Source: Sheet of National Notification of Injury Information System (SINAN – "Sistema de Informação de Agravos de Notificação")
ORIGINAL RESEARCH
Epidemiological, clinical and quality of life profiling of children with leprosy in a hyperendemic municipality
Hermaiza Angélica do Bonfim LoiolaI; Dorlene Maria Cardoso de AquinoII; Luciane Sousa Pessoa CardosoIII; Maria de Fátima Lires PaivaIV; Nair Portela Silva CoutinhoV; Rosilda Silva DiasVI
I
Nurse. MS. Federal University of Maranhão. Brazil. E-mail: hermaizaloiola@hotmail.com
II
Nurse. PhD. Associate Professor. Federal University of Maranhão. Brazil.
E-mail: dmcaquino@gmail.com
III
Nurse. Specialist. Master's Degree course student Federal University of
Maranhão. Brazil. E-mail: lucianesousa1602@gmail.com
IV
Nurse. PhD. Adjunct Professor. Federal University of Maranhão. Brazil.
E-mail: fatimalires@gmail.com
V
Nurse. PhD. Adjunct Professor. Federal University of Maranhão. Brazil.
E-mail: nairportelaufma@gmail.com
VI
Nurse. PhD. Adjunct Professor. Federal University of Maranhão. Brazil.
E-mail:
rsilvadias@ig.com.br
VII
Master's Degree thesis Cutout
Epidemiological, clinical profile and quality of life of children
with leprosy children in a hyperendemic municipality of Maranhão. Federal University of Maranhão, 2017.
DOI: https://doi.org/10.12957/reuerj.2018.32251
ABSTRACT
Objective: to examine the epidemiological, clinical and quality of life profile of children with leprosy in a hyperendemic municipality. Methods: In this descriptive study of children from 5 to 14 years old notified with leprosy, data were collected between 2015 and 2016, by documentary analysis of Leprosy notification records and application of CDLQI. Of the study population of 48 children, 40 were interviewed. Descriptive data analysis results were presented in absolute and percentage frequencies, and CDQLI scores. The project was approved by the research ethics committee. Results: mostly males, aged from 12 to 14 years, brown skin color, multibacillary operational classification, dimorphic clinical form, and disability grade zero at diagnosis more than half with some impairment by CDQLI. Conclusion: transmissible forms of tuberculosis were present in high frequencies, and the quality of life of the under-15s studied was impaired.
Descriptors: Leprosy; epidemiology; quality of life; health of the child.
INTRODUCTION
Leprosy is still a serious public health problem in Brazil, since it is the only country in Latin America that has not reached the goal of eliminating the disease, stipulated by the reduction of the prevalence coefficient to less than one case per ten thousand inhabitants.1
In Brazil, the average of detection of leprosy in children under 15 years old was 5.77 per 100 thousand inhabitants, and Maranhão is still considered one of the hyperendemic states regarding leprosy, especially in relation to cases of children with the disease, with a prevalence coefficient of 17.56 per 100,000 inhabitants in children under 15 years old.2
Currently, the effective control of leprosy has as limitations the fact that the disease has a long incubation period, the high number of cases, the stigma that the disease determines and the remaining sequelae of the clinical condition. Thus, the relentless search for contacts in leprosy is an effective method for the early diagnosis of the disease, it is possible to reduce the sources of infection and to interrupt the transmission of the disease, especially in childhood, when it is easier to detect the source through the delimitation of the family life.3
Chronic skin diseases, such as leprosy, have been observed not only from the physical point of view, but also from the psychosocial aspects that are affected by emotional and social factors, affecting the patients' quality of life.4
The child, for being in continuous process of development and growth, by presenting bodily or behavioral changes, or even any condition that threatens their bodily integrity and self-image, will be perceived differently and will require age-specific defense and adaptive mechanisms. In addition, loss of safety can cause damage to one's own development, reflecting on their adult life.5
Large-scale impacts on the lives of patients with leprosy may interfere with their quality of life. Due to this problem, scholars began to worry about the quality of life of these patients and to evaluate these impacts through questionnaires appropriate for pediatric use.6
Data on leprosy in children under 15 years old in the state of Maranhão, which is still considered high and hyperendemic, have aroused interest in studying the disease, especially in children's health. The present study is valid because the children's public is the most susceptible to changes in their living standard, which may result in impairment of their development over the years, and it may be detrimental to their quality of life.
This study aimed at analyzing the epidemiological, clinical profile and quality of life of children with leprosy in a hyperendemic municipality.
LITERATURE REVIEW
The Mycobacterium leprae was discovered in 1873 by the researcher Gerhardt Henri Armauer Hansen, and belongs to the Actinobacteria class, subclass of Actinobactereridae, order ofActinomicetalis, suborder of Corynebacterineae, of theMycobacteriaceae family, gender Mycobacterium, and of theLeprae species, being better known as Hansen's Bacillus.7
Due to the fact that leprosy is a disease with diverse clinical manifestations and diverse characteristics, there was a need to adopt a standard classification for the disease; thus, in 1953, it was proposed at the VI International Leprosy Congress the classification of Madrid, being the most used by the health services for the definition of clinical forms that can be paucibacillary or multibacillary, and its respective subdivisions which was based on four criteria: clinical, bacteriological, immunological and histological.5,8
In childhood, leprosy may result in disabilities, deformities, or neurological damage, as it first strikes the peripheral nerves. This would be a benign nature disease, but the late diagnosis in the endemic areas results in the inadequacy of the therapeutic choice. The presence of disabilities at the time of the diagnosis is an indication that the early detection of the disease may be faulty.9
The diagnosis of leprosy begins with the clinical and epidemiological examination of the individual with the suspected disease; the historical and life conditions analysis and the dermatoneurological examination are performed to identify lesions or skin areas with changes in the sensitivity and impairment of peripheral nerves.9,10
The diagnosis is also based on the bacilloscopic examination, plus the anatomopathological examination and the pilocarpine and histamine tests.11
In children, a careful examination should be performed, given the difficulty of applying and interpreting the sensitivity tests. In this regard, the Ministry of Health recommends that the complementary protocol for the diagnostic investigation of cases of leprosy in children under 15 years old - PICD <15 suggested by Technical Note PNCH/SVS, No. 14/2008. 10,11
The treatment of leprosy is fundamental to interrupt the transmission of the disease, besides being strategic for its control and elimination. It is performed through polychemotherapy (PCT) and follow-up of the individual during the treatment, in order to diagnose and treat the complications that may occur during or after the PCT. It also serves to prevent disabilities and physical deformities arising from the disease.12 In children, the drug therapy is adjusted according to age and weight.13
Studies on chronic skin diseases have been observed not only from the physical point of view, but also from the psychosocial aspects that are influenced by emotional and social factors affecting the patients' quality of life.4
The World Health Organization has defined quality of life as "the individual's perception of their position in life, in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns".14:1405
Because this definition is generic, the World Health Organization could not find application of this concept clinically or scientifically, being replaced by health-related quality of life. This concept is more restricted and easy to measure, as it is directly and specifically related to the state of health, excluding freedom, belief and environment, besides being of paramount importance to the health area for contributing as a guide for treatments and evaluations of the care provided.15
It can be stated that the best way to measure quality of life during treatment comes from the need to prolong life, relieve pain, restore the function and prevent disability in patients.16
The importance of delimiting the quality of life in health is something unquestionable in the present days, given the real need that the individual has to control their way of living and their state of health, as a way to help them cope with the disease.17
There are several instruments used to measure the quality of life of an individual, the difference between them consists in the focus that each one has, how to measure the individual satisfaction in relation to the expectations of the subject, physical, social and mental domains; and those who describe the state of health of this individual, and have a tendency to divide them into dimensions or domains of health.17
The quality of life in domains or dimensions can be subdivided into emotional (anxiety, depression), physical (daily activities, mobility), social (family life, social contact), work, pain and other symptoms.18
In relation to pediatrics, in 1995 the Children's Dermatology Life Quality Index (CDLQI) questionnaire was developed and analyzed. It is intended for use in children between the ages of 4 and 16, who carry various skin diseases, and addresses the events of the last week of the child's life.19,20
METHODOLOGY
This is a descriptive epidemiological study, with a quantitative approach, carried out in the municipality of São Luís - Maranhão (MA) . The study population was composed of children between 5 and 14 years old, of both sexes, living in São Luís - MA, who were in active registry of the disease.
The data were collected in 2015 and 2016 through a Protocol Sheet, based on the Notification/Investigation of Leprosy Sheet of the National Notification of Injury Information System (SINAN – "Sistema de Informação de Agravos de Notificação"), containing socioeconomic and demographic variables and clinical conditions. For data on the quality of life of children with leprosy, the instrument CDLQI 6developed and validated for use in Brazil was used.5
The registries in the health units that have the Leprosy Control Program were searched, and it was identified 160 cases in children under 15 reported in the years 2014 and 2015. Of these, 59 were not living in the municipality of São Luís, 34 were not in an active registry, and 21 were outside the acceptable age range for study participation. Thus, 46 children under 15 years old who were affected by leprosy were included in the study, of whom, only 40 were treated during the data collection period, since, on the days scheduled for return, the children did not attend.
In the days foreseen for the return of the children to the units, parents and children were approached, the purpose of the research was explained and, in case of acceptance of participation in the research, the Free and Informed Consent Term was signed by the adolescents and their caregivers. Subsequently, the protocol sheet was filled out through the Notification/Investigation of Leprosy Sheet of the National Notification of Injury Information System (SINAN) attached to the patient's medical record and the CDLQI was applied, which was answered by the child, and when necessary , with the help of their parents.
The clinical classification adopted in the study was recommended by the World Health Organization and registered in the SINAN Notification/Investigation Sheet known as Madrid classification (Paucibacillary Clinical Form: Undetermined and Tuberculoid; and Multibacillary: Dimorphic; and Virchowian), and the degree of disabilty were those established by the Ministry of Health.10
The data were typed into a database in Excel and analyzed in the EPI-Inf Program by means of descriptive statistics, in absolute and percentage frequencies, presented in tables. The quality of life results were evaluated according to the obtained scores: without impairment of quality of life (0 - 1) or with mild (2 - 5), moderate (6 - 10), severe (11-20) , or very severe (21 - 30) impairment.
This study is part of a larger project, which was authorized by the Municipal Health Department, by the State Health Department of the State of Maranhão and approved by the Research Ethics Committee of the University Hospital of the Federal University of Maranhão, with opinion number 1,227.248. The research was developed in accordance with the Resolution 466/12 of the National Health Council for Research with Human Beings, using the Free and Informed Consent Term with those responsible for the clients and adolescents.
RESULTS AND DISCUSSION
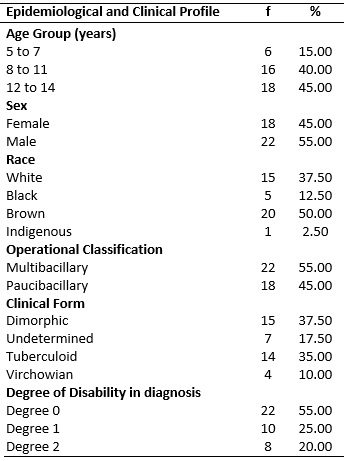
The study included 40 children affected by leprosy, 22 (55%) male, 18 (45%) aged from 12 to 14 years old, and 20 (50%) brown-skinned. Regarding the clinical characteristics of leprosy, 15 (37.50%) had the clinical dimorphic form, 22 (55%) had a multibacillary operational classification, and 22 (55%) had a degree of disability at diagnosis, as shown in Table 1.
TABLE
1: Children aged from 5 to 14 years old affected by leprosy, according to
epidemiological and clinical data. São Luís - MA, 2016 (N= 40).
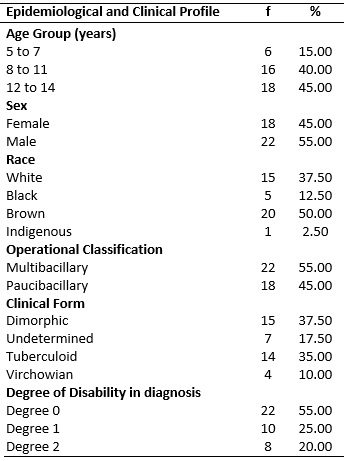
Source: Sheet of National Notification of Injury Information System (SINAN
– "Sistema de Informação de Agravos de Notificação")
In the analysis of the children's quality of life, it was possible to observe a higher frequency of moderate impairment (40%), followed by no impairment (25%), mild impairment (18%) and severe impairment (17%), according to Table 2.
TABLE 2: Quality of life of children aged from 5 to 14 years old affected by
leprosyaccording to the CDLQI classification*. São Luís - MA, 2016 (n =
40). 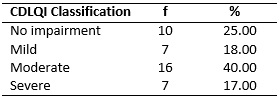
*
Children's Dermatology Life Quality Index
(CDLQI) Instrument
The results of the study showed a higher frequency of the disease in children aged from 12 to 14 years old, and brown-skinned. Leprosy in childhood does not have a differentiated prevalence rate in relation to sex, however, some authors affirm that the incidence of the disease in males is greater, a result that has corroborated other studies carried out in the Northeast Region, from 2001 to 2011.21,22
In a study carried out in the state of Goiás, data were identified regarding new cases of leprosy from the year 2009 to 2013, with a higher occurrence in children from 5 to 9 years old, and from 10 to 14 years old, all of school age.23
Regarding the predominance of the brown-skinned race, this can be directly related to the process of colonization of Brazil and the mixture of races. The miscegenation of races in Brazil may have generated a genetic profile that contributes to the incidence of leprosy in people who are brown-skinned.24
In this study, in relation to the clinical characteristics, there was a prevalence of multibacillary leprosy in children, although this clinical form is less prevalent in children. Studies have reported that it is quite possible to find multibacillary forms in children, with a higher frequency in endemic areas, probably because the symptoms of the disease are confused with the common childhood skin diseases and there is an inefficient early detection of the disease.24
Regarding the epidemiological profile of leprosy in Brasília - DF, there was a predominance of the dimorphic clinical form, in agreement with the present study, demonstrating the need for prevention and expansion of disease control actions, such as the examination of the community, which consists of the active search in schools.25
Several factors contribute to the high incidence of the disease and difficult control in Brazil, such as delayed diagnosis, lack of control of communicants, abandonment of therapy, reduced level of clarification, poor living conditions, poor health care coverage and prejudice.26,27
When analyzing the degree of disability at the time of diagnosis, prevalence was observed at degree 0, but this fact does not exclude other limitations that may be caused by the disease. In agreement with the data obtained in this study, authors affirm that at the moment of diagnosis, if the patient has a degree of disability zero, other limitations should not be excluded, since the disease generates several physical disabilities. And when diagnosed early, there are no disabilities, which appear with the increase over time in the duration of the disease without treatment. 25,26,28,29
Regarding the degree of disability, the percentage of children with degree 1 and 2 of disability was higher than that reported in a study carried out in the state of Ceará, where it was observed that the frequency of disabilities of degrees 1 and 2 in the 15-year old age group was of 2 (0.7%) cases, and there was a higher prevalence of physical disabilities in people with the multibacillary clinical form.30
The analysis of the quality of life in children and adolescents is complicated, considering that in the literature few studies are related to this theme. However, there is a growing scientific interest in working with the quality of life of children and adolescents.30
Regarding the quality of life impairment of the children in this study, according to the classification proposed by the CDLQI, there was a predominance of moderate impairment, followed by the category without impairment. It is worth mentioning that in a study with patients with leprosy, in the age group of 5 to 14 years old, the quality of life was also compromised.30
Nowadays, there is a greater concern regarding aesthetics and, therefore, attention should be paid to children who show feelings of inadequacy, stigmatization and impaired social interaction. These children tend to move away from people or vice versa because they believe the disease may be contagious or the result of injury.30
Other researchers also corroborate this statement by reporting that the impact on the quality of life of patients with leprosy is aggravated by the association of the disease with the social stigma that current societies still cultivate in relation to it, treating it as chatoyant and incurable, resulting in discrimination and exclusion from social life.9
Prejudice against individuals with leprosy is associated with the lack of knowledge about elements related to the disease, such as their mode of transmission, existence of a treatment and cure. The history of stigma and prejudice, in addition to the lack of information, incites fear in the uninformed people, leading to the social exclusion of the patient. 28 A study carried out in Natal-RN, with relatives of people with leprosy, identified among the participants stigma, prejudice and social exclusion experienced by them, reinforcing the need for greater attention to the person affected by leprosy and their families.31
For a full recovery of the health of patients with leprosy, especially children, multidisciplinary therapy is necessary to visualize the physical, psychological and social issues of this patient, as well as decisions that intend to reduce the impact of the disease on their quality of life.30-32
CONCLUSION
The sociodemographic and clinical profile of the 40 children is characterized by the prevalence of male, brown-skinned, multibacillary operational classification, the dimorphic clinical form and the Zero Degree of Disability in the diagnosis.
The quality of life of most children was compromised, with more moderate impairment, followed by mild and severe impairment.
The recovery of leprosy patients comprises the multidisciplinary therapy, encompassing psychophysical and psychosocial aspects, to overcome the impact of the disease on the quality of life of these clients, including the stigma and prejudice that increase the human suffering and lead to social exclusion.
As a limitation of the study, the difficulty of the children to return to the Unit to give continuity to treatment and, consequently, to the research, even with prior scheduling and guidance to parents/guardians on the importance of the return.
REFERENCES
1.Ministério da Saúde (Br). Secretária de Vigilância em Saúde. Hanseníase, verminose e tracoma tem cura: a experiência de uma campanha integrada. Boletim Epidemiológico. Brasília (DF); SVS;2016.
2.Schnneider PB, Freitas BHBM. Tendência da hanseníase em menores de 15 anos no Brasil. Cad. Saúde Pública (Online). 2018; 34(3):2001 – 16. e00101817.
3.Pires CAA, Malcher CMSR, Abreu Júnior JMC, Albuquerque TG, Corrêa IRS, Daxbacher ELR et al. Hanseníase em menores de 15 anos: a importância do exame de contato. Rev. paul. pediatr. (online). 2012; 30(2):292-5.
4.Santos DCMD, Nascimento, RDD, Gregório VRDN, Silva MRFD. A hanseníase e o seu processo diagnóstico. Hansen. int. (Online). 2017; 32(1):19-26.
5.Barreire SG, Oliveira OA, Kazama W, Kimura M, Santos, VLCG. Qualidade de vida de crianças ostomizadas na ótica das crianças e das mães. J. Pediatr, 2003; 79(1):55-62.
6.Prati C. Validação para o português falado no Brasil do instrumento escore da qualidade de vida na dermatologia infantil (CDLQI) [dissertação de mestrado]. Porto Alegre (RS): Universidade Federal do Rio Grande do Sul; 2007.
7.Madeira S. Aspectos microbiológicos do Mycobacterium leprae. In: Opromolla DVA. Noções de Hansenologia. Bauru(SP): Centro de Estudos Dr. Reynaldo Quagliato; 2000. p. 66-9.
8.Garbino JA. Neuropatia hanseniana: aspectos fisiopatológicos, clínicos, dano neural e regeneração. In: Opromolla DVA. Noções de Hansenologia. Bauru (SP): Centro de Estudos Dr. Reynaldo Quagliato; 2000. p. 89-99.
9.Nery JADC, Nascimento, MB, Gusmão MBN, Figueiredo LT. Manuseio do eritema nodoso hansênico em pacientes pediátricos. Pediat. mod. 2013; 49(1):22-4.
10.Ministério da Saúde (Br). Portaria nº 125, 26 de março de 2009. Secretaria de Vigilância em Saúde (SVS) .Ações de controle da hanseníase. Brasília (DF). Gabinete Ministerial; 2009.
11.Almeida JA, Almeida SND, Magalhães HM. Avaliação e tratamento dos membros inferiores para a prevenção de incapacidades. In: Opromolla DVA, Baccarelli R. Prevenção de incapacidades e reabilitação em hanseníase. Bauru (SP): Instituto Lauro de Souza Lima; 2003. p. 112-5.
12.Budel AR, Costa CF, Pedri LE, Raymundo AR, Gerhardt C. Perfil dos pacientes acometidos pela hanseníase atendidos no ambulatório de dermatologia do hospital evangélico de Curitiba. An. bras. dermatol (online). 2011; 86(5):942-6.
13.Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Diretrizes para vigilância, atenção e eliminação da Hanseníase como problema de saúde pública: manual técnico-operacional [recurso eletrônico] Brasília (DF): SVS; 2016.
14.Whoqol Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc. sci. med. 1995; 41(10):1403-09.
15.Cótica EFA. Perfil clinico-epidemiológico e qualidade de vida em crianças e adolescentes portadores de hanseníase no município de Palmas – TO [master thesis]. Brasília (DF): Universidade de Brasília; 2010.
16.Dantas RAS, Sawada NO, Malerbo MB. Pesquisas sobre qualidade de vida: revisão da produção cientifica das universidades públicas do Estado de São Paulo. Rev. latinoam. enferm. (Online). 2003; 11(4):532-8.
17.Finlay AY. Quality of lifes indices. Indian j. dermatol. Venereol. Leprol. 2004; 70(3):143-8.
18.Misery L, Finlay AY, Martin N, Bousseta S, Nguyen C, Myon E. et al. Atopic dermatitis: impact on the quality of life of patients and their partners. Dermatology. 2007; 215(2):123-9.
19.Laaksonen C, Aroma M, Heinonen OJ, Suominen S, Salanterã S. Paediatric health- related quality of life instrument for primary school children: cross – cultural validation. J. adv. nurs. 2007; 59(5):542-0.
20.Lewis-Jones S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema. Int. j. clin. pract. 2006; 60(8):984-92.
21.Sousa NP, Silva MIB, Lobo CG, Barboza MCC, Abdon APV. Análise da qualidade de vida em pacientes com incapacidades funcionais decorrentes de hanseníase. Hansen int. (online). 2011; 36(1):11-6.
22.Cecilio RSF. Perfil clinico-epidemiológico da hanseníase no município de Irecê- Bahia, período de 2001-2011 [monografia]. Salvador: Universidade Federal da Bahia; 2012.
23.Freitas BHBM, Cortela DDCB, Ferreira SMB. Tendência da hanseníase em menores de 15 anos em Mato Grosso (Brasil), 2001-2013. Rev. saúde pública (Online).2017; 51(28):1-10.
24.Talhari S., Torrecila MAA, Talhari, AC. A study of leprosy and other skin diseases in school children in the state of Amazonas, Brazil. Lepr. rev. 1987; 58 (3):233-7.
25.Neder L, Weelden MV, Viola GR, Lourenço DM, Len CA, Silva CA. Qualidade de vida relacionada à saúde avaliada pelo inventario pediátrico de qualidade de vida 4.0 em pacientes pediátricos com hanseníase e manifestações musculoesqueléticas. Rev. bras. Reumatol. 2015; 55(5):414-9.
26.Lima MA, Prata MO, Moreira D. Perfil da hanseníase no Distrito Federal no período de 2000 a 2005. Com. ciênc. saúde. 2008; 19(2):163-70.
27.Ganemo A, Svenson A, Lindberg M, Wahlgren CF. Quality of life in Swedish children with eczema. Acta derm. venereol. 2007; 87:345 -9.
28.Dias NG. Avaliação comportamental de crianças com doenças crônicas de pele a partir de relatos de suas mães [dissertação de mestrado]. Londrina (PR): Universidade Estadual de Londrina; 2010.
29.Fontes Neto PTL, Weber MB, Fortes SD, Cestari TF, Escobar GF, Mazotti N, et al. Avaliação dos sintomas emocionais e comportamentais em crianças portadoras de dermatite atópica. Rev. Psiquiatr. Rio Gd Sul. 2005; 27(3):279-91.
30.Moura ADH, Albuquerque ERRO, Chaves ES, Souza AR, Lima GG, Chaves CS. Perfil dos portadores de hanseníase de um centro de referência de um estado brasileiro. Rev. enferm. UERJ. 2016; 24(6):e9625.
31.Ludwing MWB, Oliveira MS, Muller MC, Moraes JFD. Qualidade de vida e localização da lesão em pacientes dermatológicos. An. bras.dermatol. 2009; 84 (2):143-50.
32.Pinheiro MGC, Simpson CA. Preconceito, estigma e exclusão social: trajetória de familiares influenciada pelo tratamento asilar da hanseníase. Rev. enferm. UERJ. 2017; 25:e13332.