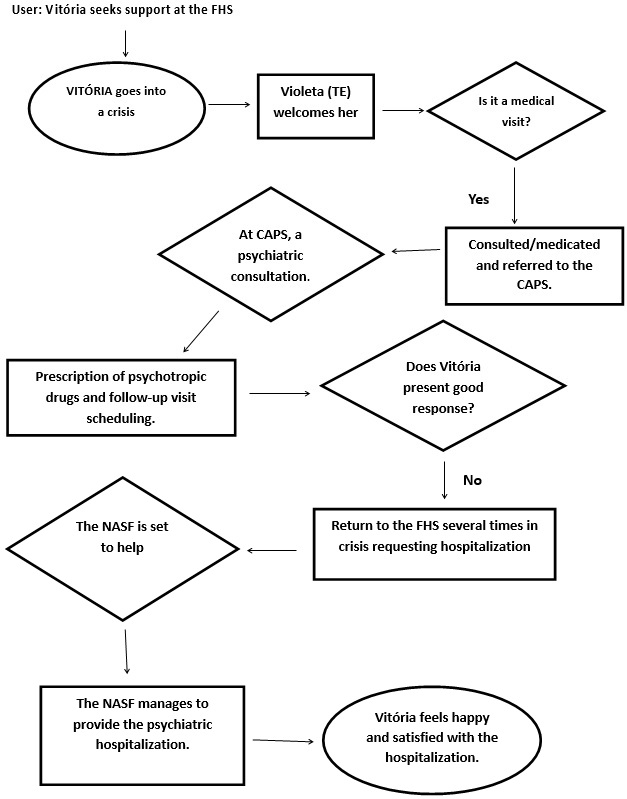
Figure 1: Flowchart to assess the care provided to a user with mental disorder. FHS, Cafelândia/SP.
ORIGINAL RESEARCH
Mental health care in primary care: a cartography
Taís Fernanda Maimoni Contieri SantanaI; Maria Alice Ornellas PereiraII
I
Nurse. PhD. Adjunct Professor. Fundação Paulista de Tecnologia e
Educação/Unilins. Lins, Brazil. E-mail: taiscontieri@gmail.com
II
Nurse. PhD. Adjunct Professor. Universidade Estadual Paulista. Botucatu,
Brazil. E-mail: malice@fmb.unesp.br
DOI: http://dx.doi.org/10.12957/reuerj.2018.32305
ABSTRACT
Objective: to map the daily care of patients with psychic disorders, the subjects of the mapping being the personnel of a family health unit and a family health support unit. Method: nine health professionals participated in this qualitative study in northwest São Paulo in mid-2013. Data were collected by case study, field diary, semi-structured interview and analytical flowchart. The project was approved by the research ethics committee. Results: results were captured and structured in three territories, of which the territory of doing was presented in this study. These evidenced the difficulties facing possible reversal of care, which is still based on the hegemonic medical model. Conclusion: there were obstacles to effective bonding, accountability and commitment by these professionals, making it hard to envisage advances in daily mental health practice, which hinders psychosocial rehabilitation.
Descriptors: Primary health care; geographic mapping; empathy; mental health.
INTRODUCTION
Over the decades, the search for improving health care in the country has been characterized by coping processes, challenges, and progresses. In this dynamics, the Family Health Strategy (FHS) has been collaborating, as this model of work prioritizes primary health care as an alternative to the disease-focused strategy, enabling managers, professionals, and users of the Unified Health System (SUS, as per its acronym in Portuguese) to understand the dynamics of places and subjects (individually and collectively), unveiling the social inequalities and health inequities, particularly in the field of mental health1.
A strong aspect of the Brazilian psychiatric reform consists in deinstitutionalization, a complex social process involving all the social actors and aiming at changing the form of organization of psychiatric institutions by creating structures to replace them. This is certainly an ongoing, dynamic process that requires changes in the models of health care, involving assistance to the family, aiming at integrating the individual into society, and seeking psychosocial rehabilitation. This is a process, a full exercise of citizenship aimed at improving the power of contract of individuals in the three major scenarios: habitat, social network, and a socially valued work2.
The reflection on the psychosocial field refers to the practices of reinsertion and permanence of the individual in social life, requiring a coordination of basic care with the new proposals of the services replacing psychiatric hospitalization3. When considering the scope of the transformation process of psychiatric care, it is important to mention that the treatment and care institution cease to mean only the prescription of drugs and the application of therapies, starting to deal with individuals rather than only with the disease; in this context, the FHS represents a relevant mechanism. It is also noteworthy that the World Health Organization (WHO) pointed out the importance of the integration of mental health actions in the Primary Care by recommending that the territory, community, and health services networks organize themselves in order to acknowledge that the mental health care is part of the primary health care, with emphasis in the new forms of providing care4.
Among the nuances of the care in the ESF, this study highlights that the main change consists in the fact that the care is no longer focused only on the individual and the disease, but also on the collective, with the family representing the privileged space of action5.
Emphasizing this aspect of providing care, it is important to mention that the users, as patients and producers of health needs, are complex, present qualitative forms of living, are collectives exposed to risks, need binding and welcoming meetings, present tension between autonomy and heteronomy to live their lives, have desires, and are also composed as biological bodies 6. Thus, considering the FHS in the context of the services, and specifically in mental health care for the assisted population, it is possible to affirm that this territory is considered an important space for care, as the family health teams represent powerful tools to offer comprehensive health care and as essential resources for mental health care in the community, contributing to the early identification and practicability of the treatment as well as to reduce the stigma related to patients with mental disorders"7.
However, this statement leads to some questions: How has the mental health care process been occurring in the community? How has the FHS been contemplating care in mental health? How have the professionals involved in this area been experiencing care?
In view of the above, the present study aimed at mapping the daily routine of the care provided to individuals with psychic disorders, with the health professionals of an FHS and of the Family Health Support Center (NASF) as subjects.
The precepts of care6 were used as the theoretical framework, based on the relationships between workers and users that permeate light technologies, as well as the work that supports the discussion pertinent to psychosocial rehabilitation2,3, building social contracts that enable users to subvert the seclusion process resulting from the effects of the mental disorder and social isolation.
METHODOLOGY
This project was carried out in accordance with Resolution CNS 466/12; it was assessed and approved by the Research Ethics Committee of the Medical School of Botucatu - Unesp under protocol number 4204-2012. The participants agreed to collaborate in this study by signing a free and informed consent form. For confidentiality and anonymity purposes, the code (E) followed by a numerical sequence was used to identify each interviewee.
This was a qualitative study using the observational case study design, field diary, semi-structured individual interviews, and an analytic flowchart. Based on the consideration of the case study, seen as a research category whose object is a deeply analyzed unit8 based on the daily routine of mental health care provided in the FHS, the field work aimed at an approximation with the subjects and provided elements of the daily routine performed by them.
The study was conducted during 2013, and the research site was an FHS unit in a city in the state of São Paulo belonging to the regional health sector VI, made up of a minimum team of professionals supported by an NASF I.
Nine professionals participated in the study; seven performed activities in the FHS: a nurse, a nursing aide, and five community health workers (CHW); all of them had passed the civil service examination and had at least two years of experience in the position. Also, two members of the NASF team participated: a nurse and a psychologist. Regarding the NASF professionals that participated: the nurse had been working in the area for 25 years and developed consulting service to the NASF, currently holding a management position in a mental health service in the neighboring municipality, and the psychologist was newly hired.
The questions included aspects related to the care performed by the subjects, as follows: How does the team provide care in mental health? How is the team-user-community relationship established? What benefits are provided, and what difficulties are faced? After the interviews, the participants agreed to schedule a meeting in order to create the flowchart. This was an important instrument for the development of the analysis of the collected material, as it supported the understanding of the user's path in the unit, from admittance to discharge9.
The tracer case was then considered. This method allowed the evaluation of the team's work process, reconstituting a case and allowing better observation of the action of providing care; as a result, it enabled the translation of the work process in the collective into a format that is visible and shareable by everyone10. In the perspective of processing the reading of the reality of the service with a focus on the care provided to individuals with mental disorders, mapping was found to be necessary, as this method is aimed at monitoring a process rather than representing an object9.
The work processes analyzed by mapping tools make it possible to capture the dynamic, live work, allowing the map maker, by means of a vibrating eye, to perceive the production in the health field based on its intensities and affected scope11. Mapping/cartography appears as a way of monitoring the course of treatment, perceiving the connections of networks or rhizomes and enabling the development of maps12.
RESULTS AND DISCUSSION
The interviews, the field diary, and the flowchart were analyzed and, subsequently, the content pertinent to the proposed objective was extracted for analysis. In the process of elaboration of the study, it was observed that the dynamic movements in effect in the institution, generated from the daily work, started to take shape, as well as the continuous movement of territorialization, deterritorialization, and reterritorialization. The analytic flowchart revealed, through the speech of the team, the path taken by a patient with a psychic disorder; from her admittance to the unit and the provided care up to her discharge.
Description of the analytic flowchart
Initially, the team elected a tracer case that enabled the visualization of the course of treatment of a patient who was given the fictitious name Vitória. She was thirty years old and diagnosed with schizophrenia; she was a user of the reference psychosocial care center (CAPS) of the FHS unit, presented records of a number of hospitalizations in psychiatric institutions, and had suffered from seclusion, prejudice, and sexual abuse by her father.
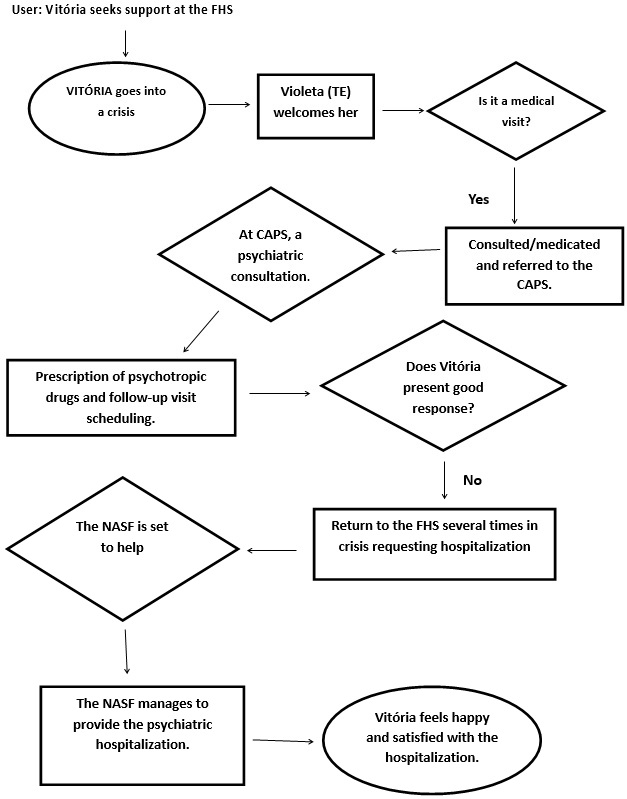
Figure 1:
Flowchart to assess the care provided to a user with mental disorder. FHS,
Cafelândia/SP.
Following the creation of the flowchart, the participants described and discussed the path taken by Vitória in the unit, and reflected about the organization of the work process.
Admittance
The patient was welcomed by the nursing technician together with the community health workers. Considering that the reception of the patient into the unit is an important factor, the following report was obtained:
[...]I want them to know that they may rely on me, even when it is not my area. I think they rely on my work . (E1)
The FHS is the only health care unit in the neighborhood, which has families living in precarious situations from the economic and social perspectives. Regarding the situation of Vitória, the user has free access to the professionals; she has always contacted them during her crisis episodes. In the meeting that generated the flowchart the community worker acted as a link between the unit and the micro area where the user lives. Vitória has always wandered the streets looking for food and affection, and in a number of occasions, she spent the night away from home.
Menu
In the FHS the service consisted in a medical consultation (general practitioner) with the prescription of psychotropic drugs and referral to the CAPS I. Prior to the data collection of this study, group meetings and therapeutic workshops used to take place, but such activities ceased to occur.
The family was approached and guided by the team. The FHS professionals were invited to participate in activities in the NASF, which included training and craft workshops approaching themes related to mental health, particularly regarding rehabilitation. According to the team, craftsmanship was aimed at reducing the idleness among users, as well as providing them with a source of income. Despite being invited, Vitória has never participated in these activities. The subjects reported that Vitória, in a number of occasions, went to the house of the professionals of the FHS and the NASF seeking support.
The decision-making process
Decision-making moments were the most traumatic, as the team felt deprived of the resources required to take action. These resources include lack of knowledge about what to think and how to act. Based on the psychic disorder medical diagnosis, the FHS team received matrix support from the NASF, establishing service protocols. Cases considered critical were referred to the CAPS I of the neighboring municipality, as the city where the studied FHS is located did not have the mentioned service.
The team concluded that hospitalization was the best decision for the situation of Vitória; it was referred to as home, as the family did not accept her and the team considered that her crisis episodes had occurred due to the lack of regular use of psychotropic drugs. A new proposal of care, considered more reasonable, was then initiated: a struggle so that Vitória could be hospitalized. At the time, the crisis episodes were aggravated. Therefore, the team believed that the best place to welcome her would be the psychiatric hospital of the neighboring municipality. (reports of E1)
Discharge
The discharge of a user is experienced by the team when there is an improvement of a condition related to the organic aspects or associated with mental disorders. Seemingly this was the moment seen by the group as a moment of accomplishment and satisfaction for a work completed. Vitória had been in a psychiatric hospital for more than a year, using medications and, according to the team, presenting no crisis episodes. According to the report, in the hospital Vitória was able to participate in therapeutic groups and crafts workshops, talked without being aggressive, her psychic symptoms were significantly reduced, and body hygiene was constant.
The establishment of territories13 was considered in the process of creation of the material to be analyzed, followed by the follow-up of the reality experienced by the individuals. A relationship in which researcher-map maker/cartographer and research territory were constituted in the same process was established, questioning the senses of the movements that were produced in the act of researching and expressing their singularities14.
Working with the territory means investing in the creation of care alternatives, focusing on where the individuals live and develop relationships and how much these places show their singularities, diversities, and realities, essential conceptions for care in the psychosocial field15. Thus, the development of a mapping of the care provided by the professionals considered the territory of the doing, of thinking this doing, and the challenges faced. This paper is part of a broader investigation, the product of a master's thesis, and approached only the territory of doing.
During the development of this study, the dynamics of the professionals was monitored, and teamwork with a significant participation of the CHW was observed. The FHS teamwork is essential so that the following attributions common to all professionals may be fulfilled: provide health care and take responsibility for the respective population. Among the actions of the CHW, the study highlights: qualified listening, performing the role of an educator, through home visits and reception of the needs of the families, as well as pointing out the health and social vulnerabilities of these families1.
In the care process, the CHW represents a unique figure in the first team-community contact, being responsible for the link and bond, considering as a dweller and component of this territory explored by the mapping tools16, and also a protagonist of this reality.
However, bonding is a phenomenon that exists in both the individuals involved in each relationship, and it is affected by the ties previously experienced by them17.
The patient presented in the flowchart came from a humble family, with scarce resources, and a history of psychic disorders in relation to her mother and siblings. In her home the quarrels were constant; she was rejected by her family, sometimes being forced to sleep in a mattress in the porch of the house. Such situation was witnessed by the FHS team when they visited her to deliver her medicines (psychotropic drugs). The reports elaborated by the professionals during the interviews pointed out the difficulty in the creation of bonds regarding mental health:
[...]it is very difficult here, patients seek our service when they need help, and in a number of cases, we are unable to help them. When we go to their houses, sometimes we do not know how to act. The family does not collaborate, it is difficult [...] (E2)
The creation of bonds between each user and a team or a professional represents the possibility of spaces for exchanges, which are necessary in mental health care. Actions in mental health are assumed in the daily life, emerging with sensitivity, responsibility, welcoming and qualified listening, and how these senses affect the care provided and the place that each one, professional and user, assumes in the relationship18. The initial menu of Vitória, just like for other patients with psychic disorders that came to the unit, was always permeated by the medical consultation and prescription of drugs, as observed in the report below:
[...] care that comes to us here is the following: the patient comes with this problem, we schedule an appointment with the doctor, they see the doctor, a general practitioner, who prescribes drugs and refers them to the CAPS, right? [...] (E1)
Therefore, mental health care in the context of this study is mixed, or even limited, to the production of consultations and exams. Continuing the course of Vitória, according to a report of the team, her visits to the FHS became frequent; when she approached the entrance gate of the service, the professionals used to be apprehensive, as they could not know whether she was in crisis. Her medical records showed data of five hospitalizations (precautionary interdiction) in psychiatric hospitals, with an average stay of thirty days; the discharge reports always showed an improvement of the clinical condition.
The model of treatment based on the asylum institutions model has been discussed, criticized, and refuted in the last decades, as this paradigm undoubtedly generates isolation and the deposit of people in the respective institutions. However, in a historical leap, limitations in the treatment and care19 still persist. The contacts during the course of the study and the notes in the field diary evidenced reports that in that unit there was nothing to be done regarding the treatment of individuals with mental disorders:
[...]there is no appropriate place here, so you see no improvement! (E1)
[...]in this city we do not have the proper service, we have to refer them to specialized centers [...] (E3)
The difficulty to understand/define the psychic disorder was also observed:
[...] formerly we had an alcoholics anonymous center next to us, many people went there, we knew who they were, they had mental problems too, the community people did not know that they had problems, because some people with mental disorders are apparently normal, so I think that a specific place to provide this type of service is necessary[...] (E4)
The fragility of the team in the care context is evidenced, with multiple feelings; the need to do something mixes with the impotence that restricts them. Apparently, the team was not able to define the concept of rehabilitation in the daily routine of care; they felt deprived of resources and of a specialized place to provide mental health care.
At this moment, care fragility was expressed, contractuality and responsibility were broken, as well as the relationships of bonding and welcoming, and the need for light technologies was reinforced7. For the effectiveness of the actions established in the FHS teams, including for mental health care to be incorporated into daily practices, it is necessary to broaden clinical and epidemiological knowledge rather than remaining limited to diagnoses and medications. A more incisive performance by the teams is relevant, with a focus on the singularity of care, breaking the strong tendency to the observation of the biomedical model as a rule for the establishment of care20.
Rehabilitation, as a strategy, enables the recovery of the ability to generate sense; thus, the task of the mental health service consists in helping individuals that, at a given moment of their lives, have lost the capacity to generate sense, following-up them in the recovery of non-protected but socially open spaces for the production of new senses2.
The FHS team points out the need for investments to expand mental health care.
[...]so, we need a vehicle, trained professionals, a place, not only the physical structure, but also a place where they could develop activities so they could talk to the professionals[...] (E2 and E1)
That which is offered by the services, physical and material resources, organizational characteristics, and the type of work of the team are considered major variables in the progress of the mental disorder, and together with the individual resources of the patient and the context in which they are inserted, perform a key role in the success or failure of a treatment.
Affirming the importance of the context and the complexity of the users, who can no longer be reduced to a diagnostic category, there was an important inversion in the logic of thinking about the treatments by suggesting the adoption of a praxis that, by recognizing the resources of each individual, assumes the role of following them up in the process of building spaces for negotiation and redemption of the citizenship20.
Therefore, the expectation is to overcome the difficulties in the organization of teamwork, expand the clinics with a focus on the subject, and go beyond the traditional care, whose operation is bureaucratized and centered in the physician.21
The team should understand individual in psychological distress, and such ability to understand should lie in how they apprehend the presented demands and needs. Singularity is produced in the face of forces such as illnesses, aspirations, and interests, just like work, culture, family, and social networks.
CONCLUSION
Based on the cartography of the FHS care it was possible to understand that the professionals of the community services are increasingly the main providers of mental health care. In turn, cartography made it possible to capture the difficulties inherent to the possibility of reversion of the hegemonic model proposed by the public policies, as well as the implementation of the principles of the Unified Health System. It was also observed that the professionals presented feelings of impotence, anxiety, affliction, and tension in the face of the delivery of mental health care, as well as they evaded from providing care, assigning it to other spheres, denying their responsibility.
In view of the results presented, this study suggests that the team rethink the solvability of their actions in health regarding bonding, co-participation, and engagement, thus making the prerogatives pertinent to psychosocial rehabilitation prevail so that the participation of professionals becomes essential, with an emphasis on the multidisciplinary, interdisciplinary teamwork, reinforcing the production of humanized care and, consequently, providing modes of interventions that are more appropriate to the actual needs of individuals with a psychic disorder.
REFERENCES
1.Gondim GMM, Monken M. Territorialização em Saúde. Escola Nacional de Saúde Pública. Fundação Osvaldo Cruz [Internet]. 2012 [cited 20 Sep 2018]. Available from: http://www.epsjv.fiocruz.br/upload/ArtCient/25.pdf
2.Saraceno B. Libertando identidades: da reabilitação psicossocial à cidadania possível. Rio de Janeiro (RJ): Te Corá/Instituto Franco Basaglia, 2001.
3.Amarante P. Teoria e Crítica em Saúde Mental - Escritos Selecionados. Rio de Janeiro: Zagodoni, 2015.
4.Wenceslau LD, Ortega F. Saúde mental na atenção primária e saúde mental global: perspectivas internacionais e cenário brasileiro. Interface (Botucatu, Online) [Internet]. 2015 [cited 20 Sep 2018] 19(55):1121-32. Doi: http://dx.doi.org/10.1590/1807-57622014.1152
5.Câmara MC, Pereira MAO. Percepções de transtorno mental de usuários da Estratégia Saúde da Família. Rev Gaúcha Enferm. 2010; dez. 31(4): 730-7.
6.Merhy EE. Saúde: a cartografia do trabalho vivo. São Paulo: Hucitec, 2007.
7.Souza J, Almeida LY, Luis MAV, Nievas AF, Veloso TMC, Barbosa SP, et al. Mental health in the Family Health Strategy as perceived by health professionals. Rev Bras Enferm [Internet]. 2017 [cited 2017 Oct 10] 70(5): 935-941. Doi: http://dx.doi.org/10.1590/0034-7167-2016-0492
8.Merhy EE, Franco TB. Cartografias do trabalho e cuidado em saúde. Tempus: Actas de Saúde Coletiva [Internet]. 2012 [cited 29 Sep 2018] (6):151-163 Doi: http://dx.doi.org/10.18569/tempus.v6i2.1120
9.Kessner DM, Carolyn EK, James S. Assessing health quality-the case for tracers. N Eng J Med [Internet]. 1973 [cited 2016 Jan 15] 288(4): 189-194. Doi: http://dx.doi.org/10.1056/NEJM197301252880406
10.Kastrup V. O funcionamento da atenção no trabalho do cartógrafo. In: Passos E, Kastrup V, Escóssia L(org). Cartografias e devires: a construção do presente. Porto Alegre: Sulina; 2010.p.32-51.
11.Franco TB, Magalhães Júnior HM. Integralidade na assistência à saúde - a organização das linhas do cuidado. In: Merhy EE, Magalhães Junior HM, Rimoli J, Franco TB, Bueno WS. O trabalho em Saúde: olhando e experienciando o SUS no cotidiano. 4ª ed. São Paulo (SP): Hucitec, 2007. p.125-33
12.Kastrup V, Passos E. Cartografar é traçar um plano comum. Fractal: Revista de Psicologia, Niterói, n. 2, v. 25, p. 263-280, maio/ago. 2013.
13.Gonçalves CAV, Machado AL. Cartografia do cotidiano de cuidados à pessoa com depressão. Sau & Transf Soc 2011; 1(3): 68-76.
14.Passos E, Barros R. B.In: Passos E, Kastrup V, Escossia L. Pistas do método da cartografia: pesquisa-intervenção e produção de subjetividade. Porto Alegre: Sulina; 2015.
15.Silva AB, Pinho LB. Território e saúde mental: contribuições conceituais da geografia para o campo psicossocial. Rev. enferm. UERJ. Rio de Janeiro, 2015. [cited 29 Sep 2018] mai/jun; 23(3):420-4. Doi: http://dx.doi.org/10.12957/reuerj.2015.10091
16.Franco TB, Merhy EE. Atenção domiciliar na saúde suplementar: dispositivo da reestruturação produtiva. Ciênc. saúde coletiva, 2008. [cited 15 Jan 2018] (13)5:1511-20. Doi: http://dx.doi.org/10.1590/S1413-81232008000500016
17.Willrich JQ, Kantorski LP, Antonacci MH, Cortes JM, Chiavagatti FG. Da violência ao vínculo: construindo novos sentidos para a atenção à crise. Rev. Bras. Enferm. [Internet]. 2014 [cited 12 Dec 17]. 67(1):97-103. Doi: http://dx.doi.org/10.5935/0034-7167.20140013
18. Martines WRV, Machado AL. Produção de cuidado e subjetividade. Rev Bras Enferm [periódico na internet]. 2010 [cited 22 Aug 2012];63(2):328-33. Available from: http://www.scielo.br/pdf/reben/v63n2/25.pdf
19.Garcia APRF, Freitas MIP, Lamas JLT, Toledo VP. Nursing process in mental health: an integrative literature review. Rev Bras Enferm [Internet]. 2017[cited 2017 oct 15].70(1):209-18. Doi: http://dx.doi.org/10.1590/0034-7167-2016-0031
20.Saraceno, B. Libertando identidades: da libertação psicosssocial à cidadania possível. Rio de Janeiro: Te Corá/ Instituto Franco Basaglia; 2001.
21.Corrêa VAF, Acioli S, Mello AS, Dias JR, Pereira RDM. Projeto Terapêutico Singular: reflexões para a enfermagem em saúde coletiva. Rev enferm UERJ, Rio de Janeiro, 2016 [cited 29 Sep 2018]. 24(6):e26309. Doi: http://dx.doi.org/10.12957/reuerj.2016.26309