Figure 1: Diagnosis, outcomes and priority nursing interventions for burned patients. Natal, Brazil, 2016.
ORIGINAL RESEARCH
Implementing the nursing process for a burn patient: a case study
Vinicius Lino de Souza NetoI; Rayane Teresa da Silva Costa II; Erlivânia Aparecida de LucenaIII; Suellen Cristina da SilvaIV; Vanessa Mandu PereiraV; Richardson Augusto Rosendo da SilvaVI
I
Nurse. Master in Nursing from the Federal University of Rio Grande do
Norte. Natal, Brazil. E-mail: vinolino@hotmail.com
II
Undergraduate Nursing Student, Federal University of Rio Grande do Norte.
Natal, Brazil. E-mail: rayane.teresa@hotmail.com
III
Undergraduate Nursing Student, Faculdade Natalense de Ensino e Cultura de
Natal. Rio Grande do Norte, Brazil. E-mail: erli87238566@gmail.com
IV
Undergraduate Nursing Student, Faculdade Natalense de Ensino e Cultura de
Natal. Rio Grande do Norte, Brazil. E-mail:
suellenlethicia.c1@gmail.com
V
Undergraduate Nursing Student, Faculdade Natalense de Ensino e Cultura de
Natal. Rio Grande do Norte, Brazil. E-mail: mandu_vanessa@hotmail.com
VI
Nurse. PhD in Health Sciences. Professor of the Nursing Department of the
Federal University of Rio Grande do Norte. Natal, Brazil. E-mail: rirosendo@hotmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2018.30962
ABSTRACT
Objective: to implement the nursing process (NP) in the context of care for a burn patient treated at a public health institution. Method: in this case study, the theoretical frame of reference was given by Horta's Basic Human Needs (1979). The NP was implemented in the following steps: completion of the case history and physical examination, preparation of Nursing Diagnoses (NDs), planning, and implementation of the activities recommended by the interventions. Sequential patient evaluations were then performed. Results: after analyzing the clinical indicators, the priorities were listed as ineffective respiratory pattern, risk of infection and impaired skin integrity. The goals, interventions and activities to be implemented for further evaluation were then planned and specified. Conclusion: implementation of the NP in care for burn patient made it possible to produce quality care guided by scientific knowledge.
Descriptors: Nursing processes; nursing; burns; nursing care.
INTRODUCTION
Burns are traumatic wounds caused, in most cases, by thermal, chemical, electrical or radioactive agents. They act on the coating tissues of the human body, determining partial or total destruction of the skin and its attachments, being able to reach deeper layers, such as subcutaneous cellular tissue, muscles, tendons and bones. Burns are classified according to their depth and size and are usually measured by the percentage of the body surface affected1.
It is estimated that around 300,000 burn deaths have occurred in the world, caused by fire. In North America, burn injuries were responsible for approximately 282,000 deaths, characterizing the fifth cause of death in the country2.
In Brazil, about one million burn injuries occur annually, of which only 200,000 patients seek hospital care. Thus, it is the third cause of death in the different age groups, and the second in children under four. The cause is related to several factors, among which we can mention scald, fireworks, chemical substances, and excessive exposure to the sun1-2.
Burns, when very extensive, multiple and deep, lead to complications in the hemodynamic state, causing the loss of the essential factor of thermal regulation and protection, leading to the development of circulatory collapse, with signs of hypovolemia, edema, shock, pulmonary alterations, such as bronchoconstriction, thoracic constriction and atelectasis, renal changes, sepsis, and paralytic ileus3.
To avoid such damages, people with burns require multidisciplinary assistance, so that their needs are met. The process of caring is a complex act that requires a relationship of care and attention, which implies putting oneself in the other's place, understanding that the patient is influenced by internal and external stressor factors1. In view of this, nursing professionals are constantly challenged in their daily lives, requiring technical and scientific tools and knowledge that optimize care and provide intelligent, qualified and comprehensive assistance that meets the needs of their patients4.
The Systematization of Nursing Care (SNC) emerges as a proposal for the organization of care, allowing the professional to think critically about the signs of nursing, thus generating a more scientific and critical care. Among the several ways to implement systematic practices, the most adopted are the following: care plan, nursing process, protocols and decision models. These methods ensure documentation of the care provided by the nursing staff4-5.
The Nursing Process (NP) is characterized as a methodological instrument that documents nurses' practice and prioritizes basic human needs, and is organized in interdependent, interrelated and recurrent stages, such as history, diagnosis, interventions, implementation and evaluation5.
The different phases of the NP favored the development of several classification systems related to Nursing Diagnoses. Among the various classification systems developed from the different phases of the NP, the NANDA International Taxonomy, the Nursing Interventions Classification (NIC) and the Nursing Outcomes Classification (NOC)6-8 stand out.
Thus, the implementation of NP to the patient with burns requires the nurse to know the pathophysiological process of this injury, to elaborate the nursing process based on scientific evidence, respecting the specificities of the patients. In this sense, the nurse has a complex role in the care of this patient4, especially in the evaluation for the detection of problems and needs for the implementation of specific care.
In this way, it is crucial to evaluate the severity of the burn, the extension, the depth of the injury generated in the body, the physical disorders, such as loss of fluid volume, metabolic changes, body deformities and risk of infection, besides the complications arising from the burn, which can cause greater complications in the health status of the patient6.
In this context, the identification of the NDs, which is the second stage of the NP, will enable practitioners to identify the patient's needs, thus facilitating the elaboration of the actions, with subsequent evaluation of the results achieved5. Therefore, it is important that the nurse be able to identify the nursing diagnoses in order to plan and implement their actions, as well as to evaluate them, resulting in a quality assistance to this clientele.
Therefore, the present study aimed to implement the NP in the context of care of a burned patient assisted at a public health institution.
THEORETICAL FRAMEWORK
The proposal of the theory of Horta was published in 1970 and influenced the Brazilian nursing in the movement of use of a methodology for the nursing process based on basic human needs. Thus, Horta made it motivated by the idea of developing a theoretical model for nursing that was far from the biomedical model. Looking for the theoretical-philosophical framework that redirects the practice of nursing, he used the human sciences and found support in the Humanist Psychology of Maslow and Mohana, however, still maintained the bond with the natural sciences9.
His theory encompasses three general laws governing universal phenomena: the law of equilibrium (homeostasis or hemodynamics), which states that the whole universe is maintained by processes of dynamic equilibrium between its beings; the law of adaptation, according to which all beings in the universe interact with their external environment, always seeking forms of adjustment to keep themselves in balance; and the law of holism, which considers that the universe is a whole, the human being is a whole, the human being is a whole, the cell is a whole; this whole is not merely the sum of the constituent parts of each being9.
It is important to emphasize that the patient burned due to tissue loss and the risk for infection tends to present their basic needs, such as oxygenation, hydration, comfort, safety and nutrition, among others. This reality brings negative impacts to the biopsychosocial being, as well as the lifestyle of the person and their family5.
In this sense, it is believed that such a theoretical framework frames the burn patient, since it provides the identification of altered basic human needs, whether psychobiological, psychosocial or psycho-spiritual, that is, it leads the nurse to reflect on the dimensioning of work in the restoration of needs in the face of a traumatic event. Also, it makes the professional observe the patient as a whole, whether individual or collective, and projects that such care should be mantained.
METHOD
This is a case study, characterized as a tool that corroborates with the practical and clinical teaching of nursing, enabling the elaboration of care plans. In addition, the construction of the first expressions of the NP was made possible through case studies10. The study was carried out at the Burn Treatment Center (CTQ in Portuguese) of a public hospital in the northeast of Brazil, from April to May 2016. The present study adopted the Basic Human Needs of Horta as a theoretical reference. The implementation of the NP was based on the respective moments, namely the clinical evaluation, through an interview script and physical examination; then, the elaboration of nursing diagnoses based on NANDA-I, version 2015-2017; planning with definition of nursing outcomes (NOC) and interventions (NIC) and implementation of the activities defined from the interventions and the reassessment of these actions.
Data collection took place at the bedside, in which the patient and the companion were informed about the research and its objectives, and thus consented to participate and signed the Informed Consent Form (ICF). To complement the information, we used some materials such as pulse oximeter to measure the oxygen level; blood pressure through the sphygmomanometer and stethoscope, a thermometer in order to check the thermal curve, and a wristwatch with analog hands, so that each researcher could check heart and respiratory rates, among others.
Thus, the elaboration of the nursing diagnoses was procedural, that is, after analyzing the clinical indicators, the researcher elaborated them based on NANDA-I. Soon after, he elaborated the goals, intervention and activities. In order to construct the indicators, he first sought in the field of scientific and practical production on the subject, through search in the computerized databases of the Virtual Health Library: Latin American and Caribbean Literature (LILACS) and International Literature in Health and Biomedical Sciences (MEDLINE); SCOOPUS, CINAHL, using the descriptors Nursing processes; Terminology; Nursing diagnosis; Nursing; Burns. It was found deficits of studies about the nursing process and the advantages of their application in the practical field, as well as the formulation of instruments that present indicators.
Soon after, it was referred to a group of specialists, formed by five nurses who provide care to the patient burned for more than 15 years in the place where the data were collected. The purpose of the group was to analyze, synthesize and validate such information. For each indicator, a score varying from 1 to 5 was drawn to measure the risks of this patient, that is, the higher the score, the worse their health condition would be. The definition of the score according to the indicators presented in the study was constructed from the NOC.
The analysis of the agreement of the participants of the focus group was adopted the Content Validity Index (CVI) method, which measures the proportion or percentage of specialists who are in agreement on certain aspects of the instrument and its items, represented by the indicators. The items that obtained a concordance of at least CVI ≥ 0.80, considered to be optimal, were considered valid.
The evaluation of the patient occurred in four moments, namely the first contact, the second, with 10 days and then with 15 days and the last one, with 25 days. Throughout the evaluations scores were improving. In this sense, the number of activities was reduced, characterizing the improvement of the clinical picture of the patient.
For this purpose, the present study was certified by the Ethics and Research Committee of the Federal University of Rio Grande do Norte, in accordance with CAAE 47380915.2.0000.5537, Opinion no. 1,117,410, since all the directives and norms of the National Health Council (CNS) were followed.
RESULTS AND DISCUSSION
Nursing history and physical examination
The patient was male, 45 years old, married and had seven children. He had incomplete high school and was self-employed and carpenter. He was admitted on April 14, 2016, at 19:15, coming from the emergency sector, victim of an automobile accident with car explosion He managed to leave with his body on fire, putting out the fire with sand. After almost 20 minutes, he was rescued by the fire department and the team of the Emergency Mobile Service (SAMU), which immediately began the approach. At the time of admission, there were second- and third-degree burns in the upper limbs (9%), thorax (18%) and lower limbs (9%), with 36% of Burned Body Surface (BBS), as well as multiple fractures exposed as in region of the right tibia, and non-exposed fractures in the right pelvis (ischio-pubis region). The patient had a lowered consciousness (Glasgow Scale = 09) and respiratory insufficiency, due to the inhalation of the fuel burn, with SpO2 86%. He was intubated, and was in Mechanical Ventilation (MV). Physical examination showed cold and sticky skin, central pulses present, and inaudible peripherals pulses. Thus, from the clinical indicators presented by the patient, diagnoses were elaborated, following the steps of Gordon's diagnostic reasonings(11), outcomes and priority interventions.
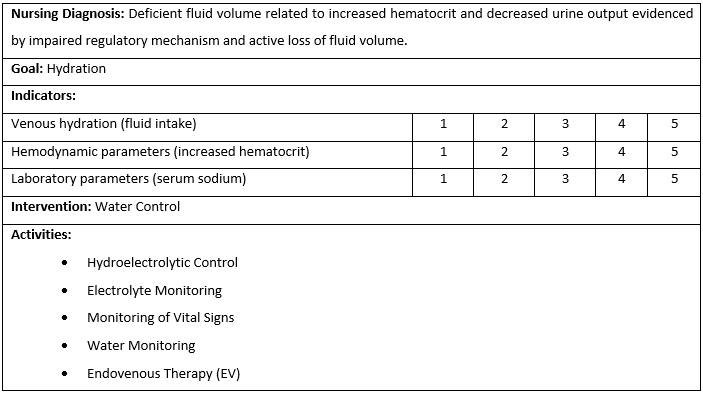
Figure 1 shows that hydration was the goal to be achieved from the proposed activities. Nursing interventions were developed based on the analysis of the clinical indicators and focused on the control of the airways. The main indicators were venous hydration, hemodynamic and laboratory parameters.
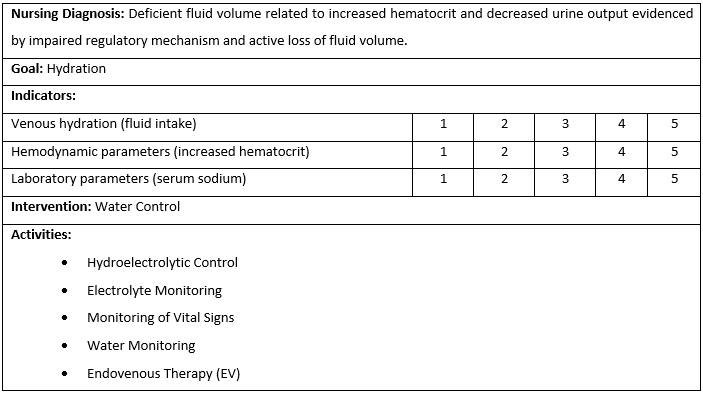
Figure 1:
Diagnosis, outcomes and priority nursing interventions for burned patients.
Natal, Brazil, 2016.
The first evaluation was carried out before the implementation of the proposed activities. In this stage, the patient obtained, in relation to the indicators, a score of 15 points. There was decrease in urinary volume, with an increase in its concentration and a density greater than 1001, increased hematocrit and changes in serum sodium.
The activities were implemented, and in the evaluation of at the 2nd day a significant decrease to 12 points in the score was verified. In the evaluation of the 10th day, a significant evolution was observed, reaching 10 points, presenting a satisfactory clinical evolution. On the 15th day, the patient was evaluated again and an improvement in the score was observed, reaching 9 points, and in the 25th day, it summarized 3 points against the sum of the indicators.
The goal shown in Figure 2 for the Nursing Diagnosis risk for infection was to carry out risk control through the proposed and implemented activities. In the first evaluation, the patient presented 20 points, reaching the maximum score of the indicators. On the 1st evaluation performed, on the 10th day, it was observed that the patient presented an average of 12 points. On the 15th day, the score went from 12 points to 9 points, and on the 25th day the score was 8 points. Thus, this evidenced that the safety measures contribute to a quality care.
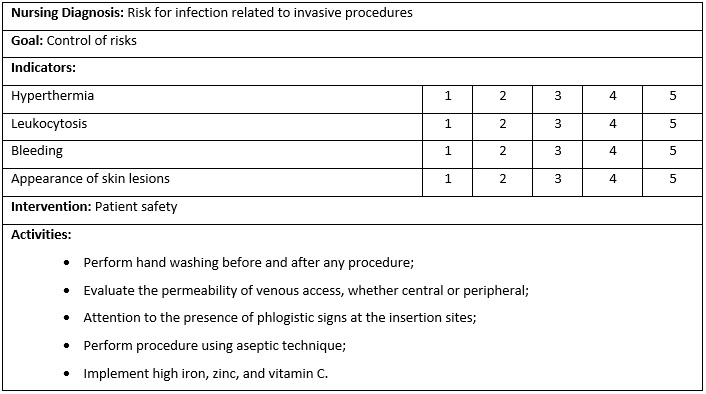
Figure 2:
Diagnosis, outcomes and priority nursing interventions for burned patients.
Natal, Brazil, 2016.
At the first moment of the evaluation of the patient, he presented a maximum score in the three indicators, obtaining 15 points, as shown in Figure 3. In the evaluations, after the start of the implementation of the activities, on the 10th day, the patient presented a positive reduction of the indicators, totaling 12 points. On the 15th day, he had reached 9 points and on the 25th day, 4 points. In this period, nutritional supplementation by glutamine, arginine and omega 3 was emphasized for the patient, who presented impaired skin integrity.
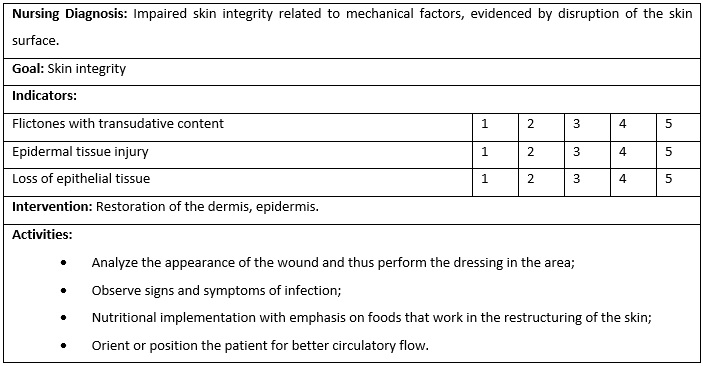
Figure 3:
Diagnosis, outcomes and priority nursing interventions for burned patients.
Natal, Brazil, 2016
Nursing care planning is part of a process to identify inferences and determine necessary interventions for each type of patient, whether they had been mildly, moderately or severely burned, always seeking to reach the desired results and established by nursing, according to the therapeutic treatment. In order for the nursing care plan to be implemented, daily priorities must be established, making the necessary changes according to the alterations in the patient's chart, always performing daily recording of all the actions and intercurrences performed, in addition to seeking to maintain communication with the team7-8.
In this context, the applicability of the SNC became a guiding proposal for nursing care when the Federal Nursing Council (COFEN) approved the Resolution 358/2009 with the objective of implementing the SNC throughout the national territory, since the systematization was underway in countries such as the United States, Chile and Canada, leading to significant improvements in the quality of care4-6. The implementation of the SNC, based on a specific knowledge and critical reflection on the organization and philosophy of nursing work, is a crucial instrument for nurses to manage and optimize nursing care in a safe, dynamic way and competent manner12-14.
Establishing both general and specific interventions is to direct nursing care, always aiming at the well-being and improvement of the patient who suffered some type of burn, whether mildly, moderately or severely burned 15. The interventions raised in this study are in line with commonly identified problems in burn patients, emphasizing that, therefore, it is necessary to evaluate each clinical case, since each one has its peculiarities and needs specific and even complex care16.
One of the points that should be considered in large burnings is volume replacement. The administration of large amounts of intravenous volume is necessary to prevent the patient from going into hypovolemic shock, since the patient after a burn loses a substantial amount of intravascular fluid in the form of mandatory total body edema in addition to the evaporative losses at the burn site17.
Any patient who has suffered a thermal injury is subject to infection. As the residues accumulate on the surface of the wound, they may slow the migration of keratinocytes, consequently affecting the epithelization process. In some cases, the debridement of the burn lesions is necessary in order to remove the tissue contaminated by bacteria and foreign bodies, protecting the patient against the invasion of bacteria18.
The development of the case study revealed that, the identification of the priority nursing phenomena for the burned patient enabled to direct the clinical practice and make it more scientific, less intuitive and more resolute. Thus, there was reduction of the scores related to the indicators defined for each nursing diagnosis and the consequent improvement of the patient after the period in which the activities were implemented. In addition, there was greater optimization and homogeneity of the knowledge among the nursing team, and the planning of care through systematic practices favored the reduction of hospitalization time, implied in the quality of life for the patient, but also reduced costs16.
Such reduction in hospitalization time was perceived in the study patient, since the change from intensive to semi-intensive care occurred in an average of six days, totaling 144 hours, with 30 hours of rest by the nursing team19-20.
The COFEN Resolution no. 253/04 determines that nursing hours aimed at intensive care should be 17.6 hours per client. In the case of the patient in this study, 114 hours were dedicated to him during the six days, totaling 19 hours of nursing care per day. A positive progression was characterized as there was a change from an intensive care setting to semi-intensive care, as a result of improvements in physiological parameters and attenuated dependencies19.
The implication of systematic care, besides specific skills, requires a satisfactory number of nurses, so that continuity of care is given. The dimensioning of nursing personnel is a systematic process, which supports the planning as well as quantitative and qualitative evaluation of professionals, so that it can provide care according to the uniqueness of the health sector, ensuring safety to patients and professionals 17.
Given this, the development of actions and interventions in a systematic way requires acceptance of participatory management and financial developments, as well as the participation of nursing21.
CONCLUSION
The implementation of the Nursing Process in the care of a burned patient enables the development of an assistance based on scientific knowledge, thus allowing an autonomy of the nursing team and the incorporation of new technologies in the care process. The development of NP does not distance the relationship between nurse and patient, but rather strengthens the bonds in a human, welcoming and scientific way. In addition, it improves the quality of care.
Thus, the limitations of the present study include the fact that it has been developed in a given geographical area and for a particular clientele, which does not prevent it from being carried out in other places and improved in other spaces.
REFERENCES
1. Brazilian Society of Burns. [website]. Concept of burns. [cited in Dez 04, 2018] Available from: http://sbqueimaduras.org.br/queimaduras-conceito-e-causas/
2. Paggiaro AO, Cathalá BS, Isaac C, Carvalho VF, Oliveira R, Gemperli R. Epidemiological profile of the skin donor of the Tissue Bank of the Hospital das Clínicas of the University of São Paulo. Rev Bras Queimaduras2017;16(1):23-27.
3. Adanichkin N, Greenwood JE, McArthur A. Face care amongst patients admitted to the Adult Burn Service: a best practice implementation project. JBI Database System Rev Implement Rep. 2015;13(9):369-85.
4. Soares MI, Resck ZMR, Terra FS, Camelo SHH. Systematization of nursing care: facilities and challenges of nurses in care management. Rev Enf Esc Anna Nery.2015; 19 (1): 47- 53.
5. Pinto E , Flóra AMD, Silva LD, Rorato TJ, Requia J, Martins ESR, Zamberlan C, Marinho MGR. The feeling and the nursing care before a severely burned patients. RevBras Queimaduras. 2014;13(3):127-9.
5. Bittencourt GKGD, Crossetti MGO. Critical thinking skills in the nursing diagnostic process. Rev Esc Enferm. 2013; 47(2): 341-47.
6. Zamberlan C, Martins ES, Moura LN, Simone P. The importance of the nurse in the first care to the patients burned in mobile service. Rev Bras Queimaduras. 2014;13(3):185-218.
7. Souza Neto VL, Andrade LL, Agra G, Costa MML. Diagnostic profile of nursing of hospitalized patients in an infectious disease unit. Rev Gaúcha Enferm. 2015;36(3):79-85.
8. Bourke P, Bison AVF. The importance of cooling the burn in pre-hospital care. Rev Bras Queimaduras. 2015;14(1):31-4.
9. Horta WA. Nursing process. São Paulo: EPU; 2011.
10.Silva LAGP, Mercês NNA. Multiple case study applied in nursing research: a case report. Rev Bras Enferm. 2018;71(3):1194-7.
11.Gordon M, Murphy CP, Candee D, Hiltunen E. Clinical judgment: an integrated model. ANS Adv Nurs Sci.1994;16(4):55-70.
12. Costa GOP, Silva JA, Santos AG. Clinical and epidemiological profile of burns: evidence for nursing care. Ciênc Saúde. 2016;8(3):146-55.
13 Lima OBA, Arruda AJCG, Carvalho GDA, Melo VC, Silva AF. Nursing and care to the victim of burns: integrative review. J Nurs UFPE on line. 2013;7(esp):4944-50.
14.King MA, Clanton TL, Laitano O. Hyperthermia, dehydration, and osmotic stress: unconventional sources of exercise-induced reactive oxygen species. Am J Physiol Regu lIntegr Comp Physiol. 2016;310:105–14.
15. Melo TO, Lima AFC. Cost of nursing most frequent procedures performed on severely burned patients. Rev Bras Enferm. 2017 May-Jun;70(3):481-88.
16. Heydarikhayat N, Ashktorab T, Rohani C, Zayeri F. Effect of Post-Hospital Discharge Follow-up on Health Status in Patients with Burn Injuries: A Randomized Clinical Trial. Int J Community Based Nurs Midwifery. 2018 Oct;6(4):293-304.
17. Chan LC, Lee MS, Ou YN, Cheng HL, Wang CH. Energy requirements for ICU burn patients in whom the total body surface area affected exceeds 50 percent: a practical equation. Asia Pac J Clin Nutr. 2018;27(6):1182-189.
18. Güldoğan CE, Kendirci M, Tikici D, Gündoğdu E, Yastı AÇ. Clinical infection in burn patients and its consequences. 2017;23(6):466-471.
19. Becerril LC, Rojas AM, Gómez BA, Lourdes M, Hernández G. Importance of reflective and critical thinking in nursing. Rev Mex Enfermería Cardiológica. 2015; 23(1):35-41.
20.Marques RS, Zeitoun SS, Lara MR, Fernandes MS. Dimensioning of staff related to patient care using the critical Nursing Activities Score in the ways prospective and retrospective. J Health Sci Inst. 2013; 31(2):149-54.
21. Garcia TR. Systematization of nursing care: a substantive aspect of professional practice. Esc Anna Nery 2016;20(1):5-10.