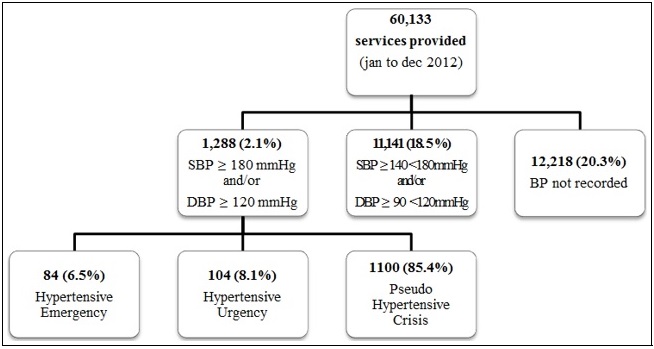
FIGURE 1: Flowchart of care services provided and distribution of patients, according to values of blood pressure and hypertensive crisis classification. Brazil, 2012.
ORIGINAL RESEARCH
Hypertensive crisis in patients at an acute care service: a retrospective study
Tamires Alessandra MineliI; Adrielle Naiara TonetiII; Daniel Martinez LanaIII; Victor Costa NogueiraIV; Leila Maria Marchi-AlvesV
I
Nurse. Master's Student, University of São Paulo. Brazil. E-mail: tamires.mineli@usp.br
II
Nurse. Specialist. Doctoral Student, University of São Paulo. Brazil.
E-mail: adrielle.toneti@usp.br
III
Physical educator. Specialist. Master's Student, University of São Paulo.
Brazil. E-mail: coach.daniellana@gmail.com
IV
Physical educator. Specialist. Master's Student, University of São Paulo.
Brazil. E-mail:
victor.costa.nogueira@hotmail.com
V
Nurse. PhD. Associate professor, University of São Paulo. Brazil. E-mail: lmarchi@eerp.usp.br
DOI: https://doi.org/10.12957/reuerj.2018.30111
ABSTRACT
Objectives: to characterize and identify the frequency of hypertensive crises (HCs) in patients at a health care service. Method: this retrospective, quantitative, descriptive study used data collected from 60,133 medical files of patients attending the emergency room of a healthcare plan provider in São Paulo state from January to December 2012. The study was approved by the research ethics committee. Results: 1,288 cases of HC (2.1%) were identified, 85.3% were characterized as hypertensive pseudocrises (HPCs), 8.1% as hypertensive crises and 6.5% as hypertensive emergencies. A significant number of records (20.3%) contained no record of blood pressure (BP) values. Conclusion: HPCs were the most frequent situation in the study population, but a large number of records with no BP measurement indicated the need for health professionals to be aware of morbid event prevention, identification and control of HCs, and the corresponding record keeping.
Descriptors: hypertensive crisis; blood pressure; hypertensive urgency; hypertensive emergency.
INTRODUCTION
Hypertensive crises (HC) are characterized by a sudden, inappropriate, intense and symptomatic rise of blood pressure (BP), with values going over 180/120 mmHg, with or without lesion of target organs1,2. It is estimated that this clinical condition is responsible for more than one-quarter of all services provided in medical emergencies3.
While acknowledging the importance of the topic and considering its high incidence in emergency services, this study tried to characterize and identify the frequency of services provided to patients with HC admitted in a private emergency care service located in the countryside of the state of São Paulo.
LITERATURE REVIEW
Some studies indicate that HC occur more frequently in Brazil in patients with a hypertension background4,5 and nearly 475,000 hypertensives are likely to have an HC every year in the country4.
The disease may appear as a hypertensive emergency or a hypertensive urgency, and this distinction is crucial in clinical practice for proper handling, with significant effects on morbidity and mortality6,7.
Hypertensive emergencies (HE) are characterized by a sharp rise in BP associated with progressive neurological, renal, ocular, or hepatic involvement, or myocardial failure, with immediate or potential life risk 7,8. In hypertensive urgencies (HU), symptoms are considered less severe, without evidence of recent involvement of target organ lesions, and therefore it can be treated within 24 hours7,9,10.
In addition to HE and HU, another condition often confused with HC can occur, which is known as pseudo hypertensive crisis (PHC), and its clinical evidence, regardless of blood pressure levels, is the absence of signs of acute target organ deterioration, without immediate life risk7,8. This condition is associated with BP rise and symptoms like headaches, dyspnea, atypical chest pain, panic syndrome and acute psychological stress7, often occurring in hypertensive patients who have abandoned treatment or who have not been followed up4,5,11.
Although these distinctions exist, the approach to HC remains controversial with regard to correct diagnosis, assessment difficulties, and the choice of an adequate treatment11,12. Moreover, incidence and prevalence of HC in representative populations are poorly addressed in the literature11.
METHOD
This is a quantitative, descriptive and retrospective study. Data were obtained from secondary sources by referring to medical records of patients who sought the services of a health care plan in the countryside of São Paulo, between January and December 2012. The company's headquarters cover five municipalities and a total of 80,000 customers. The population is served 24/7, with free access to other medical services of the city and region or by referral.
The medical records of patients aged ≥18 years cared for in emergency services within the data collection period were included in the study. HC cases were selected on the basis of care service records.
The sociodemographic identification of participants included the variables "gender", "age group", and "type of contract with the health plan provider", which were subject to validation of a service form. To characterize the situation and distinguish HE, HU or PHC, the records of a medical and nursing team in the care service form were checked, with the identification of BP values, diagnosis at admission and hypertension background, reports of lesions in target organs, life risk, description of signs and symptoms, treatment procedures, tests performed, referrals or outcome (death, hospitalization, observation, discharge).
Events in which patients had a record of a sudden and symptomatic BP rise, with systolic levels equal to or above 180 mmHg and/or diastolic levels equal to or above 120 mmHg, were characterized as HC1,8,13,14.
All cases in which the BP rise was associated with one or more types of severe lesion in target organs and imminent life risk, with necessary interventions to reduce BP and use of parenteral administration and ICU hospitalization were classified as HE. HU was defined as a BP rise without evidence of severe lesion in target organs, with remote life risk, with interventions to reduce BP within a few hours, use of oral or possibly parenteral medication and an eventual discharge with a possible period of observation. PHC cases included conditions of BP rise without signs of severe deterioration of target organs, without immediate life risk, associated with medication abandonment or emotional, painful or discomfort events, reversed with symptomatic medication and by reintroducing chronic anti-hypertensive drugs1,8,13,14.
Cases of abnormal rises in BP were also described, but with values that are lower than those of an HC, that is, systolic pressure ≥ 140 < 180 mmHg and/or diastolic pressure ≥ 85 <120 mmHg1,7.
The study was carried out according to the guidelines and regulatory norms of Human Research (Resolution 466/12 of the National Health Council) and approved by the Research Ethics Committee of the Ribeirão Preto College of Nursing at University of São Paulo, under protocol number 19546413.4.0000.5393.
Data were collected, processed with the help of the Statistical Package for the Social Sciences (SPSS), version 16.0 and submitted to a simple descriptive analysis with the calculation of absolute and relative frequencies. Results were presented by means of graphs and tables.
RESULTS
Out of the 60,133 care services provided in the period, HC was the clinical situation reported in 1,288 medical records (2.1%). The flowchart of care services provided and distribution of patients, according to values of blood pressure and hypertensive crisis classification is represented in Figure 1.
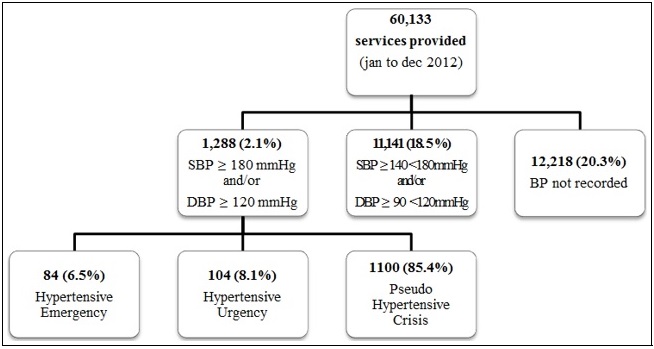
FIGURE 1: Flowchart of care services provided and distribution of patients, according to values of blood pressure and hypertensive crisis classification. Brazil, 2012.
A total of 18.5% of patients cared for in emergency services had changes in blood pressure levels, but they did not reach typical HC values. A significant number of medical records (20.3%) had no reports of BP levels, which may suggest that the number of patients with blood pressure changes can be higher.
The distribution of HE, HU, and PHC incidence according to gender, age group and type of contract is represented in Table 1.
TABLE 1: Incidence distribution of hypertensive emergency (HE), hypertensive urgency (HU) and pseudo hypertensive crisis (PHC), according to sociodemographic variables. Brazil, 2012. 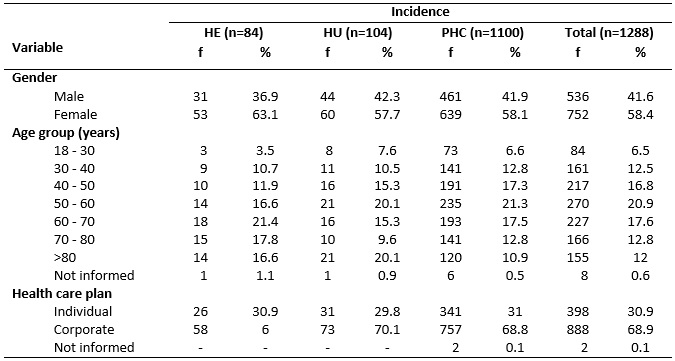
Most of HC care services (85.4%) were classified as PHC. The events which defined them as PHC were mainly related to pain, trauma, anxiety, and anti-hypertensive treatment abandonment.
As for HE, the most common diagnoses were myocardial infarction, acute pulmonary edema, and ischemic or hemorrhagic stroke. HUs included mainly cases of renal failure and pre- and postoperative events.
The main therapeutic conducts reported in medical records included the administration of medicine, performance of laboratory and electrocardiographic tests, referral to other professionals and hospitalization.
Considering the presentation of the clinical condition according to the time when the care service was provided, it is observed that between June and September there was a higher incidence of PHC cases, which were lower in the beginning and in the end of the year. Regarding HU cases, there was an increase in the number of services provided in May and November, with the lowest number in April. HE events took place mostly in June and September, with a decline in December. See Figure 2.
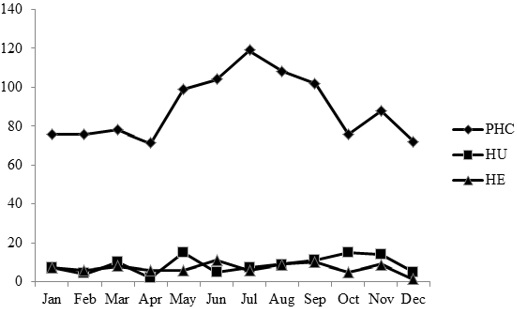
FIGURE 2: Number of medical services of Hypertensive Emergencies (HE), Hypertensive Urgencies (HU) and Pseudo Hypertensive Crises (PHC). Brazil, 2012.
DISCUSSION
Of all the services assessed, HC accounted for 2.1% of all services provided, with results similar to those of a study carried out in the state of São Paulo8,15.
The prevalence of women in HC care services in our study confirms current national5,16 and international studies17,18, emphasizing the positive association between women and the occurrence of cardiovascular complications.
The age group varied according to clinical manifestations, being lower in PHC cases, with individuals aged 18 to 29 years (86.9%). In HU, higher percentages were found (20.1%) for both people aged 50 to 59 and over 80 years. Patients in HE were mostly aged between 60 and 69 years (21.4%). Similar studies5,19 showed that the occurrence of HC is commonly found in individuals in their fifties, and it can be justified by the association between a linear increase of blood pressure and aging 7.
It was observed that most patients cared for in the surveyed service had a corporate health care plan (68.9%), justified by a high number of companies in the region. Currently, supplementary health has a significant demand in the country, with a greater concentration of individuals with a health care plan in the southeastern region (36.9%)20.
Most of HC care services (85.4%) were classified as PHC, followed by HU (8.1%) and HE (6.5%). As for the occurrence of HC according to the time when care was provided, PHC, HU and HE had a greater incidence in July, May and October, and June, respectively. A similar study in Brazil obtained similar results, with most events occurring in August (12.3%) and the lowest percentage in July (3.9%)16.
The high number of PHC cases has been reported in other studies 21-23, showing that this condition is often observed in urgency and emergency services, although it is underestimated because of the difficulties of an appropriate diagnosis16,21,24.
The main causes related to a PHC condition were pain, trauma, anxiety and non-adherence to treatment. In a follow-up study carried out in two hospitals, one public and one private, it was seen that 94% of patients with PHC were not treated accordingly, but rather if they were having an actual crisis instead, which could potentially lead to negative consequences, such as ischemia in noble organs21. A careful assessment of such cases, with targeted treatments, becomes essential to minimize harm to these patients11.
With regard to HC, HU was the most common condition in the population studied, and clinical conditions were associated with renal dysfunction and pre and postoperative periods. Some studies about HC manifestations in different populations found that HU cases stand out from HE ones, with a prevalence between 31% and 74.4%19,25,26.
HE cases accounted for only 6.5% of care services provided, with myocardial infarction, acute pulmonary edema, and ischemic or hemorrhagic stroke being the most frequent conditions which led to the search for immediate help. Similar results were observed in recent studies6,15, showing that the most common clinical manifestations behave in a similar manner in HE patients.
Generally speaking, the main therapeutic conducts found in medical records included the administration of drugs, performance of laboratory and electrocardiographic tests, referral to other professionals and hospitalization, therefore depending on patients' clinical condition. A recent review study found that, regardless of the HC subtype, its treatment is generally carried out in a very heterogeneous and empirical manner 6. We found that conducts seen in our study are in line with the recommendations of current Brazilian guidelines7.
Of the 60,133 care services provided, it was found that 12,218 patients (20.3%) did not have their BP reported in their medical records, which may have underestimated the percentage of patients with significant changes in blood pressure levels, which is an essential clinical reference for the assessment and choice of conducts.
Blood pressure reports in medical records were exclusively performed by the nursing team, and although it is not the objective of this study, it was observed that no report had information regarding the measurement technique or equipment used, limb, arm circumference, cuff size, patient position, among other relevant facts; therefore it did not comply with the national guidelines7.
Nurses' work in prevention, protection, and recovery of patients with HC is essential and comprehensive, and it includes the performance of BP checks with appropriate responses to pathophysiological manifestations, as well as nursing team coordination during care services10. Therefore, it is important to consider that the identification of needs and the implementation of a care plan are essential aspects for the systematization and organization of nursing emergency services27, in addition to the definition, improvement, and compliance with clinical protocols and therapeutic guidelines, ensuring patients with access and adequate treatment in a timely manner.
CONCLUSIONS
Results indicated that PHC was the most frequent situation in the studied population, followed by HU and a small share of HE, which is in accordance with other studies carried out in the country.
We can also highlight that blood pressure records were exclusively performed by a nursing team, which shows the potential of these professionals in the context of HC care. However, we must note that the identification of a significant number of pressure levels that were not recorded shows the need of awareness and appreciation of measurement and record of blood pressure levels, in order to identify and prevent morbid events and control hypertensive crises.
REFERENCES
1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003; 289(19):2560-72.
2.Suneja M, Sanders ML. Hypertensive emergency. Med. clin. n. am. 2017; 101(3):465-78.
3.Papadopoulos DP, Mourouzis I, Thomopoulos C, Makris T, Papademetriou V. Hypertension crisis. Blood. press. 2010; 19(6):328-36.
4.Nobre F, Ribeiro AB, Mion D Jr. Controle da pressão arterial em pacientes sob tratamento anti-hipertensivo no Brasil: controlar Brasil. Arq. bras. cardiol. 2010; 94(5):663-70.
5.Siqueira DS, Riegel F, Crossetti MGO, Tavares JP. Perfil de pacientes com crise hipertensiva atendidos em um pronto socorro no sul do Brasil. Rev. enferm. UFSM. 2015; 5(2):224-34.
6.Varounis C, Vasiliki K, Nihoyannopoulos P, Lekakis J, Tousoulis D. Cardiovascular hypertensive crisis: recent evidence and review of the literature. Front. cardiovasc. med. 2016; 3:51.
7.Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Nefrologia. VII Diretriz Brasileira de Hipertensão Arterial. Arq. bras. cardiol. 2016;107(3 Supl.3):1-83.
8.Martin JFV, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Perfil de crise hipertensiva: prevalência e apresentação clínica. Arq. bras. cardiol. 2004; 83(2): 1-14.
9.Johnson W, Nguyen ML, Patel R. Hypertension crisis in the emergency department. Cardiol. clin. 2012; 30(4):533-43.
10.Demézio DCS, Milhomes FF, Brasileiro ME. O enfermeiro frente à crise hipertensiva no atendimento de urgência e emergência. RECEEN. [Internet]. 2013 [cited 2018 Apr 08]; 4(4): 1-15. Available from: http://www.ceen.com.br/revistaeletronica
11.Yugar-Toledo JC, Cosenso-Martin LN, Vilela-Martin JF. Aspectos fisiopatológicos e clínicos das emergências hipertensivas. Rev. bras. hipertens. 2014; 21(3):140-7.
12.Monteiro-Júnior FC, Anunciação FAC, Salgado-Filho N, Silva GMA, Barbosa JB, Ferreira PAM, et al. Prevalência de verdadeiras crises hipertensivas e adequação da conduta médica em pacientes atendidos em um pronto-socorro geral com pressão arterial elevada. Arq. bras. cardiol. 2008; 90(4):269-73.
13.Feitosa-Filho GS, Lopes RD, Poppi NT, Gimarães HP. Emergências hipertensivas. Rev. bras. ter. intensiva. 2008; 20(3):305-12.
14.Hebert CJ, Vidt DG. Hypertensive crises. Prim. care. 2008; 35(3):475-87.
15.Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo AN, Yugar-Toledo JC. Hypertensive crisis: clinical-epidemiological profile. Hypertens. res. 2011; 34(3):367-71.
16.Lacerda IC, Veloso SDG, Souza ACC, Moreira TMM. Características da clientela atendida por crise hipertensiva na emergência de um hospital municipal de Fortaleza, Estado do Ceará. Acta sci., health sci. 2010; 32(1):73-8.
17.Saguner AM, Dür S, Perrig M, Schiemann U, Stuck AE, Bürgi U, et al. Risk factors promoting hypertensive crises: evidence from a longitudinal study. Am. j. hypertens. 2010; 23(7):775-80.
18.Salkic S, Batic-Mujanovic O, Ljuca F, Brkic S. Clinical presentation of hypertensive crises in emergency medical services. Mater. sociomed. 2014; 26(1):6-12.
19.Gasques JCP, Roland DMS, Cesarino CB. Caracterização da crise hipertensiva em pacientes de grupo de hipertensão de um ambulatório-escola. Rev. enferm. UERJ. 2008; 16(1):46-50.
20.Instituto Brasileiro de Geografia e Estatística [Internet]. Pesquisa Nacional de Saúde: 2013. 2015 [cited 2018 Jan 29]. Available from: http://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf
21.Sobrinho S, Correia LCL, Cruz C, Santiago M, Paim AC, Meireles B, et al. Ocorrência e preditores clínicos de pseudocrise hipertensiva no atendimento de emergência. Arq. bras. cardiol. 2007; 88 (5):579-84.
22.Barreto MS, Marcon SS. Hospitalização por agravos da hipertensão arterial em pacientes da atenção primária. Acta Paul. Enferm. (Online). 2013; 26(4):313-7.
23.Silva MAM, Santos ACS, Barbosa CF, Oliveira Filho CAS. Crise hipertensiva, pseudocrise hipertensiva e elevação sintomática da pressão arterial. Rev. bras. cardiol. 2013; 26(5): 329-36.
24.Reyes, S.F. Hipertensión arterial severa em urgências: una evaluación integral. Med. int. méx. 2014;30:707-17.
25.Merlo C, Bally K, Tschudi P, Martina B, Zeller A. Management and outcome of severely elevated blood pressure in primary care: a prospective observational study. Swiss. med. wkly. 2012; 142:w13507.
26.Al-Bannay R, Bohm M, Husain A. Heart rate differentiates urgency and emergency in hypertensive crisis. Clin. res. cardiol. 2013;102(8):593-8.
27.Governo do Distrito Federal (Br). Secretaria de Estado de Saúde. Programa de Educação e Controle de Hipertensão. Protocolo de enfermagem. Hipertensão arterial sistêmica. Brasília (DF); 2012 [cited 2018 Jan 09]. Available from: http://www.corendf.org.br/portal/images/pdf/Protocolo%20de%20Fluxo%20para%20Hipertens%C3%A3o%20Arterial.pdf