
Figure 1: Flowchart for the selection of studies for the integrative review. Rio de Janeiro, 2017.
REVIEW ARTICLE
Instruments for assessing sleep patterns in children with chronic diseases: an integrative review
Rosilene Silva de AndradeI; Ravini dos Santos Fernandes Vieira dos SantosII; Antônio Eduardo Vieira dos SantosIII; Neize Lúcia de AndradeIV; Isabela Fornerolli de MacedoV; Michelle Darezzo Rodrigues NunesVI
I
Nurse. Resident in Pediatric Nursing at Universidade do Estado do Rio de
Janeiro. Brazil. E-mail:
rosilene.andrad@hotmail.com
II
Nurse. MS. Assistant Professor, Nursing College, Universidade do Estado do
Rio de Janeiro. Brazil. E-mail: ravini_uerj@hotmail.com
III
Nurse. PhD. Adjunct Professor, Universidade do Estado do Rio de Janeiro.
Brazil. E-mail: antonio.santos@iff.fiocruz.br; antonioeduardo@uerj.br
IV
Nurse at Pedro Ernesto University Hospital, Specialist in Pediatric
Nursing. Brazil. E-mail: neizelucia@gmail.com
V
Nurse. MS. Assistant Professor, Nursing College, Universidade do Estado do
Rio de Janeiro. Brazil. E-mail: belafornerolli@gmail.com
VI
Nurse. PhD. Adjunct Professor, Nursing College, Universidade do Estado do
Rio de Janeiro. Brazil. E-mail: mid13@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.31924
ABSTRACT
Objective: to examine Brazilian and international scientific production on the use of sleep pattern assessment instruments in children with chronic diseases. Method: this integrative review was conducted on the PubMed, Web of Science, CINHAL, LILACS, and SciELO databases for 2006 to 2016. Results: 16 articles were selected for review, and several reliable sleep assessment instruments were found. However, none was adapted to Brazilian Portuguese, except for polysomnography and actigraphy. Children with chronic diseases have sleep disorders that correlate with pain, fatigue, behavior problems, lack of physical activity, and obesity. Conclusion: in Brazil, specific sleep assessment instruments are little used with children. Use of these instruments in clinical practice could help nurses to outline strategies to reduce sleep disorders among children and adolescents.
Descriptors: Sleep; child; adolescent; scale;pediatric nursing.
INTRODUCTION
Chronic diseases account for 60% of all disease burden in the world, and this is estimated to reach 80% by 2020. In Brazil, the prevalence of chronic diseases among children from 0 to 14 years old is 9.3%.1
The main characteristics of the chronic health condition are the permanent character, the residual incapacity, the long duration, the drug dependence, the recurrent character and the fact that it is almost always incurable, irreversible and degenerative,2 predisposing to compromising the sleep pattern in the child.
Frequent interruptions of sleep and rest in children interfere in the processes of growth, development, learning and health.3,4 In addition to preventing homeostatic and repairing function, changes in sleep pattern can lead to cardiovascular, metabolic-endocrine, immunological, psychological consequences, increased daytime sleepiness, decreased quality of life.5
The total sleep time varies with each age group and decreases gradually over the years, varying in average 12 hours in the newborn and up to 7 to 8 hours in the schoolchildren and adolescents.3,6 In hospitalized children, there was a significant decrease in sleep efficiency (on average 3.4 hours) mainly due to the various nocturnal awakenings and daytime naps.4,7-9
Any care that prioritizes the maintenance of sleep and rest will favor healing, since it will create conducive conditions for the body to fight the disease, preventing its exacerbation and triggering of new disorders. 6 Nursing can plan and act effectively on reducing sleep disorders in children with chronic diseases and who are hospitalized using instruments to measure the sleep pattern.
The objective of this study was to analyze the national and international scientific production related to the instruments used to evaluate the sleep pattern in children with chronic diseases.
METHODOLOGY
This is an integrative review carried out in the following stages: formulation of the problem; search procedures; evaluation of data; data analysis; and interpretation and presentation of the review. 10,11 The guiding question was: What are the instruments used to assess the sleep pattern in children with chronic disease?
To answer this question, the databases searched were: PUBMED; Web of Science and CINHAL; LILACS and SciELO. The following descriptors were used in Health Science (DeCS) andMedical Subject Headings (MESH): sono (sleep), criança ( children), adolescente (teen), escala (scale); and the following keywords: padrão de sono (sleep pattern), instrumento (instrument), dispositivo (device) — both descriptors and keywords were used in different combinations.
Original articles, published between 2006 and 2016, were included in English or Portuguese. Review articles and dissertations/theses were excluded.
The data were organized into two categories related to the exploitation of their contents. Initially, 303 articles were found. After an exhaustive reading of the abstracts, all duplicated materials were excluded, as well as those that did not belong to the subject matter of the study. Thus, there were 16 articles12-27 for further analysis. The flowchart of the selection of studies for the integrative review is shown in Figure 1.

Figure 1:
Flowchart for the selection of studies for the integrative review. Rio de
Janeiro, 2017.
RESULTS
Most of the studies were published in the United States (68.7%), and the publication period varied between 2006 and 2016, with a higher concentration (68.7%) in 2014 (37.5%), 2015 (18.7%) and 2016 (12.5%). Regarding the type of periodical, 6 (37.5%) were published in scientific journals not belonging to the nursing area, of which 4 (25%) were published in specialized journals dealing with mental disorders; 2 (12.5%) were published in pediatric specialty journals. The other 10 (62.5%) articles were published in nursing journals, of which 6 (37.5%) were published in nursing journals in pediatric oncology; 3 (18.7%) in pediatric nursing journals; and 1 (6.2%) in a periodical of basic research in nursing.
The analysis of the 16 selected studies12-27 allowed for the quantitative synthesis creation which showed, besides the instruments that evaluate sleep, other used to relate other symptoms, such as pain, fatigue, anxiety, depression, stress, behavior, feeding, parental satisfaction and environmental factors. The instruments used to evaluate sleep – questionnaires and scales – found in the selected studies and their respective description are described in Figure 2.
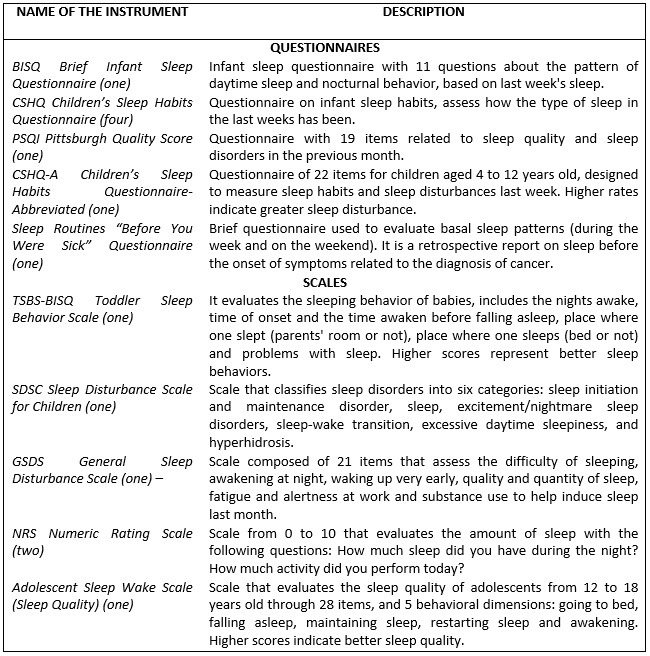
Figure 2:
Description of instruments that evaluate sleep: questionnaires and scales.
Rio de Janeiro, 2017.
The instruments that evaluate sleep – diaries and devices – are presented in Figure 3.
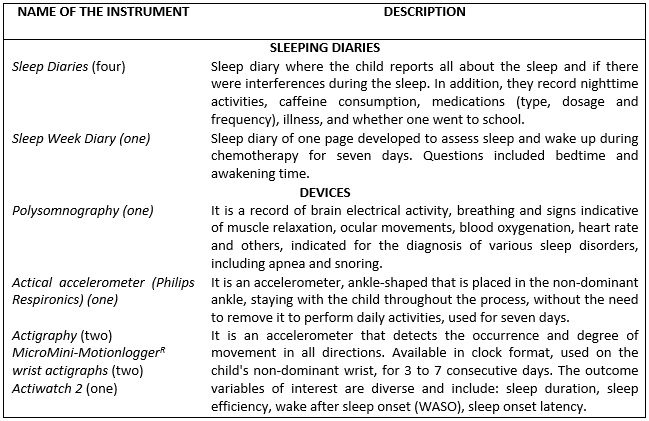
Figure 3:
Description of instruments that evaluate sleep: diaries and devices. Rio de
Janeiro, 2017.
The 16 selected studies were grouped into two categories, which are analyzed below.12-27
Category 1: Sleep evaluation in children with chronic diseases
Four studies compose this category, which exclusively evaluates sleep in children with chronic diseases.
The first study evaluated sleep in 51 adolescents (10-19 years old) diagnosed with cancer. The instruments used were answered by adolescents. The results revealed a worsening in the sleep quality and hygiene of adolescents under chemotherapy treatment.12
The second study analyzed sleep in 107 hospitalized children (1-18 years). Parents completed the diary for children under 12; after that age, the child/adolescent himself/herself responded to the instrument. The study presented a mean of 9.8 hours of sleep, ranging from 5 to 16 hours. Children aged 2 and 5 years were the most affected, 52.3% of the children had poor sleep, 49.5% had a sleep efficiency of less than 90% and 34.5% had awaken three or more times. The highest prevalence of poor sleep occurred in children with chronic conditions (61.9%). Sleep awakening was related to nursing care, alarms and pain.13
The third study analyzed sleep in 95 children and adolescents (3-17 years old) diagnosed with neurofibromatosis. The instrument for sleep evaluation was performed by the parents. The study indicated that these children are slow to start sleeping, showing sleep disturbance, sleep-wake transition, and daytime sleepiness.14
The fourth study evaluated the effect of a sleep intervention in 22 children (5-15 years) with a diagnosis of autism/intellectual disability. The intervention used was a training of the parents regarding the behavioral approach of the child. The instruments used to evaluate sleep were performed by the parents. The study revealed that the child's sleep was improved compared to the pre-intervention period. A decrease in nocturnal awakenings and an improvement in sleep resistance were shown. 15
The results of the studies analyzed agree that children and adolescents with chronic conditions present an impaired sleep. The treatment performed, the hospitalization, the presence of symptoms related to the disease and the interruptions of the sleep generated by the environment and care of the Nursing team are among the several related factors.
Category 2: Evaluation of sleep and its correlation with other symptoms
From this category, four subcategories emerged, encompassing 12 studies. 16-27 They address sleep and symptoms like pain, fatigue, behavioral problems and relate them to the sleep of children with chronic diseases. This category was divided into four subcategories according to the symptoms studied.
Subcategory 1: Sleep disturbances and behavioral problems
This subcategory is composed of three studies on sleep and behavioral problems in children with chronic disease.16-18
The first stud16 compared sleep quality and behavioral problems in 102 children (6-12 years) with a diagnosis of asthma. The instrument used was polysomnography performed in children; and the Child Behavior Checklist (CBCL), answered by children and parents. The study reports that children with asthma take longer to fall asleep and present greater movement in the legs during sleep, as well as greater REM sleep and a lower proportion of slow-wave sleep, presenting a higher respiratory excitation index.16
The second study also compares sleep disorders and behavioral problems (anxiety, depression, mood adjustment difficulties) in 116 patients (6-11 years old) with a diagnosis of juvenile idiopathic arthritis. The sleep instrument used was reported by parents. The Child Behavior Checklist (CBCL) and the Scale Pain were used, both reported by parents. The study showed that children with juvenile idiopathic arthritis have the following sleep disorders: sleep resistance, delayed onset of sleep, changes in sleep duration, anxiety, nocturnal arousals, parasomnias, disordered breathing and daytime sleepiness.17
The third study evaluated the sleep of the mother and the child (3-12 years) in 26 participants with diagnosis of acute lymphoblastic leukemia (ALL). The instruments used were: Actiwatch 2,Daily Sleep e Children's Sleep Habits Questionnaire-Abbreviated (CSHQ-A). Other instruments were used to assess anxiety and depression. The study shows that mothers and children with ALL have sleep disorders; Children with ALL take longer to fall asleep and have had variations in sleep patterns. It was identified a correlation between the mother's insomnia, stress, depression and anxiety.18
Children with chronic diseases present sleep disorders that may contribute to the development of behavioral problems in the child and in the mother.
Subcategory 2: Sleep and fatigue
The first study analyzed sleep and fatigue in 29 participants (7-18 years old) with a diagnosis of cancer. Instruments that evaluate sleep were used in children; and the Daily Sleep was answered by parents. The instruments that evaluate fatigue were answered by the children, except the Fatigue Scale-parent (FS-P), which was answered by the parents. The study reports that 70% of children slept 1 to 2 hours without waking, 22% slept 2 hours/night and 7% of children slept 4 hours of uninterrupted sleep. The number of nocturnal awakening is related to fatigue during hospitalization, and data from the Actigraph showed that there is sleep disturbance.19
The second study evaluated sleep and fatigue in 77 children and adolescents (4-18 years old) diagnosed with acute lymphoblastic leukemia. The instrument used to evaluate sleep was the Children's Sleep Habits Questionnarie (CSHQ). Children under 13 years old had parental help filling out the questionnaire, and those over the age of 13 completed it alone. In addition to the sleep instrument, instruments that evaluate fatigue and the General Sleep Disturbance Scale (GSDS) were used, which were filled by the parents. The study shows that children undergoing chemotherapy sleep less than recommended, present disturbances in sleep; children aged 8 to 12 report fatigue; and fatigue and sleep disorders were significantly correlated.20
The third study evaluated sleep and fatigue in 35 children and adolescents (8-17 years old) diagnosed with cancer. Participants were recruited at the hospital and used the instruments at home. The Actigraph and the PedsQL Multidimensional Scale of Tiredness were used. The study showed that children and adolescents with cancer have problems with sleep and fatigue even at home. It also revealed that the adolescents slept less than the children and stayed more hours awake after the onset of sleep. Children and adolescents who had less sleep duration were also those who had more problems with fatigue.21
Subcategory 3: Sleep and pain
The first study analyzed sleep and pain in 27 children (5-19 years old) with a diagnosis of sickle cell anemia. The study showed that 50% of pain episodes occur on the first day of hospitalization and that more than 50% of children report interruptions in nocturnal sleep, while 20% of them report sleeping during the day.22
The second study analyzed sleep and pain in 49 children (8-17 years old) with cancer and showed that 22.4% of children had mild pain, 20.4% moderate pain and 12.2% severe pain. The highest pain rating occurred on the first day of hospitalization. There was no significant difference in sleep in relation to pain, but pain interfered with sleep.23
The third study evaluated sleep, pain and environmental interference in 15 school-aged children diagnosed with cancer. TheWong-Baker FACES scale or numerical scale and HOBOr U12-012 were used. The study showed that school-aged children did not have a complete sleep cycle. The nocturnal sound levels, light intensity and temperature exceeded the recommended level, interfering with healthy sleep.24
The fourth study of this category evaluated sleep and pain in 66 children (10-17 years old) with a diagnosis of sickle cell anemia. ThePittsburgh Sleep Quality Index (PSQI), the Visual analog scale and the Pediatric Pain Coping Questionnaire (PCQ) were used. The study found that two-thirds of children reported pain, most (91.2%) had mild to severe sleep disturbance, and about 18.2% used sleep medications three or more times a week.25
Subcategory 4: Other sleep correlations
This subcategory is composed of two studies that found correlations of the sleep pattern different from previous studies.
The first one evaluates at the same time sleep, fatigue and pain in 40 children (8-14 years old) with diagnosis of juvenile idiopathic arthritis. It was concluded that 68% of the children with juvenile idiopathic arthritis have a disturbed sleep, the younger children (8-11 years old) slept more and earlier than the older children (12-14 years old). 26
The second sought association between sleep and obesity in 304 children (12-32 months old) born to term with more than 2,500 grams. The study revealed that the duration of nocturnal sleep varied according to race, socioeconomic situation and activity. White babies, with socioeconomic status above the poverty threshold and who had more physical activity, had a longer duration of sleep. There was also an association between obesity and shorter sleep duration, with less weight-bearing children sleeping 0.7 more hours/night compared to obese children.27 It has been observed that pain and fatigue alter sleep and that some factors, such as age and excess weight, can negatively influence children's sleep patterns.
DISCUSSION
The results found several instruments used to evaluate the sleep pattern in children with chronic diseases: five questionnaires, five scales, two sleep diaries and three devices. Almost all articles mentioned the validity and reliability of the instrument chosen for the study, but none of them were translated, adapted and validated into Portuguese, except for polysomnography devices and actigraphy. For them to be used scientifically, these instruments must be valid and reliable, and it is necessary to go through all the processes that guarantee their feasibility. 28,29
The results indicated that children in chronic situations present sleep disorders, such as worsening sleep quality and hygiene and delayed sleep. When hospitalized, they sleep less because of their own illness, symptoms, treatment, noise, and care of the nursing staff. Studies with neonates and children with chronic diseases have shown similar results: a review on neonates' sleep in an intensive care unit states that the hospital environment can be a facilitator of interrupted sleep due to the technology available, low temperature, brightness and noise;30 while another study, with 11 children (2-12 years old) hospitalized with cancer, showed that they had difficulty falling asleep, worse quality of sleep and difficulty falling asleep after discharge.8
Analysis of the studies selected in this research also revealed that sleep disorders may be related to other symptoms, such as behavioral problems, pain and fatigue. A Norwegian study with children (11-13 years old) presenting chronic disease showed that they had higher levels of emotional and behavioral disorders.31 Another study, with 83 mothers and children (2-5 years old), showed emotional reactivity, anxiety/depression, somatic complaints, withdrawal/depression, attention problems and aggressive behavior in children with sleep problems compared to those who did not have sleep problems, emphasizing that problems of sleep or insufficient sleep exacerbate the emotional and behavioral difficulties. 32 Research findings with children with cancer showed that they had more problems with sleep, depression, anxiety and chronic fatigue. 33
On sleep and fatigue, this review showed a correlation between both symptoms and with pain. Children with shorter sleep duration had more problems with fatigue and pain. A case-control study with 167 cancer subjects and 170 healthy subjects revealed that sleep and fatigue disorders were related to psychological distress and could trigger depression. 34
Regarding the correlation between sleep and pain, the results showed that the higher the pain symptoms, the greater the difficulties related to sleep and the lower the number of hours the child sleeps. A study with 112 adult rheumatoid arthritis patients reports that less than 80% of patients had poor sleep quality, and this is related to sleep apnea and depression, as well as joint pain that is correlated with sleep disorders, interfering in the quality of sleep and life of these patients.35 In a study with 89 women diagnosed with fibromyalgia: 76% presented unrepairable sleep, did not obtain a good quality of sleep (intensifying pain and fatigue) and manifested psychic problems many times, such as anxiety and depression.36
It has also been identified that obesity may be related to sleep disorders. Obese children sleep less than healthy children, and physical activity can help them sleep better. In a study with 4,231 healthy children (1-4 years old), those who slept for less than 10 hours/night were very likely to be overweight or obese at 4 years of age.37 Research on physical fitness with 200 schoolchildren revealed that those who slept less than 9 hours/day also had higher rate of body mass index. In addition, the best performance regarding physical fitness was for the group of schoolchildren who slept more than 9 hours/day.38
CONCLUSION
This study reviewed 16 scientific papers published between 2006 and 2016 and related to sleep disorders in children with chronic diseases. Most of this production was made in the US during the last four years of the period.
Most of the instruments used to verify sleep are only valid and reliable for the foreign language, demonstrating an important gap in Brazil, where only the polysomnography and the actigraphy have been used in previous studies.
It has been observed that chronic disease interferes negatively in sleep, which alterations can lead to other problems, such as pain, fatigue, anxiety and weight gain.
It is hoped that this study makes the nursing team aware of the relevance of improving the daily sleep quality of the child. This is an extremely important subject for children's quality of life and little explored in the national literature.
REFERENCES
1.Marcon SS, Radovanovic CAT, Waidman MAP, Olireira MLF, Sales CA. Vivência e reflexões de um grupo de estudos junto às famílias que enfrentam a situação crônica de saúde. Texto & contexto enferm. 2005; 14(spe):116-24.
2.Freitas M C, Mendes MMR. Condição crônica: análise do conceito no contexto da saúde do adulto. Rev. latinoam. enferm. (online). 2007; 15(4):590-97.
3.Souza RP, Viviani AG. Qualidade do sono em crianças hospitalizadas. Pediatr. Mod. 2014; 50(3).
4.Lee S, Narendran G, Madsen LT, Schulte F. A systematic review of sleep in hospitalized pediatric câncer patients. Psycho-oncology. 2016; 26(8):1059-69.
5.Pinto JPF. Estudo da qualidade do sono dos pacientes internados no serviço de cirurgia e de medicina interna do Centro Hospitalar Cova da Beira [tese de doutorado]. Covinhã(Pt): Universidade da Beira do Interior; 2014.
6.Paiva MB, Souza CAC, Soares E. Fatores que interferem na preservação do sono e repouso de crianças em terapia intensiva. Esc. Anna Nery Rev. Enferm. 2006; 10(1):29-35.
7.Nunes MDR. Avaliação da fadiga em crianças e adolescentes hospitalizados com câncer e sua relação com padrão de sono e qualidade de vida relacionada à saúde [tese de doutorado]. Ribeirão Preto (SP): Universidade de São Paulo; 2014.
8.Setoyama A, Ikeda M, Kamibeppu K. Objective assessment of sleep status and its correlates in hospitalized children with cancer: Exploratory study. Official Journal of the Japan Pediatrics International. Pediatr. int. 2016; 58(9):842-49.
9.Linder LA, Christian BJ. Nighttime sleep characteristics of hospitalized school-age children with câncer. Oncol. Nurs. forum. 2012; 39(6):553–61.
10.Whittemore R, Knafl K. The integrative review: updated methodology. J. adv. nurs. 2005; 52(5):546-53.
11.Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & contexto enferm. 2008; 17(4):758-64.
12.Walker AJ, Johnson KP, Miaskowski C, Lee KA, Gedaly-Duff. Sleep quality and sleep hygiene behaviors of adolescents during chemotherapy. J. clin. sleep med. 2010; 6(5):439-44.
13.Herbert AR, Lima J, Fitzgerald DA, Seton C, Waters KA, Collins JJ. Exploratory study of sleeping patterns in children admitted to Hospital. Journal of Paedriatrics and Child Health. 2014; 50(8):632-38.
14.Péreza MAI, Rodríguez AD, Insuga VS, Carral JD, Martín VP, Solana LGG . Prevalence of sleep disorders in patients with neurofibromatosis type 1. Neurología. 2015; 30(9):561-5.
15.Stuttard L, Beresford B, Clarke S, Beecham J, Curtis J. A preliminary investigation into the effectiveness of a group-delivered sleep management intervention for parents of children with intellectual disabilities. Journal of Intellectual Disabilities. 2015; 19(4):342–55.
16.Teng YT, Chiang LC, Lue KH, Chang SW, Wang L, Lee SP, et al. Poor sleep quality measured by polysomnography in non-obese asthmatic children with or without moderate to severe obstructive sleep apnea. Sleep medicine. 2014; 15(9):1062-7.
17.Ward TM, Sonney J, Ringold S, Stockfish S, Wallace CA, Landis CA. Sleep disturbances and behavior problems in children with and without arthritis. J. pediatr. nurs. 2014; 29(4):321–28.
18.Matthews EE, Neu M, King N. Sleep in mother and child dyads during treatment for pediatric acute lymfoblastic leukemia. Oncol. nurs. forum. 2014; 1(6):599-610.
19.Hinds PS, Hockenberry M, Zhang L, Razzouk BI, McCarthy K, Cremer L, et al. Nocturnal awakenings, sleep environment interruptions, and fatigue in hospitalized children with cancer. Oncol. nurs. forum. 2007; 34(2):393-402.
20.Zupanec S, Jones H, Stremler R. Sleep habits and fatigue of children receiving maintenance chemotherapy for ALL and their parents. J. pediatr. oncol. nurs. 2014; 27(4):217-28.
21.Nunes MDR, Jacob E, Adlard K, Secola R, Nascimento L. Fatigue and sleep experiences at home in children and adolescents with cancer. Oncol. nurs. forum. 2015; 42(5):498-506.
22.Jacob E, Miaskowski C, Savedra M, Beyer JE, Treadwell M, Styles L. Changes in sleep, food intake, and activity levels during acute painful episodes in children with sickle cell disease. J. pediatr. nurs. 2006; 21(1):23-34.
23.Jacob E, Hesselgrave J, Sambuco G, Hockenberry M. Variations in pain, sleep, and activity during hospitalization in children with cancer. J. pediatr. oncol. nurs. 2007; 24(4):208-19.
24.Linder LA, Christian BJ. Nighttime sleep disruptions, the hospital care environment, and symptoms in elementary school-age Children with cancer. Oncol. nurs. forum. 2013; 39(6): 553–61.
25.Graves JK, Jacob E. Pain, coping, and sleep in children and adolescents with sickle cell disease. J. child adolesc. psychiatr. nurs. 2014; 27(3):109-20.
26.Ward TM, Yuwen W, Voss J, Foell D, Gohar F, Ringold S. Sleep fragmentation and biomarkers in juvenile idiopathic arthritis. Biol. res. nurs. 2016; 18(3):299-06.
27.Heger ER, Calamaro CJ, Bentley LM, Hurley KM, Wang Y, Black MM. Nighttime sleep duration and sleep behaviors among toddlers from low-income families: associations with obesogenic behaviors and obesity and the role of parenting. Childhood Obesity. 2016; 12(5):392-400.
28.Lourenção DCA, Tronchin DMR. Segurança do paciente no ambiente cirúrgico: Tradução e adaptação cultural de instrumento validado. Acta Paul. Enfem. (Online) 2016; 29(1):1-8.
29.Alexandre NMC, Coluci MZO. Validade de conteúdo nos processos de construção e adaptação de instrumentos de medidas. Ciênc. saúde coletiva. (Online). 2011; 16(7):3061-8.
30. Salgado APA, Adirson DM, Cava AM, Camacho KG. O sono do recém-nascido em unidade de terapia intensiva neonatal. Rev. enferm. UERJ. 2011; 19(4):644-9.
31.Hysing M, Sivertsen B, Stormark KM, Elgen I, Lundervold AJ. Sleep in children with chronic illness, and the relation to emotional and behavioral problems—A population-based study. Journal of Pediatric Psychology. 2009; 34(6):665–70.
32.Ferreira RER, Silvares EFM, Pires MLN, Assumpção FB, Moura JCB. Sono e comportamento em crianças. Rev. psicol.: teoria e prática. 2016; 18(2):159-72.
33.Zeller B, Loge JH, Kanellopoulos, A, Hamre H, Wyller VB, Ruu E. Chronic fatigue in long-term survivors of childhood lymphomas and leukemia: persistence and associated clinical factors. J. pediatr. hematol. oncol. 2014; 36(6):438–44.
34.Daniel L, Kazak AE, Li Yimei, Hobbie W, Ginsberg J, Butler E, et al. Relationship between sleep problems and psychological outcomes in adolescent and young adult cancer urvivors and controls. Support care cancer. 2016; 24(2): 539–46.
35.Goes ACJ, Reis LAB, Silva MBG, Kahlow BS, Skare TL. Artrite reumatoide e qualidade do sono. Rev. bras. reumatol. (Online). 2017; 57(4):294–8.
36.Góes SM, Cieslak F, Stefanello JMF, Milano GE, Paiva E, Leite N. Sono não-reparador e comorbidades associadas em mulheres com fibromialgia. Fisioter mov. 2009; 22(3):323-33.
37.Halal CSE, Matijasevich A, Howe LD, Santos IS, Barros FC, Nunes ML. Short sleep duration in the first years of life and obesity/overweight at age 4 years: a birth cohort study. J. pediatr. 2016; 168(3):99-103.
38.Oliveira VM, Brasil MR, Chumlhak Z, Cordel PT, Czuy GHB, Silva SR. Nível de aptidão física em escolares:influência do índice de massa corporal, sexo e quantidade de sono. Rev. Saúde Meio Ambient. 2017; 6(1):4-17.