ORIGINAL RESEARCH
Sociodemographic and clinical characteristics of peripartum cardiomyopathy patients: contributions to nursing
Tamires Grama dos SantosI; Karla Biancha Silva de AndradeII; Flávia Giron CameriniIII; Andrezza Serpa FrancoIV; Ana Lúcia Cascardo MarinsV; Daniel Gomes de SousaVI
I
Nurse. Resident of the Cardiovascular Program at University Hospital
Universitário Pedro Ernesto. Rio de Janeiro, Brasil. E-mail: tamiresgrama@hotmail.com
II
Nurse. PhD. Assistant Professor of Faculty of Nursing at Universidade do
Estado do Rio de Janeiro. Brazil. E-mail: karla.biancha@gmail.com
III
Nurse PhD. Assistant Professor of Faculty of Nursing at Universidade do
Estado do Rio de Janeiro. Brazil. E-mail: fcamerini@gmail.com
IV
Nurse. Master's degree. Assistant Professor of Faculty of Nursing at
Universidade do Estado do Rio de Janeiro. Brazil. E-mail: dezza.franco@gmail.com
V
Nurse. Master's degree. Assistant Professor of Faculty of Nursing at
Universidade do Estado do Rio de Janeiro. Brazil. E-mail: cascardo.ana@gmail.com
VI
Nurse. Master's degree. University Hospital Pedro Ernesto. Rio de Janeiro,
Brazil. E-mail: danielg.sousa@gmail.com
DOI: https://doi.org/10.12957/reuerj.2018.32033
ABSTRACT
Objective: to identify the clinical and sociodemographic characteristics of patients with peripartum cardiomyopathy in a cardiac intensive care unit of a university hospital in Rio de Janeiro State. Method: this quantitative, cross-sectional, documentary analysis studied five medical records, between January 2014 and December 2016, according to pre-established inclusion and exclusion criteria, after approval by the research ethics committee. Data were collected using a specific form, tabulated in electronic spreadsheets, and analyzed by simple descriptive statistics. Results: subjects were aged predominantly 26-35 years (4; 80%), multiparous, skin color brown, admitted for caesarean section postoperative care (4; 80%), and for less than 2 weeks (4; 80%). The nursing problems encountered included decreased cardiac output and ineffective respiratory pattern. Conclusion: disclosure of this clientele's sociodemographic and clinical characteristics can help to delimit some representative nursing problems in this population.
Descriptors: dilated cardiomyopathy; critical care nursing; puerperium; patient care planning.
INTRODUCTION
Peripartum cardiomyopathy (PPCM) is a rare clinical condition of dilated cardiomyopathy, characterized by the development of systolic heart failure during the period between the last month of pregnancy and the first five post-partum months1. The estimated incidence varies from 1:1,300 to 1:15,000 pregnancies. In Brazil, the PPCM is responsible for 12% of hospital admissions of recent mothers. Mortality rates vary from 7 to 60%, and most deaths occur in the 3 months post-partum2.
Pregnancy produces changes in all the maternal body and their cardiovascular system undergoes progressive changes during pregnancy and childbirth, resulting in hemodynamic changes, characteristics of these periods. The main changes involved in this period are blood volume increase in around 30 to 50% and cardiac output, and systemic vascular resistance and vascular reactivity decrease3.
The etiology of the PPCM is uncertain, but the literature have proposed various causes, such as myocarditis, abnormal immune response to pregnancy, poor hemodynamic adaptive response to pregnancy (such as transient ventricular hypertrophy and cardiac remodeling) with excessive reduction of left ventricular function, cytokines activated by stress, viral infection, prolonged use of drugs to suppress premature labor, heredity, nutritional deficits (as selenium deficiency), hormonal disorders and use of narcotic drugs, such as cocaine4.
According to the National Heart, Lung and Blood Institute, there are four criteria to define PPCM. In addition to defining criteria, the main signs and symptoms for these patients are dyspnea, orthopnea, paroxysmal nocturnal dyspnea, fatigue, night cough, abdominal pain, palpitation, precordial pain, anorexia, asthenia and hemoptysis. Some of the symptoms mentioned are also normally present during pregnancy, which may delay the diagnosis of PPCM1,2,4.
The literature highlights also some risk factors, such as maternal age over 35 years, multiparity (more than three births), afrodescendence, preeclampsia/eclampsia, twin pregnancy, obesity, high blood pressure (BP) and long-term therapy (> 4 weeks) with b-adrenergic agonists 2,4-6.
Among the diseases that cause high-risk pregnancy, heart diseases are the ones that lead to maternal death. Faced with so many hemodynamic changes is expected to find some emotional instability in these pacientes7
Despite the undeniable understanding that nursing needs to appropriate specific and peculiar care to take care of peripartum cardiomyopathy patients, we still observe a shortage of national and international publications addressing this theme, including socio-demographic and clinic characteristics2,4,5-7.
Furthermore, there is little information on the subject, focused on nursing and care for the patient with PPCM, which must intend to minimize the discomfort caused by the pathology and stabilize the hemodynamic framework.
In this respect, meeting sociodemographic and clinics characteristics of women with PPCM can help nursing to draw up a plan care for these patients focused on controlling the signs and symptoms and improving comfort, as well as, the knowledge about the disease.
In this way, we believe that this study could contribute guide specific nursing care for this clientele. Thus, we formulated the following research question: what are the sociodemographic and clinical characteristics of PPCM patients in a cardio intensive unit?
And, to answer the question, this research aimed to identify the clinical and sociodemographic characteristics of patients with peripartum cardiomyopathy in a cardio intensive unit of a university hospital in the state of Rio de Janeiro.
We believed that knowing the characteristics could help the nurse who works in cardiovascular nursing, to direct care that can contemplate a quality assistance and contribute to the good practices with this specific population.
LITERATURE REVIEW
The relationship between the development of heart failure (HF) and pregnancy was initially described in 1870, when the process of myocardial degeneration was identified in patients who died in the postpartum period, by a heart failure. This heart failure is interpreted as a dilated heart disease different from that generated by the stress of pregnancy5.
PPCM is a rare pathology, but associated with high maternal mortality rate, that may vary from 2% to 56%, and with the highest incidence of premature and cesarean childbirth, probably associated with gestational hypertension and multifetal gestation. The most frequent period of appearance is in the first days after childbirth. The causes that lead to death are heart failure, arrhythmias and/or embolic events5.
Its etiology is still unknown, however, it was described as the association of changes in the processing of prolactin, angiogenic imbalance and other inflammatory and even immunological processes. Its symptoms resemble heart failure due to left ventricular insufficiency, which may be unnoticed when interpreted as frequent symptoms during pregnancy, as well as transient ischemic brain frames and it rarely presents thromboembolic complications. It is possible to recover a normal operation with appropriate diagnosis and treatment5,6,8.
The European Society of Cardiology defined it, in 2010, as the disease that develops heart failure at the end of the pregnancy or in the months after childbirth, in the absence of another identifiable cause for it, in addition to systolic dysfunction of the left ventricle with fraction of ejection, on most occasions, less than 45%, with a possible dilated left ventricle9.
This definition was extended to include women who had the same symptoms in early stages of pregnancy, although most cases were observed in the last month of pregnancy and 5 months puerperium and also emphasized that it is an exclusion diagnosis9,10.
The directive of the Brazilian Society of Cardiology for pregnancy in the woman with heart disease, describes a study that proves that the disease can manifest with HF at an early gestational age than the last month of gestation, and may appear since the 17th week of gestational age 5.
The prognosis is based on the size of the left ventricular dysfunction within six months postpartum, and some studies have demonstrated that the left ventricular dysfunction becomes persistent in 50% of cases, resulting in a mortality of 85% in 5 years4,8.
About the high mortality rate, the highest risk of death is associated with factors such as: Advanced maternal age (> or = 30 years); Higher parity (3rd gestation or more); Late onset of symptoms following pregnancy; Larger left ventricular final diastolic dimension (> or = 7.0 cm); Higher average pulmonary blood pressure (> or = 38 mmHg) and capillary pulmonary blood pressure (> or = 24mmHg); and driving disorders in the electrocardiogram4,5.
METHODOLOGY
Quantitative transversal study, which carried out documentary analysis of the patient's records10 in a cardio intensive unit of a university hospital located in the municipality of Rio de Janeiro, from January 2014 to December 2016.
The criteria for the inclusion of the medical records were: patient records with the diagnosis of peripartum cardiomyopathy, admission in the cardio intensive unit and older than 18 years old and less than 50 years old.
Exclusion criteria were incomplete or unavailable records during the data collection period.
The data were collected through a document analysis sheet, containing 15 variables focused on the sociodemographic and clinical characteristics, that are: Age; Schooling, Marital status; Color, Place of birth; Number of children; Types of childbirth; Comorbidities Period of identification of the pathology; Signs and symptoms; causes for HF; Changes in echocardiogram; Period of hospitalization; Relocation and closure and five variables directed to pharmacological description: medication, presentation, period of use, report of adverse reaction; Type of access.
We collected data through searching in the patients' movement book and requested to the file sector.
We listed 50 patients' records and after applying the inclusion and exclusion criteria, we selected five medical records to participate in the study.
After this step, the data was tabulated in electronic spreadsheets and analyzed through simple descriptive statistics, using the Microsoft Excel ® program, which made it possible to build a database and create a table and figure to show the results of this research.
The present study was inserted on the Brazil platform for the evaluation of the Committee of Ethics in Research of the proposing and co-participant institutions (CAEE: 66729517.6.0000.5229), and no authorization was requested to collect the data by means of the term free and informed consent, as the data collection took place in a documental manner.
RESULTS AND DISCUSSION
PPCM is an infrequent pathology of heart failure with still uncertain etiology11. During the allotted time cut for data collection, we found five patients carrying this pathology. All patients researched were diagnosed with PPCM during pregnancy and all gave birth premature babies (7 months).
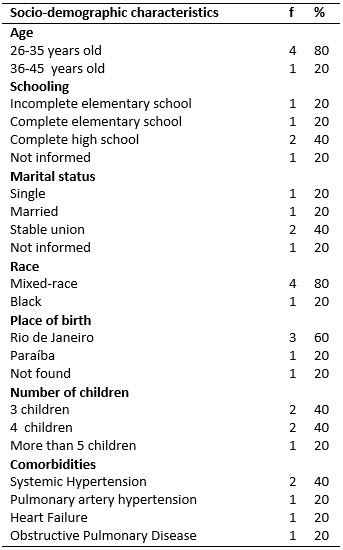
In the sample studied, the most frequent sociodemographic characteristics in patients were maternal age older than or equal to 30 years old - 4 (80%); mixed raced - 4 (80%) and black - 1 (20%); number of children greater than or equal to 3 (100%); and arterial hypertension - 2 (40%).
TABLE 1:
Demographic and clinical data of patients with PPCM admitted on Cardio
intensive Unit, Rio de Janeiro, 2017.
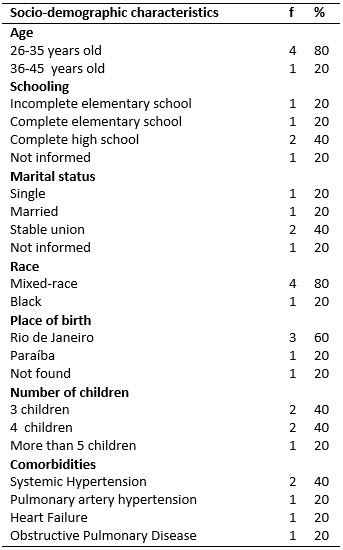
These characteristics are in accordance with those found in the literature, which describes as possible risk factors for the clinical manifestation of PPCM-the advanced maternal age, higher parity (3rd gestation or more), late emergence of symptoms after pregnancy, Afro-descendants, preeclampsia/eclampsia, twin gestation; Obesity and high blood pressure (BP)2.
In the United States of America, there are also prevalence of cases in afro-descendants. The estimated incidence of variation is between 1:1.149 and 1:1,400 born alive, while in South Africa is 1:1,100 and in Haiti 1:2.99411.
This study identified that all patients with PPCM had three or more children, classified as multiparous with the pathology discovered in the first gestation. This data shows how nursing can contribute, informing about the disease and guiding on family planning, important for these patients and their families.
Family planning is fundamental, because patients who have normalized ventricular function can get pregnant again and safely, but have a high chance of presenting recurrence of the disease in subsequent gestation. There are also those who have not recovered ventricular function and have high probability to suffer new heart decompensation and death, because the regression of ventricular dysfunction occurs in 50% of patients, while 25% can evolve to death within three months due to HF, arrhythmias or thromboembolism, the rest b remains with CMPP1,12-14.
Systemic arterial hypertension, was a risk factor that prevailed in 2 (40%) of the patients studied and to control it, it was necessary to use the measure of the invasive BP, characterizing the severity of this comorbidity, becoming indispensable to Nursing to act in the prevention and control of pressure levels. It is a complex, multifactor disease, which can be of genetic, environmental and psychosocial origin that affects thousands of women at fertile age15-17.
Patients diagnosed with PPCM are high-risk pregnant women and accompanied by the cardiologist in prenatal care. Hemodynamic changes presented during prenatal consultations may lead to the adjustment of pharmacological treatment and definition of the time when gestation should finish. Generally, this decision occurs when the clinical picture becomes more severe and signs and symptoms caused by PPCM worsen8.
The reason for the hospitalization in the Cardio intensive Unit, 2 (40%) were cesarean birth post-surgery, 2 (40%) cesarean and tubal sterilization post-surgery and 1 (20%) clinical treatment. A patient had to stop her pregnancy due to the clinical picture presented at the time of hospitalization.
These findings agree with literature that refers that cesarean birth is more likely to develop complications, whether in the trans-operative or in the post-surgery period, and it is often necessary to transfer these patients to Intensive care units for further surveillance and monitoring12.
The presentation of the signs and symptoms observed in the systolic HF are dyspnea, nocturnal paroxysmal dyspnea, persistent cough, dry cough, orthopnea, tachycardia, secondary abdominal discomfort to visceral congestion, precordialgia, palpitation, hemoptysis, peripheral edemas, ascites, hepatomegaly, cardiomegaly and jugular engorgement1,4,5,13.
As PPCM is a HF generated by gestation, its signs and symptoms are similar to those found in the other patients with HF.12 In this study, the signs and symptoms found in patients with PPCM, at the time of hospitalization, were dyspnea-3 (60%) , paroxysmal nocturnal dyspnea – 1 (20%), orthopnea – 2 (40%), lower limb edema – 2 (40%), high blood pressure – 2 (40%), nausea/vomiting – 2 (40%) and fatigue – 2 (40%).
The time of hospitalization of patients with CMPP in Cardio intensive unit was less than 2 weeks in 4 (80%) of the participants medical records. According to the National Supplemental Health Agency, in 2013, the average time of hospitalization in the adult intensive care unit varied from 4.5 to 5.3 days, according to age, diagnosis, comorbidities and complexities 15.
Only 2 (40%) patients were readmitted, 2 (40%) were discharged and 3 (60%) were transferred to another unit.
These findings point out that, despite the severity of the disease itself, these patients did not die. Perhaps this is due to the age of the women who participated in this study, not very advanced. Younger people have their defense mechanism much more strengthened, making them to recover faster 16.
About the administration of prescribed venous medications, 3 (60%) used peripheral venous access and 2 (40%) deep venous access. With respect to invasive devices, 2 (40%) patients had an invasive BP for their rigorous control and 2 (40%) vesical catheter of delay to quantify the diuresis.
The medicines most used during the period of hospitalization of these patients with PPCM were analgesics, benzodiazepines and antihypertensive, used by 4 (80%) of the patients studied.
Pharmacological treatment is similar to the standard treatment of HF, respecting gestation and lactation, and taking into account the potential adverse effects for mother, fetus or neonate. Water restriction is monitored through daily weight control in patients with volume overload and arterial pressure regulating medications6,8,18.
Nursing care to this clientele must be based on the identification of the problems. In this sense, the demographic and clinical characterization of these patients can help to make the assistance safer and minimize the signs and symptoms presented.
Thus, according to the findings of this study, some problems of nursing are suggested, according to Nursing Diagnosis (NANDA 2015-2017)19. Among the various possible nursing diagnoses, we listed seven problems and their respective justifications.
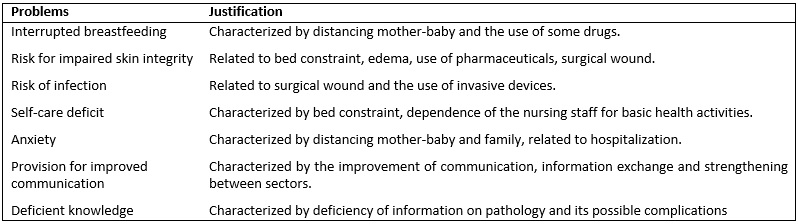
FIGURE 1:
Nursing problems identified from the sociodemographic and clinic
characterization of patients with PPCM. Rio de Janeiro, 2017.
Interrupted breastfeeding and anxiety were the main problems identified in the studied sample, because, due to the pathology, the hospitalization in the intensive therapy and the use of some drugs, the baby is removed from the mother and she is unable to breastfeed them.
Using nursing prognosis classifications, through NANDA, makes it possible to highlight the actions of the profession and the science in the process of care20. Cardiac patients have their specifics with their respective nursing diagnoses, as well as patients with PPCM, who besides being cardiac, they may be pregnant or mothers according to the phase the pathology manifests. Due to this peculiarity, some of the diagnoses identified in this study were described in Figure 1.
The nurse must know the most frequent diagnoses used in these patients, so that interventions can be implemented actively, assisting in the planning and operation of a care plan that contemplates all the Needs of this clientele in order to collaborate with their rehabilitation21.
We expect this research can contribute to minimize the gaps of knowledge on this subject, still little discussed by Brazilian nursing, and direct some nursing problems according to the identification of sociodemographic and clinic characteristic.
CONCLUSION
PPCM is a rare and more prevalent pathology in women with a history of multiple pregnancies, hypertension and age between 25 and 35 years old.
This research has some limitations, such as the reduced number of patients diagnosed with PPCM and the weaknesses of the documentary studies. More research using other methodologies and involving more than one center, in order to capture a larger number of participants, are necessary to fill the gaps left by this study.
The purpose of this research was achieved and disseminating the sociodemographic and clinical characteristics of these patients can help to delimit some representative nursing problems regarding this clientele. In the future, it may be possible to take specific care with this population, which should bring comfort and well-being, prevention of complications and guidelines for the knowledge of the disease.
We expect the results of this research may be used by nursing professionals who assist patients with PPCM and can contribute to disseminating knowledge on this subject still little explored by nursing, stimulating new research.
REFERENCES
1.Resende BAM, Jorge CS, Mello DC, Scala FD, Senra JC, Cortes JRG, et al. Peripartum Cardiomyopathy. Rev. Med. Minas Gerais. 2009; 19(3):16-20. Available from: www.rmmg.org/exportar-pdf/1094/v19n4s3a04.pdf
2.Urbanetz AA, Kalache PF, Carraro EA, Kalache LF, Lobo PHF, Germiniani H, et al. Peripartum Cardiomyopathy. FEMINA. 2009;37(1): 13-8.
3.Picon JD, Ayala AMPO. Hemodynamic changes in pregnancy. Revista da Sociedade de Cardiologia do Rio Grande do Sul. 2005 [cited 2017 Dec 10]; 14(5). Available from: http://sociedades.cardiol.br/sbc-rs/revista/2005/05/Artigo01.pdf
4.Rombaldi A, Galvão A, Kissner F, Vianna C, Tesser L. Peripartum Cardiomyopathy. Revista da Sociedade de Cardiologia do Rio Grande do Sul.2005 [cited 2017 Dec 10]; 14(5). Available from: http://sociedades.cardiol.br/sbc-rs/revista/2005/05/Artigo10.pdf
5. Brazilian Society of Cardiology directive for pregnancy in the woman with heart disease. Peripartum Cardiomyopathies. Arq. Bras. Cardiol. 2009 [cited 2017 Dec 10]; 93(1):110-78. Available from http://publicacoes.cardiol.br/consenso/2009/diretriz_card_grav_9306supl1.pdf
6.Santos VM, Araujo MCM, Albuquerque RB, Pereira VSC, Mussi P, Carvalho MRM. Peripartum Cardiomyopathy: a favorable clinical result. Rev. Med. Saúde. 2014; 3(1). Available from: https://portalrevistas.ucb.br/index.php/rmsbr/article/view/4812/3135
7.Furlan FLP, Benute GRG, Nomura RY, Fráguas R, Lucia MCS, Zugaib M. Depression in cardiac pregnant women and their influence on the maternal-fetal bond. Hospital Psychology. 2010 [cited 2017 Dec 10]; 8(1):39-60. Available from: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1677-74092010000100004
8.Carvalho MLR. Peripartum Cardiomyopathy. [Master's Dissertation – Bibliographical review article]. Porto: Universidade do Porto; 2016. [cited 2017 Dec 10]. Available from: https://sigarra.up.pt/fcnaup/pt/pub_geral.show_file?pi_gdoc_id=887320
9.Sarraulte GV, Sandoval LV. Peripartum Cardiomyopathy. Med. leg. Costa Rica. 2017 [cited 2017 Dec 10]; 34(1): 287-95. Available from: http://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S1409-00152017000100287
10.Polit DF, Beck CT. Fundamentals of Research in Nursing: evaluation of evidence for the practice of nursing. 7th ed. Porto Alegre (RS): Ed. Artmed; 2011.
11.Silva MVP, Andrade BCP, Aguiar FP, Nogueira VD, Paula LL. Peripartum Cardiomyopathy – case report. 2017 [cited 2017 Dec 10]; 20 (1): 72-5. Available from: http://www.mastereditora.com.br/bjscr
12.Santos JDO, Pacheco TS, Oliveira PSD, Hino P, Gabrielloni MC, Barbier M. Evaluation of pain in the puerperal period: comparative study of the types of childbirth. J. Health Sci. Inst. 2016 [cited 2017 Dec 10]; 34(4):200-5. Available from: https://www.unip.br/comunicacao/publicacoes/ics/edicoes/2016/04_out-dez/V34_n4_2016_p200a205.pdf
13.Oliveira FTM, Oliveira GCR, Meira MLG, Mendes MM, Amaral MSG, Costa PR SM, et al. Peripartum Cardiomyopathy. Rev. Med. Minas Gerais. 2012 [cited 2017 Dec 10]; 22 (5):25-7. Available from: www.rmmg.org/exportar-pdf/675/v22s5a07.pdf
14.Ardila DFP, Hurtado SN, Osorio EMA, Rosero RAA. Peripartum Cardiomyopathy Heart failure. 2009 [cited 2017 Dec 10]; 4(4):177-83. Available from: http://www.scielo.org.ar/pdf/ic/v4n4/v4n4a06.pdf
15. Ministry of Health (BR). National Agency for Supplementary Health. Average permanence adult ICU. ANS. 2013 [cited 2017 Dec 10]; 1(1). Available from: http://www.ans.gov.br/images/stories/prestadores/E-EFI-07.pdf
16.Aldrighi JD, Wall ML, Souza SRRK, Cancela FZV. The experiences of women in advanced maternal age gestation: Integrative revision. Rev. Esc. Enferm. USP. 2016 [cited 2017 Dec 10]; 50(3). São Paulo (SP). Available from: http://www.scielo.br/pdf/reeusp/v50n3/pt_0080-6234-reeusp-50-03-0512.pdf
17.Berardinelli LMM, Figueiredo TDFLD, Oliveira SAD, Santos ID, Giron MN, Ramos JP. High blood pressure and popular knowledge: enhancing care. Rev. enferm. UERJ. 2013; 21(4), 446-51. Available from: http://www.facenf.uerj.br/v21n4/v21n4a05.pdf
18.Resende BAM, Jorge AS, Mello DC, Scala FD, Senra JC, Cortes JRG, et al. Miocardiopatia periparto: aspectos relevantes. Red. Med. Minas Gerais. 2009 [cited 2017 Dec 10]; 19(3):75-8. Available from: www.rmmg.org/exportar-pdf/1107/v19n4s3a17.pdf
19.Herdman TH, Kamitsuru S. North American Nursing Diagnosis Association- NANDA. Nursing Diagnostics of NANDA 2015-2017. Translation by Regina Machado Garcez. 10ª ed. Porto Alegre (RS): Artmed; 2015.
20.Lopes CT, Carneiro CS, Santos VB, Barros ALBL. Nursing diagnoses validated in cardiology in Brazil: Integrative literature Review. Acta Paul. Enferm. 2012 [cited 2017 Dec 10]; 25(1):155-60. Available from: www.redalyc.org/htm/3070/307026828024
21.Oliveira ARS, Costa AGS, Moreira RP, Cavalcante TF, Araujo TL. Nursing diagnoses validated in cardiology in Brazil: Integrative literature Review. Rev. enferm UERJ. 2012 [cited 2017 Dec 10]; 20(2): 221-8. Available from: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/4066/2859