ORIGINAL RESEARCH
Monitoring hand hygiene adherence in an intensive care unit
Bruna Rocha da SilvaI; Monica de Almeida CarreiroII; Bruno Francisco Teixeira SimõesIII; Danielle Galdino de PaulaIV
I
Nurse. Specialist. Student of the Professional Master's Degree Course,
Federal University of the State of Rio de Janeiro. Brazil. E-mail: bru-rocha@hotmail.com
II
Nurse. PhD in Nursing. Professor, Federal University of the State of Rio de
Janeiro. Brazil. E-mail: carreiroma59@gmail.com
III
Statistician. PhD in Engineering. Professor, Federal University of the
State of Rio de Janeiro. Brazil. E-mail: bruno.simoes@uniriotec.br
IV
Nurse. PhD in Nursing. Professor, Federal University of the State of Rio de
Janeiro. Brazil. E-mail: danigalpa@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.33087
ABSTRACT
Objective: to characterize health professionals' adherence to hand hygiene procedure. Method: this cross-sectional study with the multidisciplinary team of an intensive care unit at a hospital in Rio de Janeiro was conducted between January and February 2017. Data were collected in 165 direct observations using an adapted form, and analyzed by R software. The project was approved by the research ethics committee. Results: the gold standard (hand hygiene before and after contact with the patient using the correct technique) was achieved in 13% of the observations. All categories of health personnel performed hand hygiene more after contact with the patient. Conclusion: the rate of adherence to hand hygiene by health professionals was low. However, the category that most hygienized hands before and after contact with patients, using the correct technique, was nurses.
Descriptors: Hand hygiene; monitoring; cross infection; nursing.
INTRODUCTION
Health care-related infections (HCRI) are those acquired by the patient during care received at health facilities, and it is a common cause of increased morbidity and mortality worldwide.1
The magnitude of this problem is demonstrated by the epidemiological relevance of HCRI. Results of studies released by the World Health Organization (WHO), based on reports performed by the Institute of Medicine of the United States, show that 1.4 million people acquire infections annually. In Europe, approximately 6.8% of the hospitalized patients acquire at least one HCRI, and this number becomes even more problematic in developing countries, where the risk of contracting infections is four times higher.2,3
It is also emphasized that the intensive care unit (ICU) is considered the epicenter of the HCRI and the influencing link in the epidemiological chain of transmission. This fact is due to the peculiarity of the patients hospitalized in this unit, as they use invasive devices such as: central venous catheter, bladder delay catheter and mechanical ventilation; in addition, the use of immunosuppressants, prolonged hospitalization, colonization by resistant microorganisms, prescription of antimicrobials and the characteristic of the ICU environment that favors the natural selection of microorganisms.4
Having this in view, several initiatives have been developed by international and national agencies, societies and associations of infection control professionals, with the aim of increasing the adherence to hand hygiene (HH) among health professionals, as WHO's First Global Patient Safety Challenge, the "Clean Care is Safer Care", which aims to reduce the occurrence of HCRI through actions related to the improvement of HH.5,6
However, for prevention to take place it is essential to know the ways that infections are usually triggered. One of the most common is the transmission of microorganisms that occurs mainly through the contact of the professionals' hands with the patients, and/or the contact of the patient with contaminated material or environment. Microorganisms can adhere and colonize any biomaterial surface, putting the patient at risk. 7
Therefore, the HH is considered the measure of greater impact and proven effectiveness in the prevention of infections. Although the action is simple, the compliance with this practice by health professionals is still considered a challenge in the control of HCRI, and it should be stimulated among professionals.8
In view of the above, the present study aimed at characterizing the adherence of the HH practice by health professionals in an adult ICU, before and after contact with the patient.
LITERATURE REVIEW
The hand hygiene is recognized worldwide as a primary measure, but a very important one in the control of HCRI. For this reason, it has been considered as one of the pillars for the prevention and control of infections within the health services, including those resulting from the cross-transmission of multi-resistant microorganisms.9
From this perspective, the hands should be sanitized at essential and necessary moments, according to the care flow. The five moments for HH are: before contact with the patient, before the aseptic procedure, after risk of exposure to body fluids, after contact with the patient, and after contact with areas close to the patient.5
Although there is much evidence that the correct HH is an important measure, adherence to this practice remains low, with rates varying from 5% to 81%, with an average of 40%.10
From the reports of transmission of microorganisms by the hands of professionals and the low rates of adherence to HH, there is a need to monitor these practices and evaluate the quality of the procedures.
In view of the above, the adherence to the recommendations or protocols involves changes in the behavior of professionals who provide care to the patient. The dynamics of behavioral change for the HH compliance is complex and multifaceted, and it is necessary to map unrealized actions in order to focus on the problem. This is a challenge for the government, directors, managers and professionals who work in the Hospital Infection Control Commission (HICC).10
The result can be very useful for the health service, and it can also be used as a HICC tool to set goals within the HCRI Annual Control Program at the institution, as well as to determine its bi-annual application for reassessment and feedback of the process, in addition to develop measures to promote and improve hand hygiene practices as well as the use of new educational strategies.5-8
METHODOLOGY
This is a cross-sectional, observational study performed in the adult ICU, composed of 30 beds, of a public hospital in the State of Rio de Janeiro.
It was used a form with adapted structure, constructed from the hand hygiene observation tool of the handbook for observers: WHO multimodal strategy for the improvement of HM.8
Prior to the final data collection, the form was tested through its application in a similar pilot population, in order to observe the operability and reliability of the instrument. In this stage, 15 health professionals were observed providing direct care to the patients.
The study population was composed of the multidisciplinary team working in the ICU of the institution chosen as the research scenario. The following inclusion criteria were outlined: professionals working in the ICU of this hospital, who actively exercised direct patient care activities during the data collection period, and who agreed to sign the Free and Informed Consent Term (FICT). Those who were on vacation, on a day off or medical leave during the collection period were excluded.
The direct observation for the monitoring of the HH adherence was adopted, being that a total of 165 observations were performed, and the participants were observed at two moments - before and after contact with the patient.
The data collection was carried out during the daytime period, in the moments of greater care activity (from 8 to 10 a.m. for the morning period and from 2 to 4 p.m. for the evening), in the months of January and February of 2017. For this stage, it was used a research assistant previously clarified about the objective of the study and trained by the researcher to complete the form.
It was considered important not to influence the behavior of the participants, however, without hiding the presence of the observers, who maintained a discreet behavior. A distance that allowed the observation without interfering in the dynamics of the unit was kept. In addition, in order to meet the WHO manual, only one health professional was observed at a time.
However, the observed professionals may have suffered the Hawthorne effect, which corresponds to improved performance due to the observation of their actions, which may motivate them to produce better results.
The data from the direct observation were compiled in worksheets and analyzed using the software R.In order to evaluate the data, the multiple correspondence analysis (MCA) was used, because it is a technique of multivariate statistical analysis of data that makes it possible to study the correspondence between several variables.
In the indications referring to HH before and after contact with the patient, positive and negative actions were expressed as a percentage; and in the analyzes, the chi-square test was used to compare the association between the variables, considering the significance level of 5% (p-value≤0.05).
The study complies with the ethical precepts contained in the Resolution No. 466/2012 of the National Health Council, and the project was approved by the Ethics Committee of the Federal University of the State of Rio de Janeiro - UNIRIO with the CAAE number: 60739916.6.0000.528, on December 1, 2016. The participants were guaranteed the secrecy of the information and the necessary clarifications about the study and its objectives through the FICT.
RESULTS AND DISCUSSION
Medical professionals, nurses, nursing technicians and other professionals who were categorized as others (physiotherapist, X-ray technician, speech therapist, occupational therapist and laboratory technician) were observed. This last category was classified in this way due to the characteristics of the work in the adult ICU, which is marked by punctual sessions during the care provision and not by a continuous work like the other professionals of the sample of this study.
There was a total of 165 opportunities for HH, of which 77 (47%) were from nursing technicians, 27 (16%) opportunities from physicians, 23 (14%) from nurses and 38 (23%) opportunities from other health professionals.
Therefore, it is possible to observe that the nursing team totaled 100 (60%) of the observed opportunities, showing that this is the professional category that is most in direct contact with the patients and their environments. This profile corroborates another similar study, which analyzed the adherence through direct observation, in which 75% of the multiprofessional team observed were nursing professionals.11
The COFEN Resolution No. 543/2017, which updates and establishes the parameters for the dimensioning of the nursing professionals staff, shows that each intensive care patient requires an average of 18 hours of nursing every 24 hours.12 When it comes to an adult ICU, it is possible to explain the high number of opportunities observed by the nursing team, since the nature of their work involves the continuous care of the patient.
From the total of 165 observations, in only 22 (13%) the gold standard was reached, which constitutes HH before and after the contact with the patient, using the correct technique. In a similar study carried out in the adult ICU of a teaching hospital in the state of Paraná, the general rate of positive adherence reached 26.5%, data that diverges from the current study.13
In the application of the MCA on the raw data of the data collection phase, it was identified that non-HH is more strongly associated with the medical and nursing technician category before contact with the patient. For the category of other professionals, it is more strongly associated with the non-performance of the HH technique after contact with the patient.
It was also evidenced that the HH actions before and after contact with the patient, in the correct moment and in the correct technique, are more associated with nurses, that is, they are more accomplished by this category, standing out the HH technique after the contact with the patient.
This result is important because studies show that among the health professionals most directly involved in care, nurses have a strategic and reference space in the team, since it is also the job of the nurse to stop the chain transmission of pathogenic microorganisms, reducing the risk of HCRI and improving the quality of care and safety of the patient and the professional.14,15
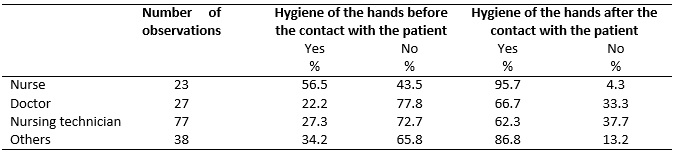
In the characterization of the HH practice observed in the adult ICU, the positive action of HH before contact with the patient was observed in the nurse category in 56.5% of the opportunities, while after contact with the patient, 95.7% of the times.
The medical category performed hand hygiene 22.2% of the times before contact with the patient, and 66.7% of the times after contact with the patient, as shown in Table 1.
TABLE 1:
Percentage of adherence to hand hygiene before and after the contact with
the patient in an adult ICU. Rio de Janeiro, 2017.
This result contrasts a similar study in which physicians obtained the highest rate of adherence to HH.16 However, the author states that the results may differ from other studies that point out the medical team with lower HH adherence rates when compared to other health professionals.17,18
Of the nursing technicians, 27.3% performed HH before the contact with the patient, and 62.3% after the contact with the patient. In a similar study performed in a university public hospital in Belo Horizonte with nursing technicians, the adherence was also higher after the contact with the patient.19 It is important to emphasize the importance of nursing technicians in relation to HH, since they are the professionals who have more direct contact with the patient, during 24 hours.20
When dealing with other categories, it was observed that in 34.2% of the observations the professionals performed the HH before the contact with the patient, and reached 86.8% of adherence to HH after the contact with the patient.
When evaluating HH before and after contact with the patient among the professional categories observed, the chi-square test showed a p-value in HH before the contact with the patient of p=0.03642, and in HH after the contact with the patient p=0.002016. Therefore, for a significance level of 5% (p-value≤0.05), the null hypothesis (Ho) is rejected, that is, there is a significant association between hand hygiene and the professional categories observed in the study.
All the professional categories performed more HH after contact with the patient. The results of the current study corroborate the one performed by the New York-Presbyterian Hospital System in New York, in which the adherence is higher after the performance of care provision. These results also corroborate studies in ICUs that performed the majority of the observations before the indications after contact with the patient. These evidences indicate the professional's concern not to be exposed to the risk of acquiring a disease.15,21
However, in the nurse category, most perform HH before the contact with the patient. They are also the category that more frequently performs HH before and after contact with the patient. See Table 2.
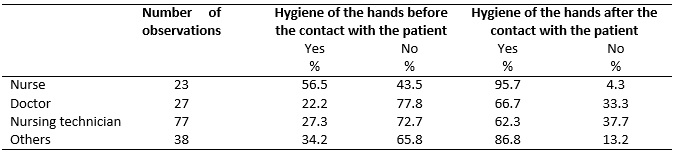
TABLE 2:
Percentage of adherence to the technique of hand hygiene before and after
the contact with the patient in an adult ICU: Rio de Janeiro, 2017.

(*)
Does not attend
According to the observations performed, it is important to mention that of all the observed professionals who sanitized the hands before the contact with the patient, 58% did it correctly; and 57% of those who sanitized their hands after contact with the patient used the recommended technique.
When analyzing the categories individually, nurses are the ones who are most concerned with the correct HH technique before (43.5%) and (56.5%) after contact with the patient. The medical category is the one that least performs HH according to technique after contact with the patient (33.3%). The nursing technicians correctly performed HH in 15.6% of the times before contact with the patient, and 39% of the times after contact with the patient.
The other professional categories performed the correct hand hygiene technique in 13.2% of the times before contact with the patient, and 44.7% after contact. This result differs from that of another study, in which 100% of the other professionals performed HH using the correct technique. 22
It is observed that the procedure of the HH technique becomes inadequate in the daily practice, due to the forgetfulness of some steps (step by step) and there is a concern on the part of health professionals about the quantity and not the quality of this act.5
Thus, the gold standard of HH, that is, at the right moment and with the correct technique, still has low adhesion. In this study, nurses are those who have the highest percentage of adherence. In another study, in a multivariate analysis, the adherence was also higher among nurses when compared to other professional categories.23
On the contrary, in this research, the medical category is the one that least performs HH in the gold standard. A study shows that being a physician is associated with a lower adherence to HH. However, it shows variation of adherence according to the medical specialty, with the overall adherence rate of 57%, ranging from 87% among clinicians to 23% among anesthesiologists.23
Researches show variations among HH-related adherence rates among health professionals, with percentages ranging from 8% to 84.5%.15,24 However, different factors may be related to the low adherence. 25 Among them, these stand out: health services with limited resources, overcrowded, with inadequate or no spatial separation between beds, physical structure, which includes poorly located sinks; the use of gloves; ability, attitudes and motivation; the importance given by the health professional to the risk of not being in compliance with the recommendations for HH, in addition to the training received and the time taken for the procedure.26,27
Authors also point to factors related to the inadequate flow of patient care, due to overcrowding, workload, stress, activities with high risk of cross-transmission of pathogens, lack of knowledge about the HH protocol, lack of a positive example from their superiors, bad habits, forgetfulness, irritation and dryness of the skin caused by the successive use of products.24,28
In view of the above, the low adherence to HH is not directly associated with the theoretical knowledge of such procedure or the situation in which it should be performed, but among other factors, to the incorporation of this knowledge into the daily practice of he professionals.29 Attention should be paid to the fact that the training should be dynamic and aimed mainly at raising the awareness of the professional and not only for the transmission of information, focusing on norms and attitudes, not just on risks.13
It is difficult to change habits, customs, concepts and, mainly, behaviors. However, if there is no awareness work on this simple attitude, nothing will be achieved. For this to occur effectively, the patients, family and/or visitors, training sessions, classes, researches, and a meticulous work with multidisciplinary teams should be prioritized by the HICC, in partnership with professionals from the area.11
CONCLUSION
It was verified in this study that the observed health professionals have a low adherence to the hygiene of the hands at the indicated times and using the correct technique.
It is understood that the nurse is the professional category that most sanitizes the hands before and after having contact with the patient using the correct technique. The categories that least perform the HH are: the medical category, before the contact with the patient and the nursing technician category, after the contact with a patient. Regarding the correct technique of HH, the other professionals category is the one that has less adherence to this practice when sanitizing the hands before the contact with the patient.
There was a greater adherence in the indications that reflect the protection of the professional when compared to those related to the patient's protection; and although there have been variations among the professional categories, it is possible to state that the care in the investigated unit, from the perspective of the low adherence to HH, implies a risk for the safety of the patient.
It was considered as limitations of the study the investigation of other possible factors that are important for the practice of HH, such as the relationship between the number of professionals and the severity of the patients assisted, the materials available, and the professionals' knowledge about the practice studied. Thus, it is understood that these and other gaps can be investigated in the future.
The study offers subsidies that demonstrate the need for continuous training, as well as it helps to unveil ways to change the institutional culture and the behavior of the professional in favor of the adherence to the HH as a routine habit of the team, since it is the simplest and most efficient practice in the control of HCRI.
REFERENCES
1. Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee. Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings, New York (USA): CDC; 2007.
2. Miliani K, Migueres B, Verjat-Trannoy D, Thiolet JM, Vaux S, et al. National point prevalence survey of healthcare-associated infections and antimicrobial use in French home care settings, May to June 2012. Euro Surveill. 2015; 20: 27.
3. Chou DTS, Achan P, Ramachandran M. The World Health Organization '5 moments of hand hygiene': the scientific foundation. J. Bone Jt. Surg. 2.012. 441: 5.
4. Oliveira AC, Kovner CT, Silva RS. Infecção hospitalar em unidade de tratamento intensivo de um hospital universitário brasileiro. Rev. latinoam. enferm. (Online). 2010 [cited in 2017 Dec 151] 18(2):98- 104. Available from: http://www.scielo.br/pdf/rlae/v18n2/pt_14.pdf
5. Ministério da Saúde (Br). Agência Nacional de Vigilância Sanitária. Segurança do paciente e qualidade em serviços de saúde assistência segura: uma reflexão teórica aplicada à prática. Brasília (DF): Ministério da Saúde; 2013.
6. Tartari E, Pires D, Bellissimo-Rodrigues F, De Kraker M, Borzykowski TH, Allegranzi B, et al. The global hand-sanitizing relay: promoting hand hygiene through innovation. J. hosp. infect. [Internet]. 2017 [cited in 2018 Feb 23]. 95(2): 189-93. Available from: http://www.journalofhospitalinfection.com/article/S0195-6701(16)30526-6/fulltext
7. Reisdorfer AS. Infecção em acesso temporário para hemodiálise: estudo em pacientes com insuficiência renal crônica [dissertação de mestrado]. Porto Alegre (RS): Universidade Federal do Rio Grande do Sul; 2011.
8. Organização Mundial da Saúde. Manual para observadores: estratégia multimodal da OMS para a melhoria da higienização das mãos. Brasília (DF): Agência Nacional de Vigilância Sanitária; 2008.
9. Ministério da Saúde (Br). Agência Nacional de Vigilância Sanitária. Segurança do paciente: higienização das mãos. Brasília (DF): Ministério da Saúde; 2010.
10.Ministério da Saúde (Br). Agência Nacional de Vigilância Sanitária. Segurança do Paciente: Relatório sobre Auto avaliação para Higiene das Mãos. Brasília (DF): Ministério da Saúde; 2012.
11.Mota EC, Barbosa DA, Silveira BRM, Rabelo TA. Higienização das mãos: uma avaliação da adesão e da prática dos profissionais de saúde no controle das infecções hospitalares. Rev. Epidemiol. Control. Infec. 2014; 4(1):12-7.
12.Conselho Federal de Enfermagem. Resolução COFEN 543/2017. Atualiza e estabelece parâmetros para o Dimensionamento do Quadro de Profissionais de Enfermagem nos serviços/locais em que são realizadas atividades de enfermagem. Brasília (DF): COFEN; 2017.
13.Bathke J, Cunico PA, Maziero ECS, Cauduro FLF, Sarquis LMM, Cruz EDA. Infraestrutura e adesão à higienização das mãos: desafios à segurança do paciente. Rev. gaúch. enferm. 2013; 34(2):78-85.
14.Backes DS, Backes MS, Sousa FG, Erdmann AL. Papel do enfermeiro no contexto hospitalar. Ciênc. cuid. saúde. 2008; 7(3):319-26.
15.Araujo AP, Nóbrega GB, Santos LFC, Aragão RS, Pontes AAN. Análise da higienização das mãos pelos profissionais de saúde em ambiente hospitalar durante dois meses. Rev. saúde e ciênc. (Online) 2015 [cited in 2017 May 11]. 4(3):44-54. Available from: http://150.165.111.246/revistasaudeeciencia/index.php/RSCUFCG/article
16.Paula AO. Impacto da estratégia multimodal na adesão à higiene de mãos entre a equipe multiprofissional [tese de doutorado]. Belo Horizonte (MG): Universidade Federal de Minas Gerais; 2015.
17.Borges MG, Ribeiro LCM, Figueiredo LFS, Sirico SCA, Souza, MA. Adesão à prática de higienização das mãos por profissionais de saúde de um Hospital Universitário. Rev. eletrônica enferm. 2010; 12(2): 266-71.
18.Nascimento NB, Travassos CMR. O erro médico e a violação às normas e prescrições em saúde: uma discussão teórica na área de segurança do paciente. Physis. 2010; 20: 2.
19.Oliveira AC, Paula AO, Gama CS, Oliveira JR, Rodrigues CD. Adesão à higienização das mãos entre técnicos de enfermagem em um hospital universitário. Rev. enferm. UERJ. 2016; 24(2):e9945.
20.Souza LM, Ramos MF, Becker ESS, Meirelles LCS, Monteiro SAO. Adesão dos profissionais de terapia intensiva aos cinco momentos da higienização das mãos. Rev. gaúch. enferm. [Internet] 2015 [cited in 2017 Dec 11]. 36(4) :21-8. Available from: http://www.seer.ufrgs.br/index.php/RevistaGauchadeEnfermagem/article/view/49090
21.Clock AS, Cohen B, Behta M, Ross B, Larson EL. Contact Precautions for Multidrug-Resistant Organisms (MDROs): Current Recommendations and Actual Practice. Am. J. infect. control. 2010; 38(2): 105–11.
22.Mota EC, Barbosa DA, Silveira BRM, Rabelo TA, Silva NM, Silva PLN et al. Higienização das mãos: uma avaliação da adesão e da prática dos profissionais de saúde no controle das infecções hospitalares. Rev. epidemiol. control. infect. 2014; 4(1):12-17.
23.Pittet D, Simon A, Hugonnet F, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann. intern med. 2009; 141(6): 1-8.
24.Muller MP, Carter E, Siddiqui N, Larson E. Hand hygiene compliance in an Emergency Department: the effect on crowding. Acad. emerg. med. 2015; 22(10): 1218-21.
25.Herrera-Usagre M, Pérez-Pérez P, Vázquez-Vázquez M, Santana-López V. Profesionales de salud ante la mejora de la higiene de las manos: estrategias clásicas versus estrategias avanzadas. Rev. chil. infectol. [Internet]. 2014 [cited in 2018 Jan 21]. 31(5): 534-41. Available from: http://www.scielo.cl/scielo.php?pid=S0716-10182014000500004&script=sci_arttext
26.Salmon S, Pittet D, Saxc H, McLaws ML. The 'My five moments for hand hygiene' concept for the overcrowded setting in resource-limited healthcare systems. J. hosp. infect. 2015; 91(2):95-9.
27.Nair SS, Hanumantappa R, Hiremath SG, Siraj MA, Raghunath P. Knowledge, attitude, and practice of hand hygiene among medical and nursing students at a Tertiary Health Care Centre in Raichur, India. ISRN Prev Med. 2014; 2014:608927.
28.Ezaias GM, Watanabe E, Shimura CMN. Skin tolerance to alcohol-based preparations: basis for improvement of hand hygiene practices. Rev. enferm. UFPE on line. 2016. [cited in 2018 Jan 16]. 34(2): 2923-32. Available from: http://www.revista.ufpe.br/revistaenfermagem/index.php/revista/article/view/9437/pdf_10790
29.Oliveira AC, Cardoso CS, Mascarenhas D. Precauções de contato em unidade de terapia intensiva: fatores facilitadores e dificultadores para adesão dos profissionais. Esc. Enferm. USP. 2010; 44(1):161-5.