REVIEW ARTICLE
Therapeutic efficacy of music: a transdisciplinary view of health for teams, patients and companions
Hermes de Andrade JúniorI
I Bassoonist. Doctor of Public Health (Phd). Senior Researcher. Center for Philosophical and Humanistic Studies. Catholic University. Portugal. E-mail: handradejunior@gmail.com
DOI: https://doi.org/10.12957/reuerj.2018.29155
ABSTRACT
Objective: to conduct a systematic review on the efficacy of music as therapy. Method: 404 articles written in Portuguese were identified by selected metadata in the Scielo Brazil and Portugal System; of those, 35 publications with results that discuss the benefits for actions in these countries, indexed from 2005 to 2016, were selected. Results: most of the studies were concentrated in the nursing field, with the articles originating in 15 professional disciplines. The main contributions and effects of music were: reduction of symptoms of discomfort, positive feelings, facilitation of personal and interpersonal communication, increased sociability of individuals, reduction of physical and mental pain, beneficial changes in physiological patterns, and bodily stimulus. Conclusion: music is a powerful transdisciplinary therapeutic resource for rehabilitation, and transcends models of health. It should not be denied to patients, their companions or even the team of health professionals caring for them.
Descriptors: Music therapy; transdisciplinarity; nursing; communication and public health.
INTRODUCTION
Music is an efficient non-invasive and non-painful treatment modality, unlike other medical techniques. With attention, its application has few or despicable side effects; the therapy is easily available to the patient, both in the hospital and in their home, allowing even their family (patient's companions) to take an active part in their treatment. All this without mentioning the economy of resources with certain therapies and with the hospitalization, when acting in a preventive and immediate way.
In terms of their practice, more evidence of benefits are found. The music exercise fosters cognitive progress, attention, memory, motor skill and creates unity between language, music, and movement. But the effect of this type of therapy goes beyond the use of music as a tranquilizer only for the patient. It serves the health professional and also the family or the patient's companion, categories that also interfere in the performance of the therapy.
For vulnerable patients, music softens the radical changes they face when they are hospitalized, the immense destabilizing factors to which they are subjected, from the new day-to-day rules to cohabitation with unknown people who have not chosen to share space and life, and above all the loss of ties with family, friends and neighbors.
Such examples affirm transdisciplinarity as a factor of technical applicability of music as therapeutic, since it brings together science, art and the sacred. The transdisciplinary approach inaugurates a new stage of history, surpassing the compartmentalized vision originated in scientism and scientific ideologies. His testimony places the quantum revolution as the central point of the desired transformations1.
The objective of this study was to carry out a systematic review on the effectiveness of music as a therapy in the context of Portuguese - speaking countries and to recommend their performance in a transdisciplinary way.
METHODOLOGY
The study carried out a bibliographic research in Scielo (Scientific Electronic Library Online) databases in Brazil and Portugal and the production of knowledge related to the effects of the use of music. Similar or correlated terminologies were considered2.
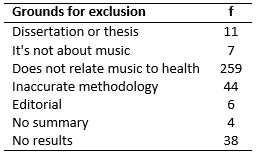
The inclusion criteria were for articles in Portuguese, between January / 2005 and December / 2016, which provided a summary; which included in their methodology projects, observational or experimental uses of music and musical intervention in some clinical situation; that cite objectives, consistent methodologies and results on the effects of music on the health of the public of the research, with date of publication. Exclusion criteria were for editorials, works without abstract, without results, dissertations or theses, those that did not deal with music, those that did not relate music with health and those with imprecise methodology, specified in Table 1.
TABLE 1:
Description of reason / number of jobs deleted. Publication period
2005-2016.
For the data collection of the articles a protocol was elaborated that included title, language, authors, specific area of the study, year of publication, published publication, clientele, sample, research objectives, results, type of intervention or observation, type of study, type of musical activity, music, subject participation, data collection instruments and final considerations.
The descriptors were used in the portuguese language, with reading of the abstracts of all the articles and the selection of those that fit the inclusion criteria, followed by the protocol created, analysis of the articles found, their results and comparison of the material obtained with the literature review. 404 articles were found. Of these, 369 were excluded because they did not meet the criteria. Thus, 35 articles that met the criteria were included in the study.
RESULTS AND DISCUSSION
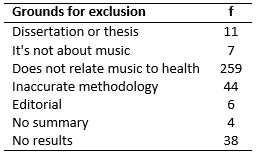
The distribution of the 35 articles identified 15 different professional areas and their interdisciplinarity (nursing, management, medicine, mental health and bioethics, letters / semiotics, physical education, medicine / pediatrics, communication, speech therapy, psychopathology, music, neuropsychology), highlighting studies in the nursing area with the highest number of publications involving the use of music according to Figure 1.
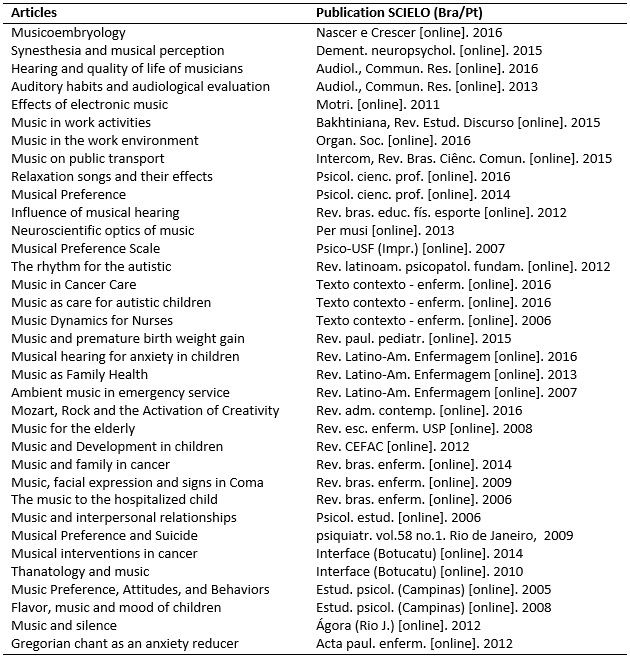
FIGURE 1:
List of articles included in the study by theme, year of publication and
source. Publication period 2005-2016.
Regarding the year of publication, 23 of the 35 articles selected referred to the period from 2012 to 2016, evidencing in recent years a growing concern of health professionals with the use of music as a tool and in their environment.
The diversity of articles, clientele and musical applicability are listed in Figure 2.
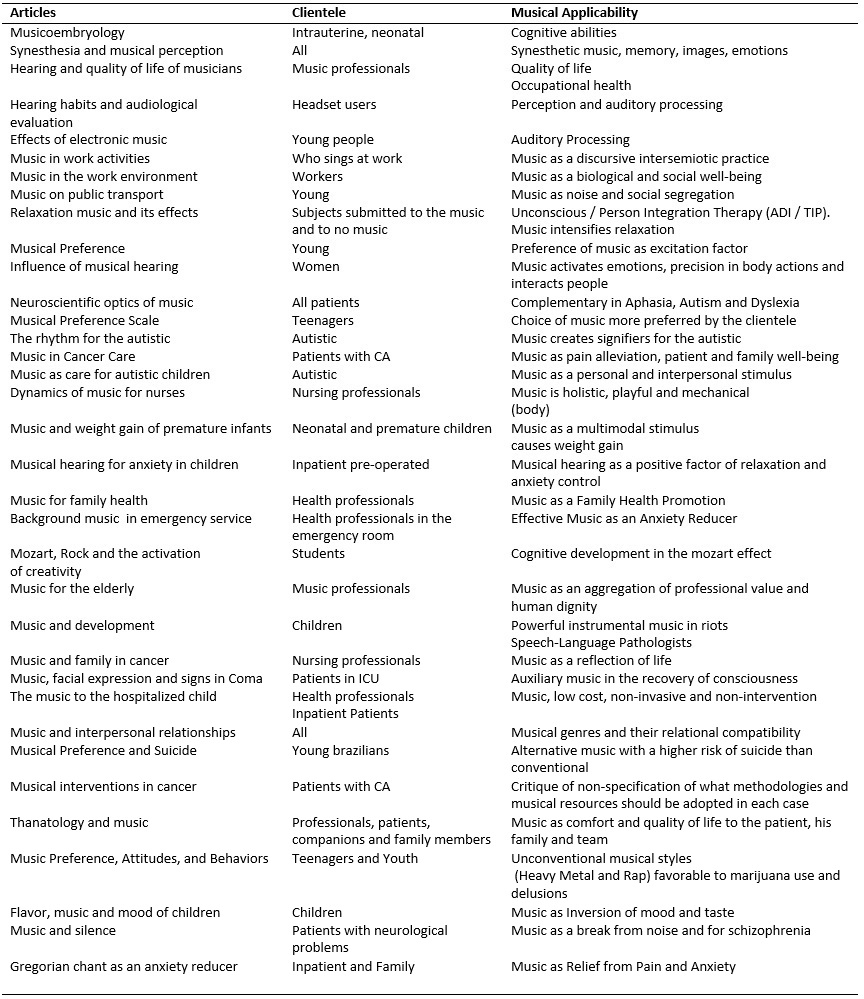
FIGURE 2:
Theme of the articles, clientele and musical applicability. Publication
period 2005-2016.
The contributions according to the reserved articles are analyzed below.
Music therapy as an intervention
Music has been used as a therapy since antiquity. Sounds and music manifest in many cultures to treat patients3,4 to this day. The music contributions, according to the reserved items are discussed below.
Marked from the old records, it becomes contemporary music therapy, which is based on scientific bases. However, since the time of Hippocrates, health literature has a skeptical attitude towards the therapeutic role of music, since the conceptual space for music as therapy seems to have been formed from philosophy and religion3-7.
In another view, music is not only an adaptive biological product of man to the world as a result of the process of natural selection, but a transformative technology: a cultural product with biological substrates that modifies the way we interact with the world and brings advantages to its users8.
In the last decades, many studies in neurosciences have shown that both instrumental music and songs are significant elements for the study of emotions, because they provoke responses with positive and negative valence, consistent even in individuals from different cultures. Activations were recorded in the amygdala, hippocampus, hippocampal gyrus, insula, temporal lobe and ventral striatum, among other brain regions 9-18.
Neuroscience shows that the brain of a long-term music practitioner, like that of professional musicians, functions in a different way from the brain of a non-musician. The first one presents greater capacity of learning, attention, concentration, emotional control and usually they are good humorous individuals. In developing their activities, such as performing a musical piece, they use both sides of the brain at the same time demonstrating developed musical abilities located in both hemispheres indicated by positively measurable changes19,20.
In children, music also exerts a great influence on its development and cerebral functioning, being understood by the brain as a form of language, since it involves different intonations, rhythms, movements and melodic contours used for communication and expression4,20.
From the conceptual point of view, music therapy can be understood as inherent to music itself in an objective, universal and independent way of context4, but it also rejects the definition of music as something objective and universal asserting that music would have potential for healing and could not be explained by cause-effect relationships or only by universal or metaphysical principles.
Health is a multifactorial phenomenon and music, one of these factors. Thus, music should be understood as something ambiguous and polysemic, that is: the meaning of music is constructed in a specific context, be it particular, local, regional or national. Social, cultural, therapeutic and personal aspects will always be able to influence the production and reception of music, understanding music as communication and social interaction7,4.
Music therapy as a relationship between the professional and the patient
If the meaning of music relates to a specific context, music therapy provides new possibilities for action7,21. Music therapy is a systematic process of intervention in which the therapist helps the client to promote health, through musical experiences and the relationship between both, as a dynamic force. An essential component in music therapy is the relationship between patient and therapist4. In this relationship, the therapist's ability to empathize with the client's condition is very important. It is a diverse and interactive space, where music is fundamentally a matter of musical experiences beyond a historical, cultural and universal phenomenon3,6. Some definitions of music therapy encompass aspects without direct therapeutic objectives 21. In fact, it is surprising that few definitions mention the term health focusing on outcomes such as well-being, self-actualization, reestablishment, while many describe outcomes due to illness rather than health, defining music therapy as treatment or rehabilitation for certain diseases, problems or needs21.
Music therapy for health professionals
Since 1980, there has been a tendency to organize all professional arts therapies in a single category and call the procedures that solved as alternative. It meant that the treatments offered by such professionals would be performed as substitutes for pharmacological treatments or used as a second option, in case traditional medicine failed22. Recently, the idea of alternative treatment has been replaced by that of complementary treatment, by allowing less usual therapies to be incorporated into traditional medicine, music therapy used together or as a complement to a specific treatment plan23.
The music therapist does not only work with the client, but with all systems 24 that relate to this. In this context, music becomes a social resource. The importance of the work of a multidisciplinary team is emphasized so that music therapy supplements and does not replace a treatment7.
In several clinical cases, it is necessary to cross the boundaries of your own discipline and establish a bridge to study phenomena that lie outside and beyond the scope of existing disciplines. Transdisciplinarity as a resource is not a new discipline, neither to the method (nor, therefore, to the transfer of the method), nor to the juxtaposition of knowledge that is part of an already existing discipline. It is rather a rigorous attitude towards everything that is found in space that does not belong to any discipline1,19.
Although the idea of the multidisciplinary team is unified in the applicability of music before these authors, it is worth emphasizing the transdisciplinary approach as the most adequate, since it results in the aggregation of integrated competences of all the knowledge for the therapeutics.
Music therapy as caring (patients, companions and family)
Music can be used in a psychotherapeutic process or in relaxation sessions, even at home, with positive effects. But as long as there is no qualified professional acting as a facilitator in the relationship between patient and music, this activity can not be considered music therapy24-26. We need the music therapist sees the whole of the patient 27, leading him to a meeting with himself, restoring its healthy part through music, which is understood in this process as a creative, private and beautiful. A global and holistic view of the patient enables a more focused approach to the care of the being, his abilities and potentials, instead of an intervention focused solely on the deficiencies arising from a certain pathology and that prioritizes only the healing of a weakness. Selected articles present music in the hospital context 28, where the client-therapist relationship is relatively brief and has secondary importance in relation to the medical procedure and the use of drugs29-33, whose treatment confers on the performance of nursing. It is believed that this is due to the fact that the nurse professional accompanies the performance of invasive and / or surgical procedures, which may be supported by musical applicability. We found publications by professionals from other areas with characteristics of the nursing praxis, confirming one of the studies28.
The experience of listening to music can focus on physical, emotional, intellectual, aesthetic or spiritual aspects and among the variations of the technique of musical hearing are musical anesthesia and musical relaxation. The first refers to the use of music to increase the effects of anesthetic and analgesic drugs, reduce or control pain and / or anxiety associated with pain; the second refers to listening to music to reduce stress, tension and anxiety and induce bodily relaxation28.
Music therapy and bioethics
We have a fear of how bioethics and music intertwine. However, respect for human dignity is one of the presuppositions of bioethics whose origin is linked to research practices with human beings carried out without respecting the dignity of man, his individuality and his own characteristics. Thus, Bioethics refers to practical ethics, which is concerned with right action. According to the principle of beneficence, health professionals seek the patient's good, health promotion and disease prevention. It refers to the action of doing good. The principle of non-maleficence is related to not causing harm to the patient. It is an abstention, a failure to do.
The thought of avoiding that music, in the clinical context of music as therapeutic, is an iatrogenic element, that is, that does not harm the patient is related to one of the principles of Bioethics, the principle of non-maleficence. Neglecting health care is an ethical issue of relevance that is supported by Bioethics and its principles, especially those of beneficence rather than maleficence.
But there is another problem that is tied to this principle of non-maleficence which is the omission of a doing, knowing that it is good for the cure and well-being of the patient. That is why musical knowledge applied to therapy should be taken seriously. Several evidences point to the noninvasive and painful therapy of music with the minimum of costs 29. So the big question for health follows: Why has music not been directly incorporated into the decalogue of medical ethics? Let us imagine that while a patient is being operated and sedated in addition to the proper instrumentation, resources and techniques, he receives music through his ears and that this happens in a protocolary way. Thus, music could, in fact, be the source of rehabilitation beyond an auditory experience or a sound stimulation of control, leading patients to complete restoration, in function of their natural responses of the body, heart and mind and still with transdisciplinarity as a methodological ally, helping in the greatest possible integration of treatment (or prevention, as the case may be). One study21 explains that such diversity is due to the existence of two guidelines in music therapy: the pathogenic and the salutogenic. According to the first, health is considered normal and ill-health, abnormal; according to the second, health and poor health are considered normal. In the pathogenic perspective, health is a state and in the salutogenic perspective, health is a continuous process of disease management.
Music therapy and its results
There is evidence of reduced discomfort symptoms30, positive sensations31, facilitation of personal and interpersonal communication32, increased sociability of individuals33, reduction of physical34 and mental pain 35, beneficial changes in physiological patterns36, and body stimulation37 with the use of music therapy. Most of the 35 articles examined show improvement in cognition (focusing on attention and concentration), physiological effects, reduction of anxiety in patients or their relatives. They report an improvement in the relaxation state of the research subjects in the general state of patients with mental illnesses of those under intensive treatment, as well as the unconscious ones. Children and the elderly are greatly benefited. Proportionally, 14.5% of studies indicate that music helps reduce anxiety; 31.7% recommend the use of music as a nursing intervention; 18.4% conclude that music acts on physiological responses; 12.4% referred to music as a viable alternative for sedative and anxiolytic use; 17.9% conclude that music helps reduce pain but 3.2% reported that there were no significant results for customers regarding the use of music. In several studies, more than one variable was observed acting in concomitance30-37.
Concerning the participation of the research subject, only three works highlight the active client during the musical intervention. In general, it is known that research subjects tend to have a passive attitude, since almost in their entirety the studies are conducted by professionals who are not qualified to the transdisciplinary treatment of music. The specialized professional to act with music in health controls tasks of creating, composing and improvising musically with the subjects, taking them to a positive and dynamic attitude towards the stimuli. He has the knowledge and mastery of music as an element of work30,38, marking the transdisciplinary requirement for health in the sphere of action, which goes beyond prescribing and delivering the most appropriate music developing a musical experience for all dimensions of the holistic being.
The explanation that music has the potential for healing is embedded in a multifactorial phenomenon7,39 and is satisfactory so that more training areas in the concentrations of studies found (at least 15) tend to merge to act with music, which is at the heart of the transdisciplinary nexus.
The applicability of the music in its complexity forces the nexus independently of the case of health in focus, which also by this tool tends to complement31,39. It is worth to mention, while a sedated patient is being operated on, in addition to the appropriate instrumentation, resources and techniques, he must witness the music and this must be promoted in a protocolary way by a professional - a clinical being, but with musical knowledge.
CONCLUSION
The findings confirm the effectiveness of music as therapeutic and that, in order to reach the goals mentioned through music, professionals sometimes not musicalized use the resources they have basing their practice on the specific knowledge of their area of formation.
However, musicalization itself and the knowledge of related areas (for forms, genres, styles, performances and technology and musical management to control the environments and materials of exposure, for example) confirm the need for transdisciplinarity as an attribute of their professional training and of the field of music as a working tool.
Thus, music could, in fact, be the source of rehabilitation beyond an auditory experience or a sound stimulation of control, leading patients to complete restoration, in function of their natural responses expressed in body, heart and mind. It is characterized the merger in the clinical sphere, which will have the security of prescribing the musical tool as the most appropriate therapy and supported by literature.
It is questioned if the music should have a therapeutic role of short duration in relation to the treatment and also secondary in importance. There is concern about the use of solid musical tools. A consistent methodology is effective and amenable to performance evaluation, characterizing its strength in therapeutic action in conjunction with musical genre, materials or techniques.
Music is a powerful therapeutic transdisciplinary resource for rehabilitation that transcends health models. It should not be denied to patients, their companions and even the team of health professionals who assist them. It is hoped that the present study may help in the understanding of professional performance and of its competence in the field of music, promoting transdisciplinarity in the context of the health area, valuing bioethics. It is necessary to include music as complementary therapy in the professional training in health and in offering assistance to clients.
REFERENCES
1.Martin V. Transdisciplinarity revealed what librarians need to know. Santa Barbara (CA): ABC-CLIO; 2017.
2.Sampaio RF, Mancini MC. Systematic review studies: a guide for judicious synthesis of scientific evidence. Rev. bras. physioter. 2007; 11 (1): 83-9.
3.Gouk P. Introduction in musical healing in cultural contexts. Brookfield (VT): Ashgate Publishing Co., 2000; 1-25.
4.Wigram T, Pedersen IN, Bonde LO. A comprehensive guide to music therapy: theory, clinical practice, research and training. Philadelphia (USA): JK Publishers; 2002.
5.Cuervo L. Joints between music, education and neurosciences: ideas for higher education. In: 7 Symposium on Cognition and Musical Arts. Brasília (DF): 2011.
6.Horden P. Music as medicine: the history of music therapy since antiquity. Aldershot: Ashgate; 2000.
7.Ruud E. Music therapy: a perspective from humanities. New Hampshire (IL): Barcelona Publishers; 2010
8.Patel AD. Music, language, and the brain. New York (USA): Oxford Univ. Press; 2008.
9.Brattico E, Alluri V, Bogert B, Jacibsen T, Vartiainen N, Nieminen S, Tervaniemi M. The functional MRI. study of happy and sad emotions in music with and without lyrics. Frontiers in Psychology. 2011; 2 (308): 1-16.
10.Fritz T, Jentschke S, Gosselin N, Sammler D, Peretz I, Friederichi AD, et al. Universal recognition of three basic emotions in music. Curr. Biol. 2009; 19 (7): 573-6.
11.Gosselin N, Peretz I, Johnsen E, Adolphs R. Amygdala damage impairs emotion recognition from music. Neuropsychology. 2007; 45 (2): 236-44.
12.Gosselin N, Peretz I, Hasboun D, Baulac M, Samson S. Impaired recognition of musical emotions and facial expressions following anteromedial temporal lobe excision. Cortex. 2011; 47 (9): 1116-25.
13.Koelsch S, Fritz T, Cramon D, Muller K, Friederici A. Investigating emotion with music: an fMRI. study Hum. Brain Mapp. 2006; 27 (3): 239-50.
14.Koelsch S. Toward a neural basis of music perception - a review and updated model. Frontiers in Psychology. 2011; 2 (110): 1-20.
15.Mitterschiffthaler M, Fu C, Dalton J, Andrew C, Williams S. A functional MRI. study of happy and sad affective states evoked by classical music. Hum. Brain Mapp. 2007; 28 (11): 1150-62.
16.Omar R, Henley S, Bartlett JW, Hailstone JC, Gordon E, Sauter DA, et al. The structural neuroanatomy of music emotion recognition: evidence from frontotemporal lobar degeneration. Neuroimage. 2011; 56 (3): 1814-21.
17.Samson S, Ehrle N, Baulac M. Cerebral substrates for musical temporal processes. Ann.NY.Acad. Sci. 2001; 930: 166-78.
18.Wong P, Ciocca V, Chan A, Ha L, Tan L, Peretz I. Effects of culture on musical pitch perception. PlosOne. 2012, 7 (4): 1-8.
19.Travis F, Harung HS, Lagrosen Y. Moral development, executive functioning, peak experiences and brain patterns in professional and amateur classical musicians: interpreted in light of a unified theory of performance. Consciousness and Cognition. 2011; 20 (4): 1256-64.
20.Aamodt S, Wang S. Welcome to the brain of your son. São Paulo: Cultrix; 2013.
21.Bruscia KE. Defining music therapy. 3rd ed. University Park (IL): Barcelona Publishers; 2014.
22.Lima VO. The effect of interactive musical activities on the well-being of children with urogenital changes during hospitalization for surgery [master's dissertation]. São Paulo: University of São Paulo; 2015.
23.Bradt J. Guidelines for music therapy practice in pediatric care. Gilsum (NH): Barcelona Publishers; 2013.
24.Hintz M. Guidelines for music therapy practice in developmental health. Gilsum (NH): Barcelona Publishers; 2013.
25.Bergold LB, Lima R, Alvim, NAT. Musical encounter: strategy of nursing care in chemotherapy to discuss illness / death. Rev. enferm. UERJ, 2012; 20 (2): 758-63.
26.Campos NL Fields, KantorskiI, LP. Music: opening new frontiers in nursing care practice in mental health. Rev. enferm. UERJ, 2008; 16 (1): 88-94.
27.Zanini CR, Jardim PC, Salgado CM, Nunes MC, Urzeda FL, Carvalho MV, et al. The effect of music therapy on quality of life and blood pressure in hypertensive patients. Arq. Bras. Cardiol., 2009; 5 (93): 534-40.
28.Bruscia KE. Case studies in music therapy. Barcelona (Es): Barcelona Publishers; 2006.
29 Effects of music and music therapy on blood pressure: a review of the literature. Rev. of the Nucleus of Studies and Interdisciplinary Researches in Music Therapy 2014; 5 (5): 37-57.
30.Paiano da Silva LAG, Baran FDP, Mercês NNA. Music in caring for children and adolescents with cancer: integrative review. Texto contexto - enferm. [online]. 2016; 25 (4): E1720015.
31.Nunes-Silva M, Valadares ACD, Rosa GT, Lopes LCM, Marra CAS. Evaluation of composite music for induction of relaxation and its psychological effects. Psicol. cienc. prof. [online]. 2016; 36 (3): 709-25.
32.Franzoi MAH, Santos JLG, Backes VMS, Ramos FRS. Musical intervention as a strategy of nursing care for children with autism spectrum disorder in one center of psychosocial care. Texto contexto - enferm. [online]. 2016; 25 (1): e1020015.
33.Ilari B. Music, social behavior and interpersonal relationships. Psicol. study [online]. 2006; 11 (1): 191-98.
34.Seki NH, Galheigo SM. The use of music in palliative care: humanizing care and facilitating farewell. Interface (Botucatu) [online]. 2010; 14 (33): 273-84.
35.Lima CM, Poli MC. Music and a little silence: from the voice to the subject. Ágora (Rio de Janeiro) [online]. 2012; 15 (nspe): 371-87.
36.Auto FML, Amancio OMS, Lanza FC. Effect of music on the weight gain of premature infants over 32 weeks: randomized clinical trial. Rev. paul. pediatr. [online]. 2015; 33 (4): e293-9.
37.Rodrigues NS, Coelho Filho CAA. Influence of musical hearing in the practice of physical exercises by adults. Rev. bras. educ. phys. sport [online]. 2012; 26 (1): 87-95.
38. El-Aquar WA, Vasconcelos CRM, Veiga Neto, AR. Quality of work life and music in the industrial working environment. Organ. Soc. [Online]. 2016; 23 (79): 656-74.
39.Wheeler B. Music therapy handbook. New York (USA): Guilford Publications; 2016
Referência incompleta