ORIGINAL RESEARCH
Safe opioid analgesic therapy dose scheduling for burn patients: a cross-sectional study
Danielle de Mendonça HenriqueI; Lolita Dopico da SilvaII; Flavia Giron
CameriniIII; Karla Biancha Silva AndradeIV; Sandra Regina Maciqueira
PereiraV; Cintia Silva FassarellaVI
INurse. PhD in nursing. Adjunct Professor, Faculty of Nursing, State University of Rio de Janeiro. RJ, Brazil. E-mail: danimendh@gmail.com
IINurse. PhD in nursing. Adjunct Professor, Faculty of Nursing, State University of Rio de Janeiro. RJ, Brazil. E-mail: lolita.dopico@gmail.com
IIINurse. PhD in nursing. Adjunct Professor, Faculty of Nursing, State University of Rio de Janeiro. Brazil. E-mail: fcamerini@gmail.com
IVNurse. PhD in nursing. Coordinator of the Intensive Care Center of the National Cancer Institute. Rio de Janeiro, RJ, Brazil. E-mail: k.biancha@ig.com.br
VNurse. PhD in nursing. Adjunct Professor, Faculty of Nursing, State University of Rio de Janeiro. RJ, Brazil. E-mail: sandregina@gmail.com
VINurse. PhD in nursing. Adjunct Professor, Faculty of Nursing, State University of Rio de Janeiro. RJ, Brazil. E-mail: cintiafassarella@gmail.com
DOI:
http://dx.doi.org/10.12957/reuerj.2017.28082
ABSTRACT
Objectives: to describe opioid therapy in analgesia for burn patients, and to
identify drug interactions in the scheduling process, thus contributing to
prevention of respiratory depression. Methods: this
retrospective study examined 272 medical records of burn patients
hospitalized between 2011 and 2013. Naloxone administration, blood pressure
lower than 110/60mmHg, orotracheal intubation, pulse oximetry less than
90%, respiratory rate less than 10 bpm, need for oxygen, and abrupt opioid
discontinuation. Results: analgesia was predominantly with
the opioids: tramadol (45.49%) and methadone (18.45%). Predominant
administration times were 10pm and 6pm. There was potential for drug
interactions in 66.6% of the cases, while 88.8% of the drug pairs studied
can cause severe harm. Conclusion: when scheduling the
prescribed medication, nurses should be aware that inappropriate opioid
dose scheduling may lead to drug interaction, potentiating pharmacological
effects, with the risk of loss of consciousness and respiratory depression.
Keywords: Critical care; analgesia; respiratory insufficiency; patient safety.
INTRODUCTION
Burns are traumatic wounds caused in most cases by thermal, chemical,
electrical or radioactive agents. According to data from the World Health
Organization1 (WHO), about 300,000 people die each year from
burns worldwide, and millions of people suffer from disfigurement and
dysfunction caused by scars, psychological trauma and significant loss of
economic productivity. According to the Brazilian Society of Burns (BSB),
one million cases occur each year in Brazil, of which 200 thousand are
treated in emergency services and 40 thousand require hospitalization 2.
Opioid analgesics are the most commonly used for the treatment of burn
pain. Factors that justify the choice for this drug class include potent
analgesia; pharmacokinetic profile (ease of absorption, distribution and
excretion); variety of administration routes; and also the promotion of a
certain degree of sedation, depending on the dose administered, which may
be particularly advantageous during burn-care procedures3.
Opioids are considered to be potentially dangerous drugs (PDD), as they
have the potential to cause harm to patients, even when used as intended.
The Institute for Safe Drug Practices (ISDP) reports that although errors
in the use of these drugs are not common, the impact on patients when they
occur can be severe and may even lead to death4.
The wide spectrum of opioids available for clinical use confers flexibility
of dosage, since its pharmacological presentation allows the administration
by different routes (oral, enteral, rectal, subcutaneous, intravenous,
epidural, transdermal and by inhalation), offering different possibilities
for the treatment of pain in burned patients. However, this variety also
suggests a higher risk when it comes to drug safety4.
Among the effects associated with the use of opioids, the most serious is
respiratory depression (RD), which is considered an adverse event and
usually preceded by excessive sedation. Given the severity of this event,
preventive measures have been discussed in different patient safety forums 5.
In high complexity units such as the Treatment Center for Burn Patients
(TCBP), nurses are responsible for the release, preparation and
administration of opioids by different routes. Thus, it is the
responsibility of nurses to evaluate the medications based on
pharmacological knowledge, evaluating the possibility of drug interactions
that may potentiate the effect of opioids and favor the occurrence of RD.
After administering an opioid, nurses should not only monitor the effects
of the drug on the patients, but also the appearance of possible events
that may predict RD.
All these aspects involving the use of opioids were the basis of this
research whose objectives were to describe the opioid therapy used for
analgesia in burn patients and identify drug interactions, based on errors
in the process of hospitalization, contributing to the prevention of RD.
LITERATURE REVIEW
Burns are classified according to depth of the burn and the body surface
affected. Burn pain is related to these factors; the deepest are classified
as third degree burns and may involve destruction of the afferent nerve,
theoretically reducing the pain in the site, although in clinical practice,
this is not always a reliable indicator6.
It is of the utmost importance that the burn victims be constantly
evaluated for pain in order to guide the analgesic conduct and the response
to medication. Features such as site of the pain, factors of improvement or
worsening, type and intensity of pain are also essential to management.
Opioids are analgesic drugs commonly used for treatment of moderate to
highly intense pain3.
Analgesia with opioid drugs should be individualized, considering the
clinical conditions of the patients, the intensity of pain, the efficacy of
the response to analgesia after careful administration of the drug, and the
presence of undesirable effects. Thus, knowledge on pharmacokinetics is
fundamental, since the absorption, distribution, metabolism, and excretion
of opioids can be altered7.
The combined use of medications for the purpose of additive or potentiated
analgesia with lower individual doses and reduction of undesirable effects
is a common practice in the treatment of pain, especially burn pain. This
practice, although widely used, may favor drug interactions and alter the
pharmacokinetics of opioids8.
In order to avoid drug interactions, nurses should be able to relate
pharmacodynamic and pharmacokinetic characteristics of the drugs to the
possibility of adverse events resulting from the use of opioids. It is
necessary to recognize as early as possible the main signs to be monitored
after administration of opioids, besides identifying those patients at
higher risk for RD9.
Safe use of opioids, associated with nursing actions, involves the
medication process, patient monitoring and recognition of predisposing
factors for RD. Nurses have the responsibility for the implementation of
barriers to prevent RD in burned patients using opioid drugs9.
METHODOLOGY
A retrospective study was carried out in the first semester of 2014. A
total of 272 medical records of burned patients hospitalized between 2011
and 2013 were analyzed at the Treatment Center for Burned patients (TCBP)
of a federal public hospital in the municipality of Rio de Janeiro.
Complete medical records were selected, with discharge or death as outcome,
of patients with a minimum length of stay of 48 hours, aged over 18 years,
who used opioids through different routes of administration, monitored with
pulse oximetry, and without a ventilatory prosthesis.
RD episodes were screened in the medical records that met the selection
criteria, , which confirmed at least two indicators, among them:
administration of Naloxone, blood pressure less than 110/60mmHg,
orotracheal intubation, pulse oximetry less than 90%, respiratory rate less
than 10 breathing cycles per minute (bcpm), need for oxygen supply, and
abrupt opioid interruption.
In order to achieve the objectives proposed by the research, the following
variables were analyzed: drugs used in the analgesia of the burned
patients, pattern of drug release, and the occurrence of drug interaction.
The identification and classification of the drug interaction was performed
by Micromedex software10.
The medical records that met the selection criteria were divided into two
groups. The group G1 corresponded to patients who presented RD and the
group G2 to patients without RD. The variables were submitted to
descriptive and inferential statistics, and a 95% confidence interval was
calculated for the calculation of p-values using the Fisher's Exact Test.
Association measures such as Odds Ratio (OR) and Relative Risk (RR) were
also used.
The study project was submitted to institutional approval by means of a
letter authorizing the research, and by the Research Ethics Committee (REC)
of the institution, obtaining approval by the consubstantiated Opinion of
REC - nº 453.911/2013, on November 11, 2013.
RESULTS
A total of 272 medical records of burned patients hospitalized between 2011
and 2013 were analyzed, but only 42 medical records met the selection
criteria of the study, and from these, 12 (28.58%) presented 24 episodes of
RD. In the 42 medical records analyzed, 255 doses of prescribed analgesics
were identified, and all drugs were classified according to the Anatomical Therapeutic Chemical (ATC) classification system.
Among the analyzed doses, opioid analgesics predominated in the groups with
and without RD. Among opioids, the most noteworthy were tramadol, 116
(45.49%), and methadone, 47 (18.43%). Among the available benzodiazepines,
only diazepam (n = 27) was used and its ratio was similar between the
groups with and without RD. Among the tricyclic antidepressants, imipramine
predominated; and among anticonvulsants, gabapentin was more frequently
used by patients who did not present RD.
In order to aid the analysis of the management of the analgesic therapy, it
was necessary to identify how nurses organize the timing of this therapy in
the release of the prescribed drugs to the burned patients.
It was observed that in both groups, with and without RD, there was a
predominance of release at 22h and 06h, but inversely. In the group of
patients with RD, the predominant time, with the highest concentration of
medications, was 22h.
The concentration of release at the abovementioned hours has the
consequence of potential drug interaction (PDI). Thus, the association
between exposure to PDI and occurrence of RD was the tested.
Patients who were exposed to PDI due to the mode of medication release are
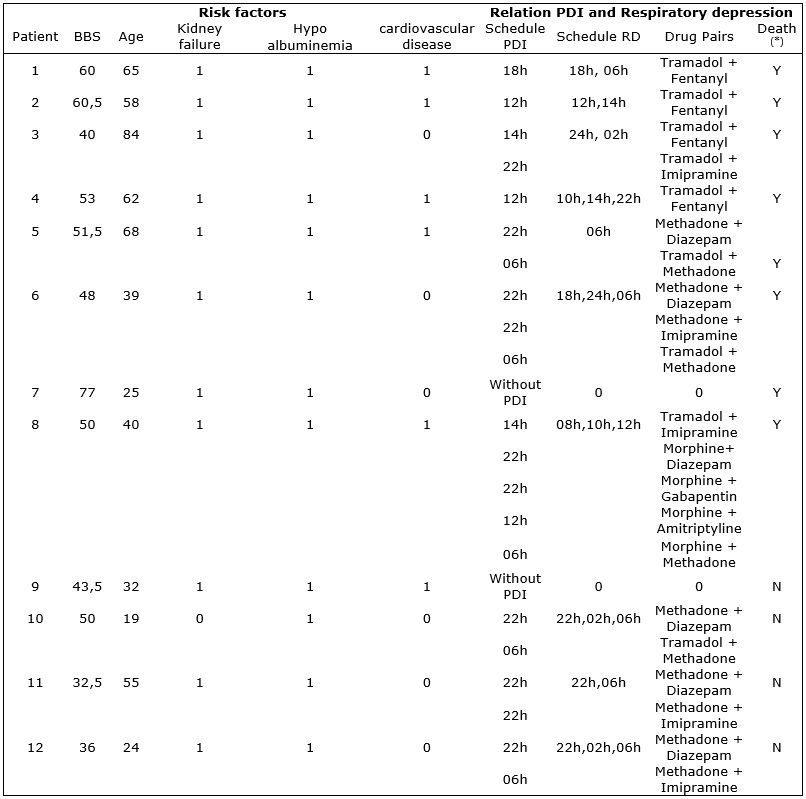
listed in the Figure 1, with the respective variables of interest for the
research.
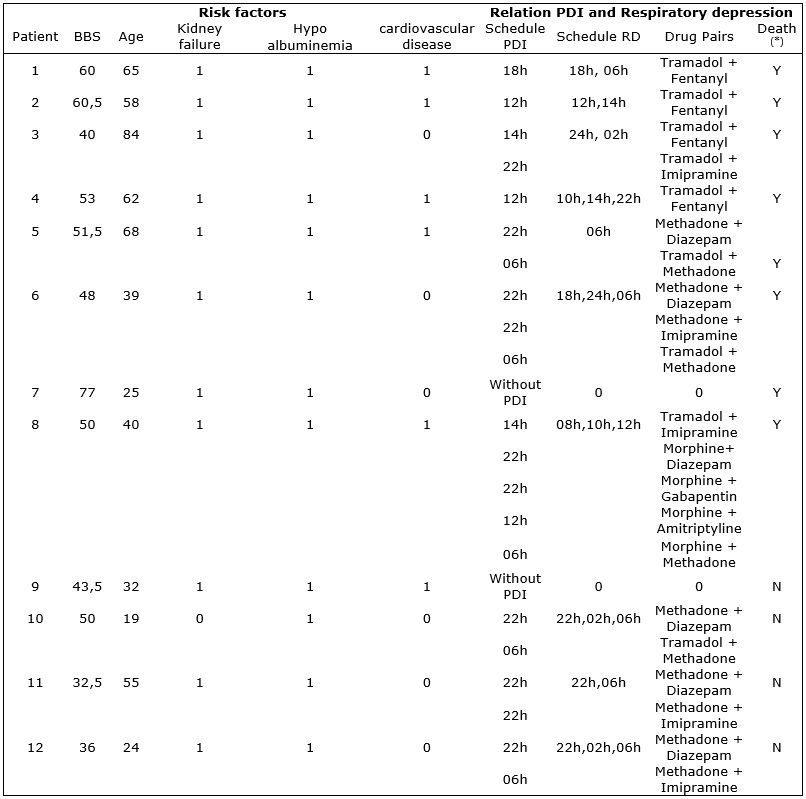
Legend: Respiratory depression (RD); Burn Treatment Center (BTC); Burned
Body Surface (BBS); Potential Drug Interaction (PDI).
Note: (*) Death - Y = yes and N = no.
FIGURE 1
: Overview of patients with RD in whose prescriptions were identified PMIs.
Rio de Janeiro, 2014.
The Figure 1 presents an overview of the patients who had RD according to
the burned body surface (BBS), occurrence of predominant risk factors for
RD, PDI schedule, RD schedules, drug pairs involved in the PDI, and the
occurrence or not of death.
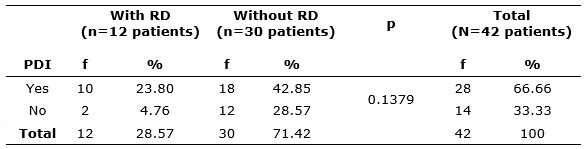
Although no significant difference (p-value = 0.1379) was found between the
two groups, the OR and RR were calculated and showed a positive
association. There was a three-fold greater chance of RD in patients with
PDI and a 2.5-fold increased risk of RD in these patients. See Table 1.
TABLE 1:
Distribution of the occurrence of PDI in patients with and without
respiratory depression. Rio de Janeiro, 2014.
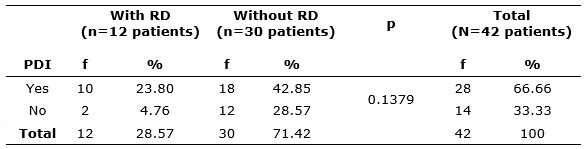
Legend: respiratory depression (RD); Potential drug interaction
Note: Fisher's exact test (CI: 95%).
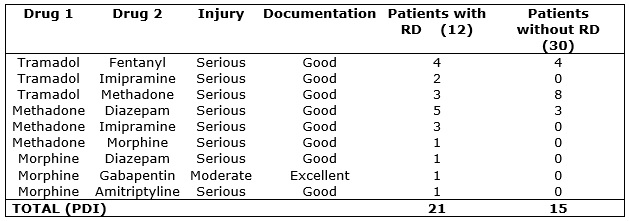
The drug pairs involved in PDI, their classification as to severity and the
level of evidence of these drug interactions, in the prescriptions released
in the TCBP, in patients with and without RD, are described in Figure 2.
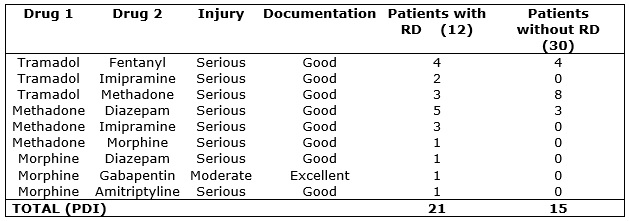
Legend: respiratory depression (RD); Potential Drug Interaction (PDI).
Source: Micromedex6.
FIGURE 2:
Pairs of drugs involved in Potential Drug Interactions. Rio de Janeiro,
2014.
It is observed that in the pairs of drugs studied, the number of PDIs (21)
was higher in the 12 patients with RD, whereas in the 30 patients without
RD, 15 PDIs occurred, as detailed in Figure 2.
In the studied TCBP, the pairs of prevailing drugs with PDI in patients
with RD were methadone with diazepam (n = 5) followed by tramadol with
fentanyl (n = 4), methadone with imipramine and methadone with tramadol
(3). See Figure 2.
In the group without RD, PDIs occurred in the cases of administration of
methadone with tramadol (n = 8), tramadol with fentanyl (4), and methadone
with diazepam (3). The most prescribed drugs also appear among the
prevalent involved in PDI, as it is the case of tramadol, methadone and
diazepam.
Regarding the severity of the PDIs, the data show that, in TCBP studied,
there was a predominance of associations that induce serious damage.
Regarding the documentation of PDIs, most are good; only the association of
tramadol with imipramine was weak. See Figure 2.
The study indicates that patients with a median burned body surface (BBS)
of 50%, and of age 47.5% have severe RD. The prognosis of younger patients
was better, eight out of12 patients with RD died; among the four survivors,
the younger ones predominated, with a mean age of 32.5 years, and the
oldest of the survivors had the lowest BBS. See Figure 1.
Another factor that should be considered is the occurrence of risk factors
for RD due to opioids. Renal failure was identified in 11 (91.6%) of the RD
patients, cardiovascular diseases in 6 (50%) and all had hypoalbuminemia,
which is characterized as a typical condition of burned patients and favors
the possibility of RD.
We observed that 10 (83.33%) individuals with RD presented PDI, with a
predominance of the 22h and 06h schedules. The drugs of higher interaction
were methadone with diazepam and tramadol and fentanyl, which were
administered through oral, intravenous and transdermal routes. The PDI
schedules were close to the registered RD schedules.
The drug with the highest number of prescribed doses was tramadol. This
drug is, therefore, more likely to cause PDI. On the other hand, despite
having a lower number of prescribed doses, morphine offers a greater risk
of RD.
Proportionally, it was observed that from the 38 doses of tramadol
prescribed in patients with RD, PDI was identified in eight cases. In turn,
morphine was used in only one patient who had RD, and all the four
administered doses had PDI.
DISCUSSION
In this research it was evidenced that the analgesic therapy of burn
patients is performed through different drug classes, with opioids as the
basis of this treatment; still, tramadol and methadone were the drugs most
used in the studied population.
Analgesia with opioids should be individualized. The clinical conditions
and intensity of pain of the patient, the effective response to analgesia
after careful administration of the drug, and the possible presence of
undesirable effects should be considered. Thus, knowledge on
pharmacokinetics is fundamental, because the absorption, distribution,
metabolism and excretion of opioids can be altered11.
Hypermetabolism in burned patients, which occurs in the first 24 to 48
hours after the burn, causes an increase in extracellular fluid volume,
causing possible changes in glomerular filtration. These characteristics
may alter the pharmacokinetic and pharmacodynamic response of opioids,
potentiating or reducing their effects on burned patients12,13.
The combined use of drugs for the purpose of obtaining additive or
potentiated analgesia with lower individual doses and reduction of
undesirable effects is a common practice in the treatment of pain,
especially burn pain14. This explains the use of different drug
classes in this study.
Besides opioids, other medications such as gabapentin are used. The latter
is an anticonvulsant, but is currently also prescribed for the management
of neuropathic pain. There is evidence that this drug assists in the
reduction of pruritus in the epithelization phase of burns15,16.
Benzodiazepines have no analgesic properties and should not be used as
such, but are useful and effective in reducing the perception of pain in
anxious patients. Antidepressants, such as amitriptyline and imipramine, in
low doses, have a comfirmed role in the management of neuropathic pain 15-17. Nurses need to have specific pharmacological knowledge to
contribute to the prevention of adverse events of opioids18.
In this study, tramadol and methadone were the most evident in the
treatment of burned patients. Nurses should be able to administer such
drugs, identify their pharmacological properties and expected therapeutic
effects, basing their conducts on this knowledge18.
It is understood that when nurses manage the drug therapy of burned
patients, they should monitor them during and after drug administration and
recognize early side effects of each drug in order to evaluate intervention
measures.
Regarding the profile of the release and PDI in the pharmacological therapy
in burn patients, 66.66% of drug interactions in this study were identified
as resulting from errors in drug release. At the moment of scheduling the
administration of opioids, nurses should be aware of the pharmacodynamic
characteristics of the drug, ensuring the efficacy of the analgesia and
avoiding PDIs.
The pharmacokinetics of opioids may be altered by drug interactions,
particularly by hypnotic-sedatives, antipsychotics, and monoamine oxidase
(MAO) inhibitors19,20.
According to the search conducted in Micromedex®10, drug
interactions capable of causing RD were identified and they are considered
serious. Drug interactions should be known by nurses, so that they can be
avoided by delaying a prescription, contributing to the prevention of
adverse events related to drug therapy21.
The times of administration of drugs in the night shift – 22h and 06h –
predominated in both groups of patients, with and without RD. There were no
doses released at odd hours. The hours of drug release depend on the
organization of the service in the sector, since the bath of burned
patients and dressings are performed in the morning.
The organization and execution of drug release in the studied site appear
to be strongly adapted to the institutional routine, being an activity that
seems to receive little attention. Although knowledge is fundamental to
avoid PDIs that can harm patients, there is an organizational logic in
which nursing professionals follow standardized schedules without taking
into account the possibility of drug interactions22.
Safe and accurate release of medication is an important responsibility of
nursing professionals, who still perform it manually in most hospitals,
following a fixed schedule routine that rarely considers the
characteristics of the prescribed medication and/or the clinical situation
of the patient, and this is the reality of the field of this study. Through
drug release, nurses organize the drug therapeutic plan established for the
patients and, in most hospitals, the pattern of time intervals is closely
associated with the routine of nursing care, of doctors, and of the
pharmacy service23.
In intensive care units, such as the TCBP, the prescriptions contain
increasingly complex combinations, making it very difficult to foresee
PDIs, which are those in which there is a possibility of changing the
effect of the drugs involved and may lead to undesirable results,
increasing the incidence of adverse effects of therapy without concomitant
therapeutic benefit23.
Although their results may be both positive (increase in effectiveness) and
negative (decrease in effectiveness, toxicity or idiosyncrasy), PDIs are
usually unplanned and undesirable in pharmacotherapy. Results have shown
that complications related to medication use are the most common type of
adverse event in hospital admissions (19% of patients), and that 2-3% of
the hospitalized patients experience reactions specifically provoked by
pharmacological interactions23.
In this study, the most prevalent drug pairs related with PDIs were
methadone with diazepam, tramadol with fentanyl, methadone with imipramine,
and methadone with tramadol. It is recommended that the preparation of the
medications be carried out in a safe environment, and that this environment
be the one in which nurses will release medication, so that the
professional may be able to consult tables and protocols, simple and
practical resources to inform about the more common PDIs with intravenous
drugs22.
Diversifying the schedules may be a strategy to reduce PDIs. We suggest the
use of odd hours for drug release. Although the literature does not
specifically address how medication timings should be distributed 4-24, the need to alternate opioid schedules with drugs that
potentiate their effects, such as benzodiazepines, for example, was evident
in this study.
Perhaps the ideal to avoid a drug release that can provoke PDI is the
computerized prescription that guides the drug release. Several softwares
that were exclusively developed for the purpose of checking the possible
interactions between drugs are already available in the market, but they
are not always within the reach of the nursing team, in their work places.
Furthermore, the use of computerized drug prescription systems, when
coupled with specific databases and specific calculators, enable physicians
to instantaneously receive useful warnings about drug interactions when
they are prescribing the drugs, preventing a drug release schedule that
could cause a drug interaction. However, this tool still has some obstacles
to be overcome, because of its high costs and the need for a reasonable
infrastructure and training of the health team, a fact that explains the
slowness of its implementation in the hospital system23.
The occurrence of a severe PDI due to a routine of drug release should be
considered by nurses a mistake to be prevented. Errors should serve as
tools to promote the quality of the service provided, foster changes in
institutional and professional culture, encourage non-punitive attitudes,
enable corrections to the system's flaws, and ensure greater patient safety 24.
CONCLUSION
This study identified that the pharmacological treatment of burned patients
involves different drug classes. Yet, the basis of the treatment are
opioids, evidenced by the predominance of the number of doses of these
analgesics in both groups with and without RD. Tramadol and methadone are
the most commonly used opioids.
In this sense, it is necessary for nurses to acquire knowledge about the
potential effect of opioid therapy on excessive sedation and RD, so as to
be able to recognize adverse drug reactions such as early identification of
the progression of sedation and the importance of making timely adjustments
in the care plan.
We recommend that health institutions create and implement policies and
procedures for continuous clinical monitoring of patients receiving opioid
treatment.
Most medical records contained data that, after analysis, indicated the
PDIs. Patients with PDI presented a three-fold greater chance of RD. Undue
drug release may contribute to the occurrence of drug interaction, and this
interaction, in turn, may potentiate the pharmacokinetic and
pharmacodynamic effect of the drug and, in the cases of patients taking
opioids, this may lead to a decrease in the level of consciousness and RD.
We hope that this study advance the Brazilian scientific production on the
topic of drug safety, fostering new studies in this area,
generating knowledge and data source for consultation of health
professionals, because RD caused by the use of opioids is an extremely
serious adverse event, which should be the focus of discussion of the
entire multidisciplinary team, generating safe assistance processes.
REFERENCES
1.World Health Organization. Burn prevention: success stories and lessons
learned. Geneva: World Health Organization, 2011. [cited in Jul 05, 2016].
Available from:
http://apps.who.int/iris/bitstream/10665/97938/1/9789241501187_eng.pdf
2.Takino MA, Valenciano PJ, Itakussu EY, Kakitsuka EE, Hoshimo AA, Trelha
CS, et al. Epidemiological profile of children and adolescents victims of
burns admitted to a burn treatment center. Rev Bras Burns. 2016; 15 (2):
74-9.
3.National Network for Burn Care. National Burn Care Referral Guidance. UK:
NHS Specialised Services, 2012. [cited in 2017 Jan 17]. Available from:
britishburnassociation.org/referral-guidance
4.Institute for Safe Medication Practices. Potentially hazardous drugs for
hospital and outpatient use - updated lists 2015: ISMP; 2015. [cited
January 17, 2017]. Available from:
http://www.ismp-brasil.org/site/wp-content/uploads/2015/12/V4N3.pdf
5.Kraychete DC, Siqueira JT, Garcia JB. Recommendations for the use of
opioids in Brazil: Part II. Use in children and the elderly. Rev Dor.
2014;15(1):65-9.
6.Richardson P, Mustard L. The management of pain in the burns unit. Burns.
2009; 35(1): 921-36.
7.Lemonica L. Pharmacological basis for the clinical use of opioids. Rev
Hospital practice. 2008; 10 (56): 1229-35.
8.Bolgiani AN, Serra MCVF. Update on the local treatment of burns. Rev Bras
Queimaduras. 2010; 9 (2): 38-44
9.Henrique DM, Silva LD. Respiratory depression as a complication of opioid
use: grounding the nursing care. Evidentia. 2014; 11 (1): 47-8
10.Micromedex 2.0. Truven Health Analytics, Inc. Greenwood Village, CO.
[cited in 2017 Jan 17]. Available from: http://www.micromedexsolutions.com
11.Cavalcanti VL, Barcelos LS, Cavalcanti RLS. Knowledge of nurses in the
control of burn pain in burned patientS. Magazine presença. 2016; 2 (5):
25-41
12.Henrique DM, Silva LD, Pereira SEM. Characteristics of burned patients,
opioid user, and factors contributing to respiratory depression. Enfermería
Global. 2016; 15 (43): 112-25.
13.Trupkovic T, Kinn M, Kleinschmidt S. Analgesia and sedation in the
intensive care of burn patients: results of a european survey. J Intensive
Care Med. 2011; 26(6):397-407.
14.Lima LS, Correia VOS, Nascimento TKGO, Chaves BJP, Silva JRS, Alves JAB
et al. Profile Of Burn Victims Attended By An Emergency Unit.
2017;10(10):1-9.
15.Richardson P, Mustard L. The management of pain in the burns unit.
Burns. 2009; 35(1): 921-36.
16.The Joint Commission. Safe use of opioids in hospitals. Sentinel Event
Alert, Issue; 2012. p.49. [cited in 2017 Jan 12]. Available from:
http://www.jointcommission.org/assets/1/18/SEA_49_opioids_8_2_12_final.pdf
17.Castro RJA, Leal PC, Sakata RK. Pain treatment in burn patients. Rev
Bras Anestesiol. 2013; 63 (1): 149-58.
18.Pinho FM, Amante LN, Salum NC, Silva R, Martins T. Guideline of actions
in nursing care to adult burned patients. Rev Bras Queimaduras.2016; 15
(1): 13-23
19.Institute of Healthcare Improvement. Campaign of 5 million lives,
preventing damage caused by high-risk drugs. 2008 [cited in Feb. 20, 2017].
Available from:
http://www.ihi.org/IHI/Programs/Campaign/
20.Katzung BG. Farmacologia básica e clínica. 9ª ed. Rio de Janeiro:
Guanabara Koogan; 2006.
21.Henrique D.M, Silva, L.D. Safe use of opioids in burned patients:
grounding the nursing care. Rev Bras Burns. 2014; 13 (1): 6-10. [cited in
Jan. 12, 2017]. Available from:
http://www.rbqueimaduras.com.br/detalhe_artigo.asp?id=190
22.Camerini FG, Silva LD. Patient safety: analysis of the preparation of
intravenous medication in a sentinel hospital. Text Context Enferm. 2011;
20 (1): 41-9.
23.Silva LD, Matos GC, Barreto BG, Albuquerque DC. Drug release by nurses
in sentinel hospital prescriptions. Texto contexto enferm. 2013; 22 (3):
722-30
24.Lima CSP, Barbosa SFF. Occurrence of adverse events as indicators of
quality of care in an intensive care unit. Rev Enferm UERJ.2015; 23 (2):
222-8.