(*) Descriptive level for Pearson's Chi-square test
(**) Descriptive level for Fisher's Exact Test
(***) MW - Minimum Wage (Year 2014 = R $ 724.00, Year 2015 = R $ 788.00)
ORIGINAL RESEARCH
Factors associated with changes in mammograms
Neide DerenzoI; Elen Ferraz TestonII; Willian Augusto de MeloIII; Maria Antonia Ramos CostaIV; Marcelo Picinin BernuciV
I
Nurse. Master. Permanent Professor, State University of Paraná - Paranavaí
campus. Brazil. E-mail: neidederenzo@hotmail.com
II
Nurse. PhD. Assistant Professor, State University of Paraná - Paranavaí
campus. Brazil. E-mail: elen-1208@hotmail.com
III
Nurse. PhD. Permanent Professor, State University of Paraná - Paranavaí
campus. Brazil. E-mail: profewill@yahoo.com.br
IV
Nurse. PhD. Permanent Professor, State University of Paraná - Paranavaí
campus. Brazil. E-mail: enfunespar1982@hotmail.com
IV
Nurse. PhD. Assistant Professor, State University of Paraná - Paranavaí
campus. Brazil. E-mail: elen-1208@hotmail.com
V
Biological Sciences. Post PhD. Permanent Professor, University Center of
Maringá. Brazil. E-mail: mbernuci@gmail.com
DOI: https://doi.org/10.12957/reuerj.2018.31640
ABSTRACT
Objective: to examine factors associated with changes in mammograms. Method: in this cross-sectional study of 145 women receiving care under the family health strategy in a municipality in northwestern Paraná, Brazil, data were collected by semi-structured interviews between August 2014 and October 2015 and analyzed using Pearson's Chi-square test and Fisher's exact test. The project was approved by the research ethics committee. Results: the women were of mean age 52.5 years. Those who were white (OR = 0.17), nulliparous (OR = 4.53), with alterations at self-examination (OR = 12.72), clinical examination (OR= 35.75) and a history of previous problems (OR = 9.45) presented a greater likelihood of changes in mammography. Conclusion: the factors associated with altered mammography were white skin color, nulliparity, alterations during self-examination and clinical examination, and a previous breast problem.
Descriptors: Prevention of diseases; self exam; mammography; healthcare professional.
INTRODUCTION
Cancer is the leading cause of death in the world and in Brazil. Estimates for the biennium 2016-2017, indicate the occurrence of about 600 thousand new cases1. In developing countries 70% of deaths are due to cancer, and most cases are diagnosed in more advanced stages making treatment difficult1.
Among the most prevalent types of cancer is breast cancer. The high incidence is influenced by the increase in life expectancy, the process of urbanization and industrialization2,3 as well as the improvement of diagnostic technology and the expansion of screening programs 4,5. However, increased incidence and mortality trends reflect differences in the patterns of risk factors, access and availability of screening for early detection and timely treatment5,6.
A number of factors are related to the late diagnosis of neoplasms such as difficult access to health services, incomplete or non-existent information regarding the self-examination and prevention tests, and even the predominant screening strategy, characterized by spontaneous search of the target population7.
Knowing these risk factors associated with the occurrence of breast cancer allows the planning of new intervention strategies to optimize early detection and favor the survival of women8,9. In this aspect, this study aimed to analyze the factors associated with mammographic changes of women inserted in the family health strategy (FHS).
LITERATURE REVIEW
Breast cancer is the second most common type of cancer in the world and the most common among women, representing a permanent source of concern in public health services. It is worth mentioning that early detection is a form of secondary prevention and aims at identifying cancer in early stages, when the disease has a greater chance of better prognosis, and also generating lower costs to the health care system3.
In the Brazilian context, a study pointed out that, since 2004, cancer has become a priority and has gained visibility in the agenda of public policies, advancing since then in structuring the health care network at different levels of attention, with a focus on screening and early diagnosis10. The objective of the screening is to perform relatively simple tests in healthy people in order to identify diseases in pre-clinical (asymptomatic) stages. At the same time, the purpose of early diagnosis is to identify people with initial signs and symptoms of a particular disease, emphasizing the quality and guarantee of comprehensive care at all stages of the disease4.
In Brazil, according to the review of the Guidelines for the Early Detection of Breast Cancer, screening actions for breast cancer include primarily mammographic examination, breast self-examination (BSE) and clinical breast examination (CBE)3. In view of this, studies about the knowledge women about screening tests for breast cancer are necessary, so that health services can have subsidies for the planning of active search strategies, development of educational actions and prevention of the disease.
We reiterate the need for holistic and comprehensive care for women in primary health care beyond the focus on the physical pregnant body, providing knowledge on self-care actions in relation to their general health11. The study found that women's knowledge of the importance of self-examination of the breasts, when stimulated by health professionals, works as a protective factor for the early detection of cancer and promotes sexual and reproductive health12.
METHODOLOGY
This is a cross-sectional and analytical study developed in a municipality in the northwestern region of PR, with a population of 81,590 inhabitants, of which 42,308 are women13. The 24 FHS teams cover 100% of the population and are distributed in 12 basic health units.
In August 2014, 14,638 women aged between 35 and 69 years were enrolled in the FHS teams. From this total, a probabilistic and systematic sample of cadastral records was calculated, adopting the prevalence of breast cancer of 80 per 100 thousand women and considering a 95% confidence level and a 5% probabilistic error. After inclusion of a further 30% to cover possible losses, a final sample of 145 women was obtained.
After clarification regarding the objectives and method of the research, data were collected through semi-structured interviews using an adapted instrument developed by Batiston14, from August 2014 to October 2015. This was composed of three blocks of questions referring to the independent variables: sociodemographic characteristics (age, marital status, schooling, ethnicity, professional occupation and income); reproductive history (age of first menstruation, age at first sexual intercourse, number of children, maternal age at first child, time of breastfeeding, use of oral contraceptives); and reported knowledge about risk factors for development of breast cancer, with open and closed alternatives of multiple choices. The response variable was mammography with or without alterations.
A pilot test was conducted with 30 women out of the original sample plan in order to verify possible inconsistencies and/or difficulties in interpreting the questions in relation to the research objective.
Measurements of simple proportions and measures of central tendency (mean and median) were verified through descriptive statistics; for bivariate analysis, the Pearson chi-square test and the Fisher's exact test were used when one of the research variables presented a frequency of less than six. The adjusted odds ratio was calculated to estimate the measures of association between variables. A significance level of 5% (p < 0.05) and a 95% confidence interval were considered for all analyses. Analyses were performed with the Excel for Windows software, version 2010 and Epi Info version 7.2.1.
The study was approved by the Committee of Ethics in Research with Human Beings of the Cesumar University Center (UniCesumar) under Opinion nº 977.791.
RESULTS AND DISCUSSION
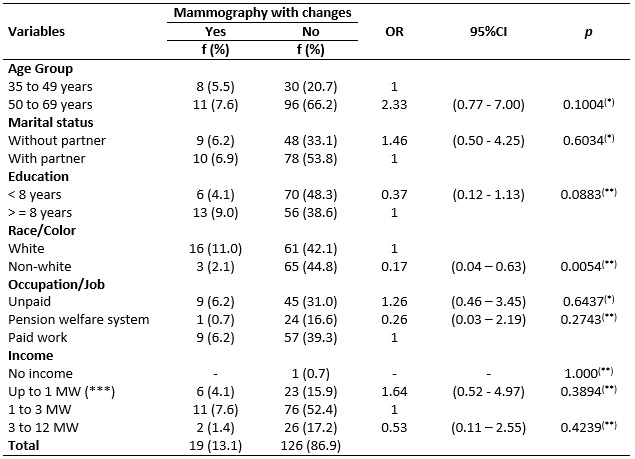
The mean age of women was 52.5 years (± 9.3 of standard deviation) and white women were 5.6-fold more likely (p = 0.0054, OR = 0.17, 95% CI = 04-0.63) to present mammographic changes, as shown in Table 1.
TABLE 1:
Sociodemographic characteristics according to the results of mammographies
reported by women assisted at by FHS teams. Paranavaí, Paraná, Brazil,
2014-2015.
(*)
Descriptive level for Pearson's Chi-square test
(**)
Descriptive level for Fisher's Exact Test
(***)
MW - Minimum Wage (Year 2014 = R $ 724.00, Year 2015 = R $ 788.00)
The prevalence of altered mammographies in women aged between 50 and 69 years corroborates the literature; menopausal women are at higher risk to develop breast cancer due to intense hormonal variations. However, although it is not a routine condition, breast cancer has now been observed in a significant number of young women, especially those with a positive family history of premenopausal breast cancer and genetic risk factors 3,15,16. Given the knowledge of risk factors, it is important to emphasize the importance of health education actions that stimulate early detection because this would be an important strategy for better prognosis.
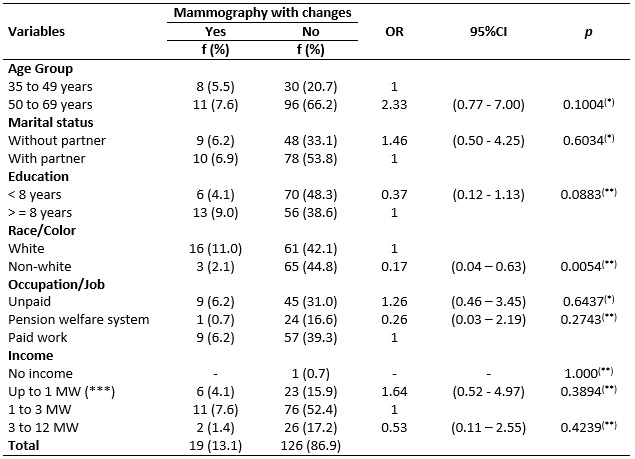
Regarding color, although historically white women had the highest rates of breast cancer incidence, the rates are converging towards white and African American women due to the etiological heterogeneity and the different effects of risk factors such as obesity and parity, for example 17,18. In this context, considering the reproductive history, women who did not have children presented 4.5-fold higher chances to present mammographic changes (OR = 4.53, CI95% = 1.18-17.32), according to Table 2.
TABLE 2:
Reproductive and gynecological history according to results of
mammographies reported by women assisted by FHS teams. Paranavaí, Paraná,
Brazil, 2014-2015.
(*)
Descriptive level for Fisher's Exact Test
It is worth noting that nulliparity has been also pointed out by other studies as a risk factor for breast cancer because breastfeeding is a protective factor due to the complete differentiation of breast cells and shorter time of exposure to the action of sex hormones that decrease during amenorrhea, induced by lactation19,20.
It should be noted that health professionals are the main source of information on risk factors, prevention and characteristics of the disease. Moreover, the importance of establishing an effective communication process between professionals and patients is reiterated. Besides passing on information, professionals must encourage women's awareness of self-care actions21.
Although there are innumerable strategies and programs to guide and stimulate breast cancer prevention, the way these measures are implemented is still questionable, since most women seek help when the disease is manifesting signs and symptoms22,23. Furthermore, the worst prognosis of women assisted in the Brazilian public service has also contributed to diagnosis of the disease at a very advanced stage 24.
Thus, it should be emphasized that although there are national and regional policies aimed at early detection, breast cancer in Brazil is still an important public health problem due to late diagnosis. This can be attributed to difficulties in accessing public health services, the imbalance between supply and demand for services, and the inefficient management of the municipal and state spheres to define demand flows, especially for suspected cases of breast cancer, and the lack of knowledge about possible risk factors and treatment methods24.
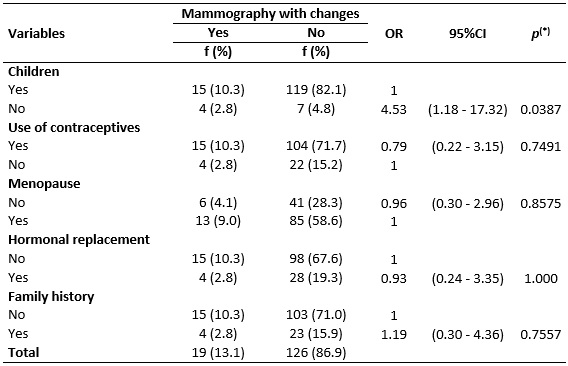
Regarding the changes perceived by women in self-examination, they were approximately 13-fold more likely to be confirmed by mammography (OR = 12.72, 95% CI = 3.72-43.45, p < 0.01). Likewise, lesions detected in the clinical examination and history of previous problems were also statistically associated with posterior mammographic confirmation (p < 0.01) (See Table 3).
TABLE 3:
Screening for breast cancer according to mammographic results reported by
women assisted by FHS teams. Paranavaí, Paraná, Brazil, 2014-2015.
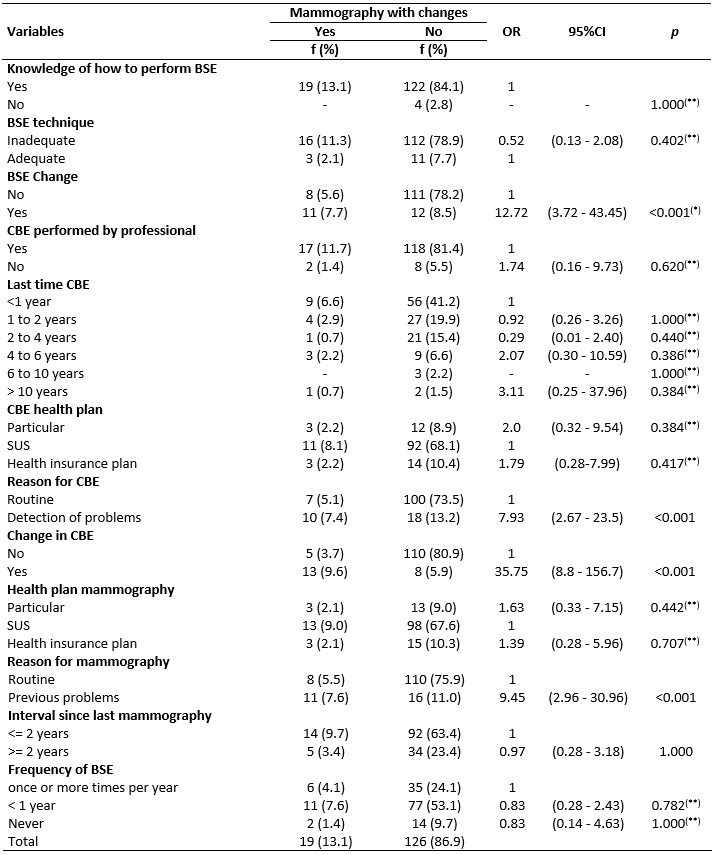
(*)
Descriptive level for Pearson's Chi-square test
(**)
Descriptive level for Fisher's Exact Test
Self-examination and clinical examination of the breasts represent the main methods of early detection of breast cancer and have a positive impact on the reduction of morbidity and mortality. However, in the current context of the health services, not only the explanation on how to perform the self-examination is needed, but also the practical demonstration during the clinical examination in order to stimulate the learning by the women. Therefore, the inclusion of this practice should be prioritized in all consultations of women regardless of the existence of complaints. A study carried out in Ethiopia with health professionals evidenced a reduced practice of self-examination among the professionals themselves and pointed out the need to invest in actions to stimulate self-examination, initially among professionals, in order to effectively reach the community 25,26.
Besides the awareness of professionals, the need for continuous training on the technique of clinical examination of the breasts, the differentiation of the main findings and the distribution of the different points of attention for the adequate and timely referral of patients also stand out. A study indicated that 75% of the women affirmed having done the clinical examination of the breasts and the last cytopathological examination for cervical cancer, but some of them reported that the presence of nodules was not detected during the examination although the nodule was already present 25.
Finally, we emphasize the importance of comprehensive and qualified care for women, as well as active listening on the part of professionals and a detailed anamnesis in order to identify risk factors for the development of cancer, such as a history of breast problems. Knowing the patients, the context in which they are inserted, and their behaviors and risk factors allows the multidisciplinary team to provide a person-centered care, attending specificities and adapting the proposals of intervention to the patients27.
CONCLUSION
The factors associated with mammographic changes were white women, nulliparity, identification of changes during self-examination and clinical examination, and the existence of a previous breast problem.
These findings reinforce that health education actions need to emphasize and enable women to adequately perform self-examination of the breasts. Health professionals also need ongoing training to perform the clinical examination of the breasts and identify changes. This has direct implications for managers of health services, in the sense that they should make continuing education possible in the health service, contemplating the improvement of the techniques and the follow-up of protocols.
Although performed only in one municipality, we believe that the results of the present study contribute to the ongoing discussion among health teams regarding the quality of the breast cancer prevention strategies implemented.
REFERENCES
1. Ministry of Health (Br). National Institute of Cancer José Alencar Gomes Da Silva - INCA. Incidence of Cancer in Brazil. Estimates 2016. [cited in Sep 1, 2017]. Available from: www.inca.gov.br/estimativa/2016/index.asp?ID=2
2. Ghoncheh M, Mirzaei M, Salehiniya H. Incidence and mortality of breast cancer and their relationship with the human development index (HDI) in the world in 2012. Journal Cancer Prev. [Internet]. 2015 [cited in Oct 2, 2017]; 16 (18): 8439-43. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26745098
3. Ministry of Health (Br). National Institute of Cancer José Alencar Gomes da Silva. Guidelines for the early detection of breast cancer in Brazil. Rio de Janeiro: INCA; 2015.
4.Panis C, Kawasaki ACB, Pascotto CR, Justina EYD, Vicentini GE, Lucio LC, et al. Critical review of cancer mortality using hospital records and potential years of life lost. Einstein [internet]. 2018 [cited in Jan 13, 2018]; 16 (1). Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1679-45082018000100204&lng=en&nrm=iso&tlng=en&ORIGINALLANG=en
5. De Santis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International variation in female breast internet]. 2015 [cited in Oct 16, 2017]; 24 (10): 2654-64. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26359465
6.Park B, Shin A, Jung-Choi K, Ha E, Cheong HK, Kim HJ, et al. Correlation of breast cancer incidence with the number of motor vehicles and consumption of gasoline in Korea. Journal Cancer Prev. [Internet]. 2014 [cited in Nov 08, 2017]; 15 (7): 2959-64. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24815431
7.Gonçalves LLC, Travassos GL, Almeida AM, Guimarães AMD'N, Gois CFL. Barriers in health care to breast cancer: perception of women. Rev. Esc. Enferm. USP. [Internet]. 2014 [cited in Sep 07, 2017]; 48 (3): 394-400. Available from: http://dx.doi.org/10.1590/S0080-623420140000300002
8. Ministry of Health (Br). National Institute of Cancer José Alencar Gomes da Silva - INCA. Coordination of Prevention and Surveillance. 2014. [cited in Jan 18, 2017]. Available from: http://www.inca.gov.br/estimativa/2016/
9.Marques CAV, Silva VR, Gutiérrez MGR. Actions of nurses in the detection of breast cancer. Rev. enferm. UERJ.2017; 25: e22639
10. Marques CAV, Figueiredo EN, Gutiérrez MGR. DOI: Public health policies for breast cancer control in Brazil. Rev. enferm. UERJ. [Internet]. 2015 [cited in Dec 08, 2017]; 23 (2): 272-8.Available from: http://www.facenf.uerj.br/v23n2/v23n2a21.pdf
11.Zapponi ALB, Tocantins FR, Vargens OMC. The nurse in the early detection of breast cancer in primary health care. Rev. enferm. UERJ. [Internet]. 2015 [cited in Dec 12, 2017]; 23 (1): 33-8.Available from: http://www.facenf.uerj.br/v23n1/v23n1a06.pdf
12. Conceição Ferreira M, Ferreira S, Ferreira N, Andrade J, Duarte JC. Adherence to the screening of cervical and breast cancer of Portuguese women. Millenium [internet]. 2014 (cited in Dec 13, 2017); 47 (2): 83-96. Available from:
http://revistas.rcaap.pt/millenium/article/viewFile/8111/5709
13. Brazilian Institute of Geography and Statistics. Population count 2010. Rio de Janeiro: 2011. [cited on Nov 12, 2017]. Available from: http://www.ibge.gov.br/home/estatistica/populacao/censo2010/indicadores_so-ciais_municipais/social_indicators_municipal.pdf
14.Batiston AP, Tamaki EM, Souza LA, Santos MLM. Knowledge and practice on risk factors for breast cancer among women aged 40 to 69 years. Rev. Bras. Maternity Health. [Internet]. 2011 [cited in 02 Nov, 2017]; 11 (2): 163-71. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1519-38292011000200007
15.Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends-an update. Cancer Epidemiol. Biomarkers Prev. [internet]. 2017 [cited in Nov 22, 2017]; 25(1):16-27. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26667886
16.Winters S, Martin C, Mueprhy D, Shokar NK. Breast cancer epidemiology, prevention and screening. Prog. Mol. Biol. Transl. Sci . internet]. 2017 [cited in Oct 12, 2017]; 151: 1-32. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29096890
17.Höfelmann DA, Dos Anjos JC, Laurenti AA. Survival for ten years and prognostic factors for women with breast cancer in Joinville in the State of Santa Catarina, Brazil. Ciênc. saúde coletiva [internet] (Online). 2014 [cited in Dec 08, 2017]; 19(6): 1813-24. Available from: http://www.scielo.br/scielo.php?pid=S1413-81232014000601813&script=sci_abstract&tlng=en
18.De Santis C, Ma J, Bryan L, Jemal A. Breast cancer statistics. CA: A Cancer Journal for Clinicians [internet] .2013 [cited in Dec 27, 2017]; 64(1):52-63. Available from: http://onlinelibrary.wiley.com/doi/10.3322/caac.21203/full
19.Lauter DS, Berlezi EM, Rosanelli CLSP, Loro MM, Kolankiewicz ACB. Breast cancer: case control study in Southern Brazil. Rev. Ciência & Saúde [internet]. 2014 [cited in Jan 12, 2017]; 7(1):19-26. Available from: https://www.researchgate.net/publication/287812896_Cancer_de_mama_estudo_caso_controle_no_Sul_do_Brasil
20.Penha NS, Birth DEB, Pantoja ACC, Oliveira AEM, Maia CSF, Vieira ACS. Socio-demographic profile and possible risk factors in women with breast cancer: a portrait of the Amazon. Journal of Basic and Applied Pharmaceutical Sciences [internet]. 2014 [cited on 02 Feb 2017]; 34 (4): 579-84. Available from: http://servbib.fcfar.unesp.br/seer/index.php/Cien_Farm/article/viewFile/2708/1498
21.Kaplan HG, Malmgren JA, Atwood MK, Calip GS. Effect of treatment and mammography detection on breast cancer survival over time: 1990-2007. Câncer [internet]. 2015 [cited in Jan 18, 2017]; 121(15): 2553-61. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25872471
22.Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and Ethnicity in the United States. JAMA. [internet] 2015 [cited in Feb 18, 2017]; 313(2):165-73. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25585328
23.Bellolio E, Pineda V, Burgos ME, Iriarte MJ, Becker R, Araya JC, et al .Predictive value of breast imaging report and database system (BIRADS) to detect cancer in a reference regional hospital. Rev. méd. Chile [internet]. 2015 [cited in Feb 08, 2017]; 143(12):1533-8. Available from: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S003498872015001200005&lng=en&nrm=iso
24.Oshiro ML, Bergmann A, Silva RG, Costa KC, Travaim IEB, Silva GB, et al. Advanced Breast Cancer as a Sentinel Event for Evaluation of the Program for Early Detection Breast Cancer in the Center-West of Brazil. Revista Brasileira de Cancerologia [internet]. 2014 [cited in Mar 15, 2017]; 60 (1): 15-23. Available from: http://www.inca.gov.br/rbc/n_60/v01/pdf/04-artigo-cancer-de-mama-avancado-como-evento-sentinela-para-avaliacao-do-programa-de-detecção-do-cancer-de-mama-no-centro-oeste-do-brasil.pdf
25.Muluken A, Gedefaw A, Alemtsehay M. Assessment of factors associated with breast self-examination among health workers in West Gojjam Zone, Northwest Ethiopia. Int. Journal Breast Cancer [internet]. 2013 [cited in Mar 08, 2017]; 814395. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3835626/?tool=pubmed
26.Shamsi U, Khan S, Usman S, Soomro S, Azam I. A multicenter matched case control study of breast cancer risk factors among women in Karachi, Pakistan. Journal Cancer Prev. [internet] 2013 [cited in Mar 17, 2017];14(1):183-8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23534721
27.Partridge AH, Elmore JG, Saslow D, McCaskill-Stevens W, Schnitt SJ. Challenges in ductal carcinoma in situ risk communication and decision-making: report from an American Cancer Society and National Cancer Institute workshop. CA Cancer Journal Clin . [internet] 2012 [cited in Mar 05, 2017]; 62(3): 203-10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112288/?tool=pubmed