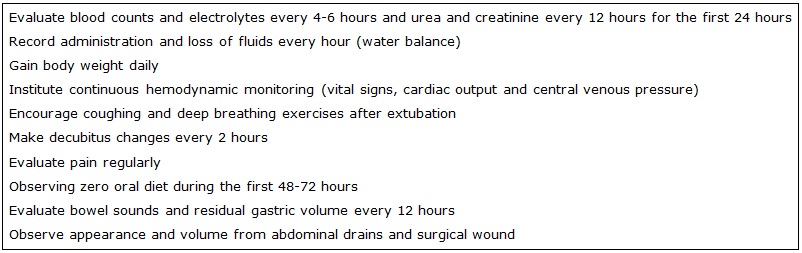
FIGURE 1: Postoperative nursing care for patients undergoing transoperative intraperitoneal hyperthermic chemotherapy
UPDATE ARTICLE
Intraoperative hyperthermic intraperitoneal chemotherapy: what nurses should know
Rafael Tavares JomarI; Laise da Silva SantosII; Márcio Francês ConteiroIII; Karen dos Santos MatsumotoIV; Cristiane Helena GallaschV; Gunnar Glauco de Cunto TaetsVI
I
Nurse. PhD in Public Health. AssistantProfessor. Rio de
JaneiroStateUniversity, NursingSchool. Rio de Janeiro, RJ, Brasil. E-mail: rafaeljomar@yahoo.com.br
II
Nurse. NationalCancerInstitute José Alencar Gomes da Silva, Hospital
ofCancer I. Rio de Janeiro, RJ, Brasil. E-mail: laise.santos@live.com
III
Nurse. NationalCancerInstitute José Alencar Gomes da Silva, Hospital
ofCancer I. Rio de Janeiro, RJ, Brasil. E-mail: marciomfc@globo.com
IV
Nurse. Master in Public Health. NationalCancerInstitute José Alencar Gomes
da Silva, Hospital ofCancer I. Rio de Janeiro, RJ, Brasil. E-mail: karenmatsumoto@gmail.com
V
Nurse. PhD in Nursing.Adjunct Professor. Rio de Janeiro StateUniversity,
NursingSchool. Rio de Janeiro, RJ, Brasil. E-mail:
cristiane.gallasch@gmail.com
VI
Nurse. PhD in Science. Adjunct Professor. Rio de Janeiro Federal
University, MacaéCampus. Macaé, RJ, Brasil. E-mail: masterufrj@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2017.29326
ABSTRACT
Objective: to present the current state of scientific knowledge about intraoperative hyperthermic intraperitoneal chemotherapy for the treatment of peritoneal carcinomatosis, and postoperative nursing care for patients undergoing this therapy. Methods: the study describes technical aspects of intraoperative hyperthermic intraperitoneal chemotherapy, the potential complications and post-operative nursing care involved. Results: emphasis was placed on the importance of nursing care, viz.: monitoring of vital signs, peripheral perfusion, cardiac output, and central venous pressure; pain assessment; encouraging coughing and deep breathing exercises; recording drainage of surgical wound and drains; investigating bowel sounds; measuring gastric residual volume; ensuring change of decubitus; evaluating laboratory blood test results; establishing water balance; and measuring body weight. Conclusion: intraoperative hyperthermic intraperitoneal chemotherapy has been shown to be a promising therapy in treatment of patients with peritoneal carcinomatosis. However, to be successful, the nursing care provided is fundamental.
Keywords: Chemotherapy, cancer, regional perfusion; nursing care; peritoneal cavity; postoperative care.
INTRODUCTION
Estimates for the Brazilian population point to 34,280 new cases of colorectal cancer, the second most common type of cancer among women and the third among men, in the biennium 2016-20171. In this epidemiological context, peritoneal carcinomatosis stands out as a condition associated with the unfavorable prognosis that may be present in the natural history of colorectal cancer and of some other cancers, such as peritoneal pseudomyxoma2,3.
Characterized by wide dissemination of carcinomas through the peritoneum2,3, peritoneal carcinoma secondary to conventional gastrointestinal neoplasms leads to a median survival of 5.2 months in advanced colorectal cancer and 3.1 months in advanced gastric cancer4.Until recently, conventional treatment consisted of systemic chemotherapy, or just palliative care. However, promising results have been reported following the implementation of radical cytoreductive surgery followed by transoperativehyperthermic intraperitoneal chemotherapy (HIPEC), which has prolonged survival and has improved the patients' quality of life2,5,6.
Considering the rapid technological development of cancer therapies that, in turn, require constant updating of nurses for a qualified clinical practice7,8, the objective of the present study was to present the state of scientific knowledge about HIPEC in the treatment of peritoneal carcinomatosis and the postoperative nursing care for patients submitted to this therapy.
Technical aspects and potential complications
As systemic chemotherapy has not demonstrated satisfactory results in the case of peritoneal carcinomatosis, most commonly originating from the spread of colorectal, gastric, uterine and ovarian cancers, the method of choice for its treatment is the radical cytoreductive surgery associated with HIPEC9-20, which limits the high concentrations of antineoplastic drugs to the peritoneal cavity thereby reducing systemic toxicity9,10,12,14,20.
The action of heat on HIPEC promotes greater efficacy of chemotherapeutic agents such as Doxorubicin, Cisplatin, Mitomycin C, Melphalan, Docetaxel, Irinotecan, and Gemcitabine11, since it potentiates their cytotoxic effects, including protein denaturation, induction of apoptosis and inhibition of angiogenesis9,10,15-17,20.
Under mechanical ventilation and general anesthesia, the patient undergoes a surgical incision extending from the xiphoid process to the pubis, followed by peritonectomy. After excision of macroscopic peritoneal tumors, the abdominal cavity is successively washed with saline solution. Thereafter, suction drains are placed to introduce and remove antineoplastic drugs, which should be at a temperature between 41°C and 43°C maintained by the infusion machine9-11,13-15,18,20.
Surgical smoke evacuators are placed around the abdomen to minimize the exposure of operating room personnel to aerosols from antineoplastic drugs. The surgeon regularly massages the outside of the abdomen, keeping the uniform distribution of the perfusate which is a mix of drugs with at least one liter of heated saline solution12,16. Cisplatin, Doxorubicin and Mitomycin C are the most commonly used drugs in HIPEC. Depending on the protocol, the surgery may lasts from 30 to 120 minutes9-11,16,20 .
Besides placing temperature probes inside the abdominal cavity for intraperitoneal temperature monitoring, esophageal or tympanic temperature, diuresis, hemodynamic and cardiopulmonary parameters are also continuously and carefully evaluated during the procedure9-11,16,20.At the end of HIPEC, the abdominal cavity undergoes extensive washes with saline solution and abdominal drains are installed to be maintained for at least two days in order to facilitate the drainage of residual fluids. Radical cytoreductive surgery followed by HIPEC may last from five to 13 hours 9-11,13,19,20 and the patient's stay in a postoperative intensive care unit for up to two days is recommended 9,12-14,19,20.
The most common complications of cytogenetic surgery combined with HIPEC are transient elevation of liver enzymes and serum creatinine levels, neutropenia and transient thrombocytopenia, fistula, anastomosis dehiscence, edema and surgical site infection. Other less frequent, but more serious, are ascites, gastrointestinal perforation, abscess or intrabdominal hemorrhage, pleural effusion, pneumonia, hypovolemia, sepsis and acute renal failure9-12,16,17,19,20.
Advanced age, extensive peritoneal carcinomatosis, surgical time greater than five hours and blood loss greater than 2.500 ml increase the risk of postoperative complications9-12,16,17. The presence of abdominal drains, not only cause pain - a common side effect - but also increases the risk of infection, intestinal perforation and the occurrence of fistulas. To prevent further complications, experts have recommend the adoption of infection control measures12.
Cytoreductive surgery combined with HIPEC may also lead to hemodynamic changes resulting from moderate blood loss. Although HIPEC alone does not alter the healing of the anastomosis, less collagen formation has been documented with administration of Mitomycin C and Cisplatin, which in turn increases the risk of acute renal failure10,20.
Postoperative nursing care
Patients submitted to HIPEC usually spend the immediate postoperative period in intensive care units, where surveillance is continuous 9,12-14,19-20.Therefore, nurses working in these units should be aware of the signs and symptoms resulting from the potential complications of HIPEC, so as to plan preventive care and optimize postoperative results 14,17.
As some complications of HIPEC are related to the transport of certain drugs to the systemic circulation, nurses should consider the possibility of potential hematological toxicity, and therefore evaluate laboratory blood test results every four hours during the first 24 postoperative hours 10,17. This is especially so when Oxaliplatin is used, because this drug increases the risk of bleeding, as well as the risk of acute renal failure10.Furthermore, electrolyte levels should be monitored every four to six hours and fluid administration/loss should be recorded hourly14,17. Water balance is therefore recommended.
Renal function should be rigorously evaluated with measurement of diuresis every one hour, as well as serum urea and creatinine titration every 12 hours, and body weight at every day14,17. Once Cisplatin has been used in HIPEC, Sodium Thiosulfate will be administered intravenously to control the nephrotoxic action of the metabolites of that drug. Both Cisplatin and Sodium Thiosulphate are eliminated via the renal route; thus optimum intravenous hydration and adequate urine production (200 ml/hour for the first 12 hours and 100 ml/hour for the following 12 hours) should be carefully maintained after administration10,14,17,19.
If urine production is inadequate despite the planned intravenous hydration, diuretic agents may be administered14,17, depending on the patient's cardiorespiratory state, which must be assessed by the nurse for signs of hemodynamic instability. Vital signs, peripheral perfusion, cardiac output and central venous pressure are therefore permanently monitored. In addition, edema and crackling lung sounds on pulmonary auscultation should be regularly investigated for signs of fluid overload17.
Patients undergoing cytoreductive surgery combined with HIPEC usually remain under mechanical ventilation for at least 12 hours due to the inflammatory response secondary to this therapy. After extubation, they are encouraged to cough and perform deep breathing exercises. Decubitation changes every two hours are also nursing care to promote proper ventilation. However, these changes can be challenging due to the presence of abdominal drains, the surgical incision itself and pain17.
Nurses play an important role in the control of pain secondary to the surgical removal of peritoneal tumors, since they are the professionals who regularly evaluate and administer the analgesics prescribed by the medical staff. Pain control optimizes airflow volume, deep breathing, and coughing, as well as improves early ambulation ability and deep breathing exercises. For about four to six days, epidural and intravenous analgesics are administered17,20. Another method used for pain control is patient-controlled analgesia, what can be instituted as soon as the patient is alert and able to activate the device12,17,19.
Nutrition is an essential component of nursing care provided to patients undergoing HIPEC. However, in order to reduce the risk of anastomotic leakage, nurses should observe the oral non-administration of nutrition9.Total parenteral nutrition is recommended as nutritional support until the second or third postoperative day due to gastroparesis, with indispensable maintenance of an enteral feeding tube until complete gastrointestinal recovery. Return of bowel sounds and low residual gastric volume are considered as indicators for the beginning of enteral feeding12,17. Therefore, nurses should investigate these signs at least every 12 hours.
Abdominal drains and wound dressing deserve special attention, with a record of their characteristics. The initial drainage flow rate can reach about 500 ml per day. Any drain with a flow rate greater than 100 ml in 24 hours should be maintained and its removal should be considered only when its content is purely lymphatic (citrus yellow). Bloody or frankly hemorrhagic drainage from the surgical wound or from drains should be immediately reported to the medical staff19.
In addition to the previously described care, as summarized in Figure 1, nursing professionals should pay attention to the appropriate excreta handling of the patient submitted to HIPEC in the last 48 hours. Properly dressed with a waterproof apron, procedure gloves, goggles and surgical mask, the professionals should carefully discharge excreta to avoid spilling, capping the toilet before flushing it down twice. Clothing contaminated with excreta or body fluids should be packed in an identified plastic bag and sent to the laundry room to be washed separately. Among other materials, gauze, diapers and gloves contaminated with excreta or body fluids should be discarded in a rigid, impervious container with a properly identified sealing cap21.
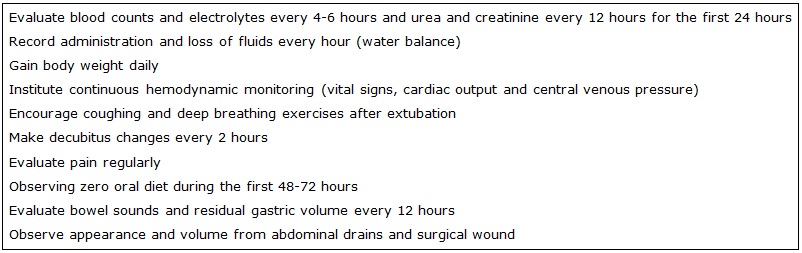
FIGURE 1: Postoperative nursing care for patients undergoing transoperative intraperitoneal hyperthermic chemotherapy
With the progressive expansion of the use of HIPEC, the issue of safety in the operating room cannot be overemphasized. This therapy exposes professionals to the potential contamination by antineoplastic drugs through the skin and the respiratory, digestive and ocular systems, in case of defective gloves, spills, aerosols or heating steam12,18. Therefore, it is recommended to exclude pregnant and breastfeeding women, women who wish to become pregnant or who have a history of spontaneous abortion from the HIPEC operating team. All people with a history of hematological disease or oncologic therapy or any other immunosuppressive therapy are also recommended to be excluded from the team18.
Further safety measures are recommended for the operating rooms where HIPEC is to be performed: surgical hoods, goggles, FFP3 masks and double impervious gloves must be used by the professionals present in the room 12,18; signs warning that HIPEC is in progress must be placed at the entrance of the dedicated surgical area; antineoplastic spill kit and rigid containers for properly labeled biological material must be available; surgical smoke evacuator during the procedure must be used; and triple wash of reusable surgical material with soap and water must be performed before referral for sterilization12.
The standard precautionary measures, including use of impervious aprons, procedure gloves, goggles and surgical mask, within 48 hours following the cytoreductive surgery combined with HIPEC is also recommended for all health professionals involved in the care provided to the patient submitted to this therapy.
Finally, it is worth emphasizing that the humanized and participative care, not only of nursing but of the entire healthcare team involved in patient care, from the receipt of the diagnosis of peritoneal carcinomatosis until the late postoperative period of HIPEC, is essential to support the patient in coping with cancer22.
CONCLUSION
HIPEC has proved to be a promising therapy in the treatment of patients with peritoneal carcinomatosis. However, for it to be successful, the provision of post-operative nursing care is fundamental, including: monitoring of vital signs, peripheral perfusion, cardiac output and central venous pressure; evaluation of pain; encouraging coughing and deep breathing exercises; record of drainage of surgical wound and drains; investigation of bowel sounds; measurement of gastric residual volume; promotion of decubitus change; evaluation of laboratory blood test results (blood count, electrolytes, urea and creatinine); water balance maintenance; and measuremente of body weight.
Since the planning, implementation, and supervision of evidence-based nursing care are essential, we suggest the realization of empirical nursing studies with patients submitted to HIPEC so as to improve the nursing care provided to this population.
REFERENCES
1.Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2016: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2015.
2.Rabelo FEF, Queiroz FL, Rego RSN, Costa BXM, Lamounier PCC, Oliveira TAN et al. Multimodal treatment of peritoneal malignancies - results of the implantation in a tertiary hospital. J Coloproctol (Rio J.). 2012; 32(2):106-12.
3.Lifante JC, Glehen O, Cotte E, Beaujard AC, Gilly FN. Natural history of peritoneal carcinomatosis from digestive origin. Cancer Treat Res. 2007; 134:119-29.
4.Segelman J, Granath F, Holm T, Machado M, Mahteme H, Martling A. Incidence, prevalence and risk factors for peritoneal carcinomatosis from colorectal cancer. Br J Surg. 2012; 99(5):699-705.
5.Kusamura S, Younan R, Baratti D, Favaro M, Gavazzi C, Deraco M. Cytoreductive surgery followed by intraperitoneal hyperthermic perfusion: analysis of morbidity and mortality in 209 peritoneal surface malignancies treated with closed abdomen technique. Cancer. 2006; 106(5):1144-53.
6.Sugarbaker PH. Five reasons why cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy must be regarded as the new standart of care for diffuse malignant peritonealmesotheliomia. Ann Surg Oncol, 2010;17(6):1710-2.
7.Souza MCF, Peres MAA, Martins GCS, Almeida-Filho AJ. Update of the professional habitusfrom the nurses at the National Cancer Institute(1980-1990).Texto contexto enferm. 2014;23(3):720-7.
8.AraújoCRG, Rosas AMMT, Menezes HF, Rodrigues BMRD. Teaching and learning in the gynecological brachytherapy nursing appointment: the nurses' perspectives. Rev enferm UERJ. 2016; 24(4):e18737.
9.Abu-Zaid A, Azzam AZ, AlOmar O, Salem H, Amin T, Al-Badawib IA. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for managing peritoneal carcinomatosis from endometrial carcinoma: a single-center experience of 6 cases. Ann Saudi Med. 2014; 34(2):159-66.
10.Halkia E, Kopanakis N, Nikolaou G, Spiliotis J. Cytoreductive surgery and HIPEC for peritoneal carcinomatosis. A review on morbidity and mortality. JBUON. 2015; 20 (Suppl. 1):S80-S87.
11.Winder T, Lenz HJ. Mucinous adenocarcinomas with intra-abdominal dissemination: a review of current therapy. Oncologist. 2010; 15(8):836–44.
12.Al-Quteimat O, Al-Badaineh M. Intraperitoneal chemotherapy: rationale, applications, and limitations. J Oncol Pharm Pract. 2014; 20(5):369-80.
13.Seidel GD, Locklin J, Muehlbauer PM. Part I: Regional chemotherapy clinical studies in nontraditional clinical settings. Clin J Oncol Nurs. 2006; 10(3):338-44.
14.Muehlbauer PM, Klapec K, Locklin J, George ME, Cunningham L, Gottschalk C, Seidel GD. Part II: Nursing implications of administering chemotherapy in interventional radiology or the operating room. Clin J Oncol Nurs. 2006; 10(3):345-56.
15.Arias F, Otero JM, Guerrero C, Cardona AF, Vargas CA, Carranza H et al. Pseudomixoma peritoneal: primeros casos tratados en Colombia con peritonectomía radical y quimioterapia intraperitoneal hipertérmica. Rev Colomb Cir. 2009; 24(3):184-94.
16.Sutton SW, Yancey LW, Chase VA, Hunley EK, McCarty TM, Kuhn JA, Loggie BW. Intraoperative modality of treatment for peritoneal carcinomatosis: use of hyperthermic interperitoneal chemoperfusion. Perfusion. 2002;17(6):441-6.
17.Mauricio RV, Green H, Hayes-Jordan A. Care of pediatric oncology patients after continuous hyperthermic peritoneal perfusion. Crit Care Nurse. 2010; 30(4):58-70.
18.Benoit L, Cheynel N, Ortega-Deballon P, Giacomo GD, Chauffert B, Rat P. Closed hyperthermic intraperitoneal chemotherapy with open abdomen: a novel technique to reduce exposure of the surgical team to chemotherapy drugs. Ann Surg Oncol. 2008; 15(2):542-6.
19.Gava VG, Balzan S. Cuidados perioperatórios em cirurgia citorredutora e quimioterapia hipertérmica intraperitoneal. Rev Med Res. 2013;15(4):293-7.
20.Carrillo-Esper R, Nava-López JA, Romero-Sierra G, Cáñez-Jiménez C. Manejo perioperatorio de la quimioterapia intraperitoneal hipertérmica. Rev Mex Anestesiol. 2014;37(3):193-200.
21.Instituto Nacional de Câncer José Alencar Gomes da Silva. Manual de boas práticas: exposição ao risco químico na central de quimioterapia: conceitos e deveres. Rio de Janeiro: INCA; 2015.
22.Gomes NS, Silva SR. Women's quality of life after breast cancer surgery. Rev enferm UERJ. 2016; 24(3):e7634.