazil. E-mail: leila_leontina@hotmail.com
VI
Nurse. PhD. Adjunct Professor. Universidade Federal Fluminense at Rio das
Ostras University Campus, RJ. Brazil. E-mail: amateusbarreto@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.33181
ABSTRACT
Objective: to examine nurses' knowledge of use of the peripherally inserted central catheter (PICC), as an intravenous device in practical care, at three public hospitals in Rio de Janeiro State. Method: this descriptive, cross-sectional study used univariate and bivariate analysis and calculated central tendency measures. Results: although 38 (92.7%) of the nurses reported knowing about the PICC, 29 (70.8%) had no qualification in inserting the catheter; 23 (56.1%) were unaware of the advantages of the device; and 26 (63.4%) stated that the catheter was not indicated at the institutions studied, but that deep puncture predominated. Conclusion: most of the nurses surveyed lacked the title or qualification enabling them to indicate and insert the PICC. Likewise, the institutions surveyed did not indicate the catheter as an intravenous device, despite its undeniable advantages, such as quality and safety in clinical practice.
Descriptors: Peripheral venous catheterization; training; nursing; intensive therapy.
INTRODUCTION
The increasing complexity imposed by the processes of production of nursing care requires the restructuring of the management model applied in the care units to patients with medium and high complexity, aiming to meet with safety and quality the actual needs presented.1
In this aspect, the admission of the patient to the intensive care unit (ICU) poses a great challenge for the health team, who perform an integrated assistance to the patient in this context by considering from the catabolic state of the disease, hemodynamic changes to the clinical, physical and psychic recovery making it imperative to provide a damage-free assistance.2
ICU-referenced clients are in an unstable clinical state, requiring immediate and prolonged interventions, including the need for durable and safe venous access, allowing the infusion of large and constant flows of liquids, such as total parenteral nutrition (TPN), infusion of vasoactive drugs, venous hydration with high glucose infusion rate (GIR), and varied drugs.3,4
With the technological and therapeutic improvement, the use of the peripherally inserted central catheter (PICC) has become an indispensable resource in the treatment of acute and chronic diseases, being a central device of first choice, used for various purposes and varied situations.5,6
It is a safe intravenous device inserted into peripherally arranged vessels with a central location, and its tip should be in large caliber veins, such as the superior and inferior vena cava, allowing the infusion of various drugs, hyperosmolar, vesicant/irritants and long-term therapies. 7, 8
To be successful in clinical practice with PICC, some factors should be considered, such as the skill and technical qualification of the nursing professional, knowledge about the catheter, indication, contraindication, choice of vessel to be punctured, insertion technique, complications, specific care for insertion, maintenance and removal at the end of the therapeutic indication.3
Considering the nurse as the professional mainly responsible for the indication, insertion, maintenance and withdrawal of the PICC, the following question should be highlighted: what knowledge does the nurse have about this intravenous device?
This study aims to analyze the knowledge of nurses about the use of PICC in the practice of care, in three public hospitals in the coastal region of the State of Rio de Janeiro.
LITERATURE REVIEW
At present, 90% of hospitalized patients are treated with intravenous therapy, making it one of the most invasive procedures performed in the hospital setting and a practice mostly developed by the nurse.9
Studies have demonstrated many benefits through clinical practice with the use of the PICC (Peripherally Inserted Central Catheter). Among the main benefits are: reduced risk of infection, preservation of the venous network, less traumatic insertion, longer stay, reduction of costs, reduced risk of complications, administration of vesicant/irritant solutions, such as antimicrobials and vasoactive drugs , in addition to the safe insertion at the bedside by nurses.4,10 Drugs, when administered through this device, dissolve more rapidly, reducing possible adverse events, together with a lower cost and a lower infection rate when compared to the tunneled or surgically inserted Central Venous Catheter (CVC).10,11,12
To obtain better results, in addition to the technical-scientific knowledge, technical ability and qualification for the insertion of the catheter, the nurse must recognize the potential risks and complications of the use of the device, promoting a qualified and safe care to the patient. 13,14
Under this perspective, good health practices, through nursing care, are presented as a key point not only for transformation, but also for scientific evolution. Intravenous therapy is one of the procedures that demands innovations in clinical practice by the nurse, based on scientific grounds, to obtain better care results and quality indicators.5
METHODOLOGY
This is a sectional descriptive study. The research was conducted in three public hospital units of the coastal region of Rio de Janeiro-RJ, Brazil. The hospital units were firstly listed for offering pediatric, neonatology and adult/elderly care units to patients who were more vulnerable, hemodynamically unstable and, more specifically, susceptible to the constant attempt of venipuncture, which made it possible to investigate knowledge and use of the PICC – intravenous device – by nurses.
In view of the ethical aspects provided for in Resolution 466/2012, the participants were nurses who, through the presentation of the Informed Consent Form (ICF), accepted to participate in the study. The following criteria were adopted as inclusion criteria: nurses, pediatric units, neonatal units, adult/elderly care units, generally belonging to the intensive care unit and/or medical clinic,for at least 3 months, regardless of the nursing training time. Other health professionals who were not nurses, with a practice of less than 3 months and who did not work in the sectors, were excluded from the study.
For convenience, the sample was defined considering all professionals by sector, the application of inclusion and exclusion criteria, and the availability of professionals. Forty-one nurses participated in the study.
The research project was submitted to the Research Ethics Committee (REC) of Universidade Federal Fluminense (UFF) and obtained approval under opinion number 1.220.205.
The data collection took place between November 2015 to March 2016. The data collection tool was a structured questionnaire consisting of two parts; the first part of which is devoted to the characterization data of the participants, related to age, gender, length of training, time in which they work in the institution, professional training such as, postgraduate course lato and/or stricto sensu. The second part was related to aspects directly involved with the knowledge and clinical practice of the PICC; among them: qualification or skills; where the course was carried out, indications of the device, advantages, professionals authorized to implant, existence of norms, routines, Standard Operating Procedure (SOP), use of protocol for insertion, maintenance and withdrawal of PICC, among others.
The data collected were submitted to univariate and bivariate analysis, with the calculation of central tendency measures. The data were tabulated in the statistical program R (https:www.r-project.org), which is in the public domain. The results are presented in tables.
RESULTS AND DISCUSSION
Forty-one nurses who worked in the three units in different shifts participated in the study. Thirty-two of them (78%) were predominantly female. The average age was 35 years. Among the participants surveyed, 35 (85.4%) had a Latu Sensu postgraduate degree and 3 (7.3%) had a master's degree. Sixteen of them (39%) have specialization in the area of adult intensive care, followed by specialization in neonatal and pediatric intensive care with 10 (24.4%) and nursing with 7 (17.1%). It was evidenced a profile of nurses with average time of profession between 5 and 10 years. Regarding the working sector, 11 (26.8%) professionals work in the ICU, 11 (26.8%) in the pediatric ward and 6 (14.6%) in the medical clinic.
When questioned if they knew this kind of device, 38 (92.7%) answered yes, and when questioned where they have got the knowledge, 18 (43.9%) answered that it was in universities, followed by 9 (21.9 %) during courses, 7 (17.1%) in lectures and 4 (9.7%) in service.
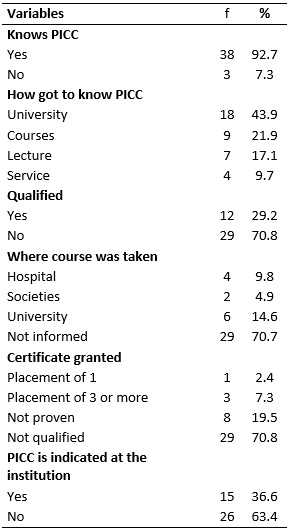
Although a large percentage of the respondents had a specialization degree, out of the 41 professionals, 29 (70.8%) of them had no qualification for insertion of the PICC. With regards to the qualified professionals, when questioned where the qualification course with PICC was held, 4 (9.8%) reported having performed it in hospitals, 6 (14.6%) in universities and 2 (4.9%) in specialized societies. Regarding the certification, 1 (2.4%) participant reported having obtained the certificate according to the requirement of the course to prove the insertion of a catheter, 3 (7.3%) through the insertion of three or more catheters and 8 (19, 5%) had no proof of insertion. It was also observed that 26 (63.4%) nurses of the hospital units surveyed did not indicate the catheter as an intravenous device for the recovery of patients, as shown in Table 1.
Table 1:
Knowledge of nurses about the PICC and qualification for its insertion.
Three units researched, Coastal Region - RJ, 2016
Regarding the knowledge about the catheter, it was possible to observe that most of the participants claimed to know the catheter. However, among them the largest share, despite having a latu sensu postgraduate degree and working in the ICU, is enabled to work with PICC.
It is noted that most nurses were not qualified by specialist societies and that they also obtained the qualification certificate without the practical proof of insertion of catheters. In this sense, it is noticed that there is no legal determination on the requirement of insertion of catheters by the competent bodies and regulators of the profession. Thus, the entities that offer the course themselves have to determine the requirement of implantation of two or more catheters, so the nurses may get a certification.
Despite its benefits, clinical practice with PICC involves a range of factors, which require specific technical-scientific knowledge, and therefore, training and habilitation, with priority for the prevention and early detection of complications related to the use of the device, aiming at the safety and well-being of the patient.12
Among the factors involved in this aspect, it should be noted that the professional, in order to deepen his/her theoretical and practical knowledge, must undergo a training and habilitation course, offered by Sociedade Brasileira de Especialistas em Pediatria (SOBEP) [Brazilian Society of Pediatric Specialists] and by Sociedade Brasileira de Enfermeiros em Terapia Intensiva (SOBETI) [Brazilian Society of Intensive Care Nurses], following the guidelines determined by theInfusion Nurses Society (INS) and by the Center For Diseases Control and Prevention (CDC), headquartered in the United States of America.15,16
In this directive, it is also emphasized the need to include this content in the postgraduate course, assuming a more practical character in the academic training, in order to train new nurses for the insertion of the PICC. Thus, the qualification offered by duly legalized companies or courses point to a safer and less risky practice.17
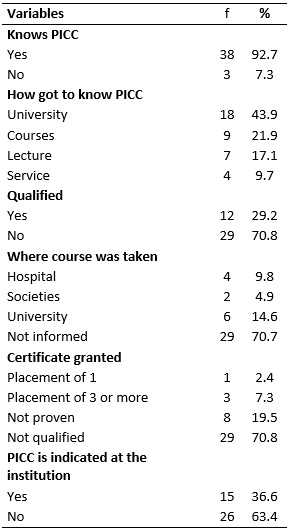
Concerning the knowledge about the PICC indication in the institutions studied, 8 (19.5%) nurses obtained a level of accuracy related to the infusion of vesicant/irritant solutions, such as vasoactive drugs, venous hydration (VH), antibiotic therapy (ATB) and total parenteral nutrition (TPN); other 1 (2.4%) highlighted that the antibiotic scheme requires longer periods, generally longer than 7 days, with a majority of 32 (78.1%) not indicating the device in the Adult ICU, according to the results of Table 2.
TABLE 2:
Nurses' general knowledge about clinical practice with PICC in the three
units surveyed. Coastal Region - RJ, 2016
Regarding the indication of the device, in conducting the care provided, it was possible to observe that most professionals do not indicate the catheter as a choice. This fact is directly related to the lack of training of the nurses, and, therefore, the lack of knowledge about the use of this device in high complexity patients.
Concerning the advantages, it was found that 23 (56.1%) interviewed nurses do not know the advantages that the intravenous device offers, 8 (19.5%) pointed the reduction of venous punctures as a main advantage and 6 (14.6%,) indicated the use of the device for prolonged infusion. When questioned about the average number of catheters per month in the respective institutions, 20 (48.8%) participants reported it as above 10 catheters, 12 (29.3%) reported a maximum of 5 catheters and 9 (21.9%) reported from 5 to 10 catheters.
Regarding the average number of catheters that are indicated per month in the institutions surveyed, the majority claimed an average above 10 catheters per month, however it was possible to observe that in almost all the institutions studied the catheter is not inserted.
In this sense, it is essential to encourage the use of the catheter in the hospital units, knowing that the non-visibility of the catheter is a worrying situation, and it was observed that this is due both to the cost and the training of professionals for the handling of this device, although its benefits are incontestable.17,18
Confirming the fact that the vast majority of the participants were not able to practice with the PICC and did not indicate the device, the majority – 23 (56.1%) – did not know the advantages of using this resource. See Table 2.
Regarding the practitioner who implanted the catheter, 32 (78.1%) of the respondents reported not implanting it, and 8 (19.5%) mentioned it was implanted by nurses and 1 (2.4%) by doctors. Among the interviewees, 32 (78.1%) answered that there were no protocols, norms, routines and/or SOPs as an administrative tool in conducting clinical practice with the catheter, while 9 (21.9%) reported their existence in the institution where they work.
In Brazil, the accomplishment of this procedure is legally supported in Resolution 258/2001 of the Conselho Federal de Enfermagem (COFEN) [Federal Nursing Council], in its article 1, which considers that it is lawful for the nurse to insert the catheter provided that, as described in article 2, the professional is duly qualified through a regulated course.19
Regarding the observation of norms, protocols and guidelines, as an administrative tool in conducting the practice with PICC, the great majority of the participants stated that they did not use them. And among the limits and possibilities for using the catheter, the majority – 31 (75.6%) – pointed to the cost, lack of knowledge and lack of qualified professionals, while the minority 10 (24.4%) – pointed out only the cost as a limiting factor for its application. See Table 2.
The nurse is the protagonist in many actions in his/her daily life. In the case of practice with the PICC, the nurse is responsible from its insertion and maintenance to its withdrawal. However, this concept must extrapolate the valorization of procedures only as a technique and cover the various technical and scientific knowledge that support this practice. As is the case of the existence and use of protocols, norms, routines, SOPs, as well as the Informed Consent Term (ICT) that directs nursing practice in the use of this catheter, aiming to standardize a prescribed procedure, which makes it fundamental to its success.4,7
Regarding the limits and possibilities of use of the PICC, a survey carried out in the city of São Paulo showed that there is a statistically significant difference in the predominance of the use of PICC by private institutions, possibly indicating that the economic factor makes it difficult to incorporate it into the practice of care.18
A study on this topic compared the cost of the catheter, where a peripheral venipuncture costs US$ 32.00 and insertion of the PICC costs around US$ 200.00, which appears to be more expensive, but, when considering the time ICU clients require intravenous therapy, generally superior for seven days, the final cost of the PICC is equal to that of a peripheral puncture. 20
Still, a child with difficult venous access can undergo, on average, 12 to 20 puncture attempts within a four-week period of hospitalization, showing that, from a financial point of view, the use of the catheter may be a more than viable alternative.18
Regarding the most used device in severe patients, the majority of professionals reported that deep puncture is their device of choice, followed by jelco used in the therapeutic conduction of the patient. This demonstrates total ignorance about the advantages and safety provided by the PICC.
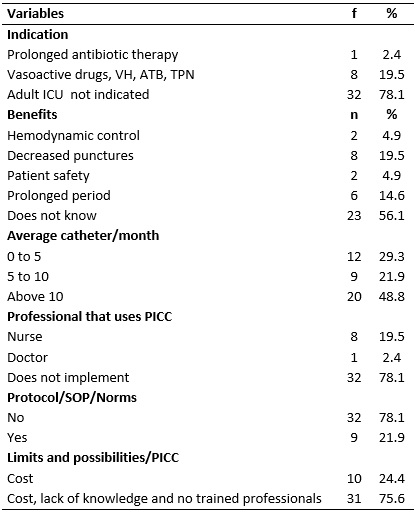
When questioned about which device is implanted in place of the PICC, 20 (48.8%) nurses mentioned jelco in greater proportion, followed by deep venous puncture with 18 (43.9%); thus, the management of the severe patient, in relation to the intravenous therapy, occurs mainly through jelco and deep puncture. See Table 3.
Table 3:
Knowledge about intravenous device most used in severe patient and
implanted device in place of PICC.Three units surveyed, Coastal Region -
RJ, 2016

A study carried out at Instituto Fernandes Figueira showed that the number of catheters inserted in the study period and the number of adverse effects of infectious cause were related to a higher infection rate in the deep venous catheters (34.2%), followed by venous dissection (26.3%), compared with the PICC, which presented a rate of 18.6%.19
Studies have shown that deep puncture should not be the first choice of venous access in treating patients at the limit of their clinical and physical capacity. Regarding the use of jelco in vulnerable patients, some risks become imminent, and may lead to the momentary interruption of the therapy implemented and to the development of iatrogenies, such as phlebitis, vasospasm, pain and infection, as well as an increase in the patient's stay in the hospital unit.21
CONCLUSION
Considering the experiences of nurses with the PICC and the undeniable advantages offered by the device, especially in the management of the severe patient, an incipient and not very expressive practice with the catheter was noted among the units surveyed.
It is concluded that the majority of the interviewed nurses do not have the qualification certificate and/or qualification for the indication and insertion of the PICC and does not indicate the catheter as an intravenous device of choice.
The results point out the need for catheter visibility on the part of professionals, who are mostly unaware of the importance and advantages offered by this device in the patient's recovery. They also show lack of investment from maintaining agencies of the hospital units of the region, interfering in the process of care, in the clinical recovery of the patient's quality of life.
Despite achieving its objective, this study has limitations regarding the performance in only three public hospital units, with a reduced sample, which prevents the generalization of the findings.
This research has as potentiality the portrait done on clinical practice with catheters in these public units. However, it indicates the need for new national studies in nursing in order to elucidate the questions and controversies regarding the clinical practice with the PICC.
REFERENCES:
1.Klock P, Erdmann AL. Caring for newborns in a NICU: dealing with the fragility of living/ surviving in the light of complexity. Rev Esc Enferm USP. 2012; 46(1):45-51.
2.Melão MRC, Marcatto M. Humanização no cuidado neonatal: a concepção da equipe de enfermagem. Rev. pesqui. cuid. fundam. (Online). 2014;6(4):1409-18.
3.Oliveira CR, Neve ET, Rodrigues EC, Zamberlan KC, Silveira A. Cateter central de inserção periférica em pediatria e neonatologia: possibilidades de sistematização em hospital universitário. Esc. Anna Nery Rev. Enferm. 2014; 18(3):379-85.
4.Reis AT, Santos SB, Barreto JM, Gomes GRS. O uso do cateter epicutâneo na clientela neonatal de um hospital público estadual: estudo retrospectivo. Rev. enferm. UERJ. 2011; 19(4):592-7.
5.Avelar AFM, Peterline MAS, Pedreira MLG. Assertividade e tempo de permanência de cateteres intravenoso periféricos com inserção guiada por ultrassonografia em crianças e adolescentes. Rev. Esc. Enferm. USP. 2013; 47(3):539-46.
6.Jacinto AKL, Avelar AFM, Wilson AMMM, Pedreira MLG. Flebite associada a cateteres intravenosos periféricos em crianças: estudo de fatores predisponentes. Esc. Anna Nery Rev. Enferm. 2014; 18(2):220-6.
7.Moura PF, Contim D, Amaral JB. Cateter central de inserção periférica: revisão bibliométrica. Rev. enferm. atenção saúde. 2013; 2(1):106-15.
8.Costa LC, Paes GO. Applicability of nursing diagnosis as grants for indication of Central Catheter of Peripheral Insertion. Esc. Anna Nery Rev. Enferm. 2012; 16(4):649-56.
9.Rangel RJM, Castro DS, Primo CC, Zandonade E, Christoffel MM, Amorim MHC. Cateter central de inserção periférica em neonato: revisão integrativa da literatura. Rev. pesqui. cuid. fundam. (Online). 2016; 8(4):5193-202.
10.Costa P, Kimura AF, Vizzotto MPS, Castro TE, West A, Dorea E. Prevalência e motivos de remoção não eletiva do cateter central de inserção periférica em neonatos. Rev. gaucha enferm. 2012; 33(3):126-33.
11.Reynolds GE, Tierney SB, Klein JM. Antibiotics before removal of percutaneously inserted central venous catheters reduces clinical sepsis in premature infants. J. Pediatr. Pharmacol. Ther. 2015; 20(3):203-9.
12.Oliveira DFL, Azevedo RCS, Gaiva MAM. Diretrizes para terapia intravenosa no idoso: pesquisa bibliográfica. Rev. pesqui. cuid. fundam. (Online). 2014; 6(1):86-100.
13.Oliveira FT,Machado KMF,Santos LPR, Queiroz NR,Silva J,Paes G. A práxis de acadêmicos de enfermagem aplicada à terapia intravenosa: um estudo antes e depois. Rev. enferm. UERJ. 2014; 22(2):219-25.
14.Baggio MA, Bazzi FCS, Bilibio CAC. Cateter central de inserção periférica: descrição da utilização em UTI neonatal e pediátrica. Rev. gaucha enferm. 2010; 31(1):70-6.
15.Silva ACSS, Santos EI, Queiroz PT, Góes FGB. O papel do enfermeiro com o cateter central de inserção periférica: revisão integrativa. Enferm. Atual. 2017;82(4):71-8.
16.Lourenço AS, Ohara, CVS. Conhecimento dos enfermeiros sobre a técnica de
inserção do cateter central de inserção periférica em recém-nascidos. Rev.
lat. am. enferm. 2010; 18(2):189-95.
17.Camargo PP, Kimura AF, Toma E, Tsunechiro MA. Initial placement of the
peripherally insert central catheter`s tip in neonates. Rev. Esc. Enferm.
USP. 2008;42(4):723-8.
18.Gomes AVO, Nascimento MAL, Silva LR, Santana KCL. Efeitos adversos relacionados ao processo do cateterismo venoso central em unidade intensiva neonatal e pediátrica. Rev. eletrônica enferm. 2012; 14(4):883-92.
19.Vendramim P, Pedreira MLG, Peterlini MAS. Cateteres centrais de inserção periférica em crianças de hospitais do município de São Paulo. Rev. Gaucha enferm. 2007;28(3):331-9.
20.Conselho Federalde Enfermagem. Resolução n° 258, 12 de julho de 2001: Dispõe sobre a inserção do cateter periférico central por enfermeiros. 2001 [cited 2017 May 20]. Available from: http://www.cofen.gov.br/resoluo-cofen-2582001_4296.html .
21.Petry L, Rocha KT, Madalosso ARM, Carvalho RMA, Scariot M. Peripherally inserted central venous catheters: limits and possibilities.Rev. eletrônica enferm.2012;14(4):937-43.