ORIGINAL RESEARCH
Patients' perceptions of health care-related infections and safety measures
Miriam Cristina Marques da Silva de PaivaI; Cristiane Helena
GallaschII; Silvana Andrea Molina LimaIII; Lucy
Sitton-KentIV; ReenaDeviV; Andreas XyrichisVI
I
Nurse. PhD, State University of São Paulo, Botucatu, São Paulo, Brazil.
E-mail: miriampaiva@fmb.unesp.br
II
Nurse. PhD, University of the State of Rio de Janeiro, Brazil. E-mail:
cristiane.gallasch@gmail.com
III
Nurse. PhD, State University of São Paulo, Botucatu, São Paulo, Brazil.
E-mail: smolina@fmb.unesp.br
IV
Nurse. PhD, University of Nottingham, England. E-mail:
lucy.sitton-kent@nottingham.ac.uk
V
Psicologist. PhD, University of Nottingham, England. E-mail:
reena.devi@nottingham.ac.uk
VI
Nurse. PhD, King's College London, England. E-mail: andreas.xyrichis@kcl.ac.uk
VII
Funding source: products resulting from a research project with support
from the British Academy through the Newton FundMobility Grant.
DOI:
http://dx.doi.org/10.12957/reuerj.2017.27468
ABSTRACT
Objectives:
to analyze data from qualitative studies of patient perceptions of measures
to prevent and control healthcare-related infections and factors that
contribute to their own safety. Method: systematic review
of publications from 2006 to 2016, followed by thematic synthesis by coding
patients' accounts and interpretations of findings given. Results: six themes highlighted barriers to patients'
participating actively in promoting their own safety: insufficient
information supply; poor comprehension; negative feelings; negative
experiences; behavior of health care personnel; and factors that influence
patient involvement. Conclusion: the gap between patients'
understanding infection prevention and control measures and their becoming
involved in the process point to a need for measures to foster effective
communication, better care personnel-patient relations, and access to
information that encourages patients to interact and contribute to health
care.
Keywords:
Cross infection; health promotion; patient safety; active patient
participation.
INTRODUCTION
Scientific and technological progress have provided valuable resources for
diagnosis and treatment of diseases and recovery of health, but various
devices and procedures, such as insertion of central and urinary catheters,
are often associated with infections and influence care outcomes 1. The burden of health care-related infections (HCRI) is high
in developed countries2, but such rates are up to 20 times
higher in developing countries, and the proportion of infected patients
reaches frequencies above 253.
In an effort to prevent and control HCRI, researchers have sought to
provide and synthesize recommendations on procedures, resources, and
management that can serve as guides for the health staff4,5.
However, infection prevention and control (IPC) continue to pose challenges
for health systems; innovative researches that promote better care outcomes
are still desired1.
National Patient Safety Programs valuing patients as the center of care and
their involvement in safety actions were listed by the World Health
Organization among the solutions to improve the process of health care and
to contribute to risk reduction and patient safety6,7.
The participation of patients as promoters of health care changes requires,
however, the training of individuals, families and the community, aiming to
promote their empowerment and collaboration with health care professionals1. In this sense, it is necessary to explore the level of
understanding of patients about safety measures in HCRI prevention and
control to propose and/or promote their participation8.
Motivated by the need to know the advances of research on actions to
promote the involvement of patients in safety measures for HCRI prevention
and control and encouraged by national and international recommendations,
the following questions was selected for this: What are the patients'
perceptions about HCRI prevention and control and patients' contributions
to their own safety in this area? What are the main research findings in
this topic?
In this context, the present study aims to analyze qualitative studies
about patient perception of prevention and control measures of health
care-related infections and factors that contribute to patient safety.
METHODOLOGY
This is a systematic review of qualitative studies. Qualitative researches
were chosen because a qualitative approach seeks to explore the way people
understand the world around them, who they are, and how they present
themselves and respond to others9, and these issues are not
easily elucidated with an experimental methodology10. The
thematic synthesis described by Thomas and Harden was chosen due to its
potential to facilitate the formulation of appropriate and effective
policies and practices. In this method, the goal is to preserve an explicit
and transparent relationship between the conclusions and the text of
primary studies11.
The searches ran from October 2016 to February 2017, using the Virtual
Health Library (VHL), Cumulative Index to Nursing and Allied Health
Literature (CINAHL), Embase, United States National Library of Medicine
(Pubmed), Scopus, and Web of Science. The inclusion criteria used were:
articles published between January 1, 2006, and December 31, 2016, in
Portuguese, English or Spanish. The exclusion criteria were: articles not
available in full length, with exclusively quantitative analysis, repeated
publications, and literature reviews. As search strategies, we used the
Descriptors in Health Sciences - DeCS and the Medical Subject Headings -
MeSH: (Infecção hospitalar AND Pacientes AND Pesquisa qualitativa);Cross infection AND Patients ANDQualitativeresearch; and Infecciónhospitalaria AND Pacientes AND Investigacióncualitativa; and in the CINAHL
database, HAI AND Patient AND Perception AND Qualitativeresearch.
For selection of articles, the relevance of the works was analyzed by
reading of titles, and then reading the abstracts and/or the full texts.
The selected articles were independently assessed by two reviewers before
inclusion in the review. Each selected article had the following data
collected: title, authors, year of publication, country of study, research
team, objectives, participant subjects, methods of data collection and
analysis, study site and results. The results of each article were coded
line by line and then the relationships between them were identified. Codes
with similar meanings were grouped to create a synthesis with categories
that converged in broad descriptive themes. This material was critically
analyzed and interpreted by the authors, who answered the study question by
the abstraction of the themes and presented a synthesis and implications
for the development of interventions11.
As this study did not involve humans, the study did not require approval
from Research Ethics Committees.
RESULTS
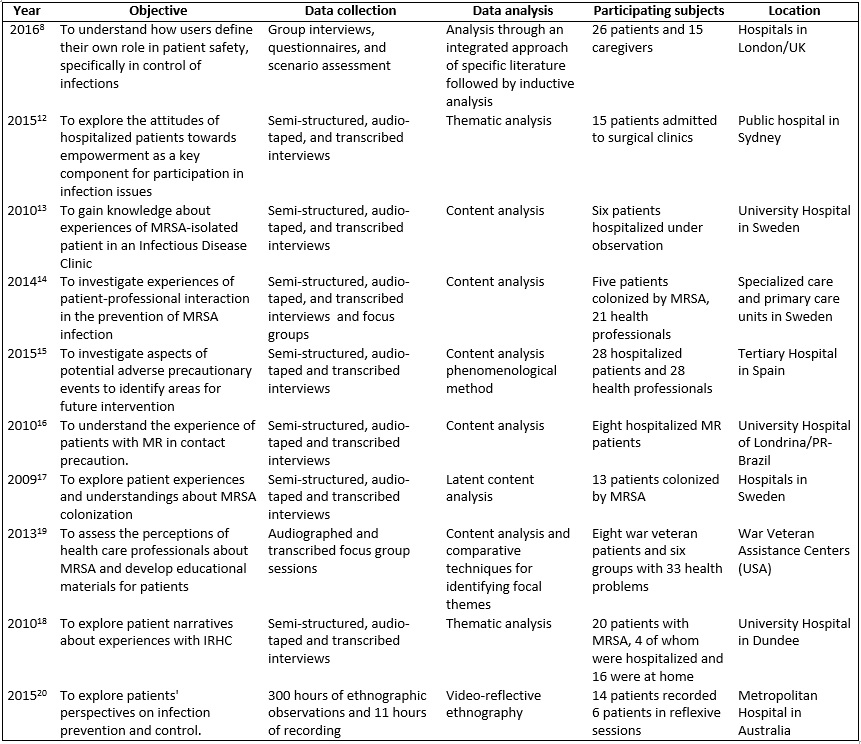
Four hundred and seventy six publications were identified: 121 in the VHL;
161 in CINAHL; 41 in Scopus; 120 in Pubmed; 22 in Web of Science; and 11 in
Embase. Ten studies stood out for examining the patients' perceptions about
measures related to HRCI after application of pre-established criteria. In
order to preserve the context of the studies, an individualized summary is
presented in Figure 1.
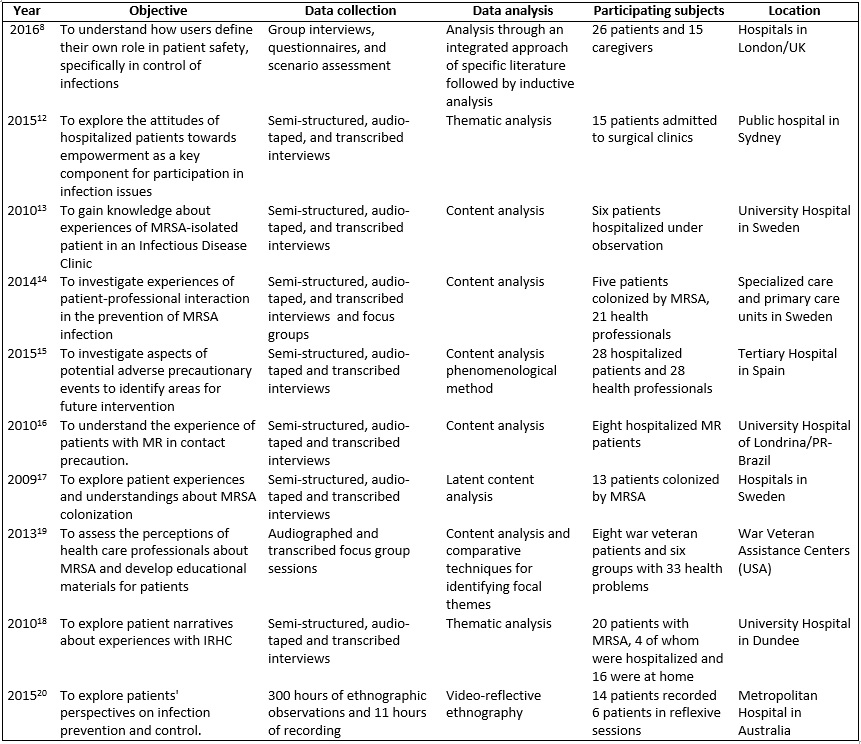
(*) MRSA: Methicillin-resistant Staphylococcus aureus. (**) MR: multiresistant microorganism. (***) IRHC: Infections related to health care
FIGURE 1:
Articles collected in databases on patient perceptions of health
care-related infections. 2009/2016.
Two articles deal specifically with HCRI from the point of view of patient
involvement as a safety measure8,12. Seven studies addressed
HCRI and multiresistant bacteria. For data collection, most of the studies
used semi-structured interviews; one used a focus group with patients;
another used a set of methods; and another, observation and video-tapes. As
for method of analysis, six articles used content analysis 13-17,19, two used thematic analysis12,18, one study
used inductive analysis8, and one performed reflective video
ethnography20.
Six themes emerged from the texts analyzed, revealing the patients'
perceptions about prevention and control of HCRI (PCH) implying factors
that influence the involvement and contribution of patients to their own
safety.
Theme 1: Insufficient information provided
In the studies, the patients' perception about the poor supply of
information about HCRI in health services in terms of quantity, quality and
means of disclosure was highlighted in the studies. Moreover, the
information provided was qualified as non-specific, superficial, inadequate
and discordant. The communication between health professionals (HP) and
patients was flawed, either verbally or due to the absence of printed
material or other means13-20. The aspects highlighted in the
papers were lack of information about the health situation of the patient,
when there is infection13,16-18; concepts in the theme of
infection and types of bacteria13,16,18; modes of transmission;
and PCM measures14,17,19,20. Although some patients had been
informed about the reason for the measures adopted, they expressed the
desire for additional information15-17, including written
guidelines19,20
Theme 2: difficulty to understand instructions on PCM
A convergence of limited understanding about PCM measures was observed 16,18-20. The studies reveal that some patients feel confused
and have incorrect concepts or ideas regarding the origin of the infection17,18, the modes of transmission and the use of paramentation 16,20 that are dissociated from preventive measures. The causes
of the difficult understanding identified were: personal, physical,
emotional and psychological factors related to the baseline condition and
insufficient knowledge of care practices; interpersonal factors such as
communication problems between professionals and patients and the
inadequate moment to receive guidelines; and cultural factors:
marginalization of patients by professionals and resistance for allowing
them to share in the process20.
It was observed that the excess of guidelines disclosed at the same time
hampered the retention of information17. It was not clear
whether patients did not remember the information or whether the
information had not been provided19. The experience of previous
HCRI seemed to favor awareness and understanding of means of transmission
and risks to patients12,20.
Theme 3: Negative feelings toward HCRI
Negative feelings prevailed in the experiences of the study patients.
Admission to the isolation room was solitary, worrying, limiting and
violent13. The feeling of discrimination, particularly on the
part of health care professionals, was observed in the case of delay to
respond the patients' requests without reasonable justification 13. The manifested fear and insecurity referred to different
aspects such as: diagnosis16, prognosis12, use of
personal protection equipment (PPE)16,17, fear of the bacteria 17 and fear of transmitting the infection to family members and
others16. Guilt and shame emerged in relation to partners and
about the possibility of having contaminated others15,17. Some
patients with multidrug resistant bacteria rejected the responsibility of
informing the health services that they were carriers of the infection 17.
Theme 4: Experiences for understanding IRAS and measures for PCH
Different levels of knowledge about PCH were recorded in the studies
analyzed. Insufficient numbers of bathrooms and showers and dirt on their
floor were mentioned as modes of transmission/contamination of HCRI in
health services12,16. It was mentioned that the patients
themselves and their attitudes toward hygiene were responsible for HCRI 12. Fomites, direct contact, care procedures, and professionals
recruited in banks of employees for eventual work were also mentioned. Some
patients saw infections as unavoidable in the hospital environment18.
Gloves and aprons stood out as measure of PCH in care provision by
professionals16,20. The use of PPE in waiting rooms and common
areas was poorly understood among patients17,20, but isolation
and treatment of infections, as well as surveillance and prevalence studies
are accepted for PCH20.
During an activity of reflection on material related to PCH, patients were
able to re-think their own hygiene habits, and they perceived potential
sites of accumulation of contaminants and problems with cleaning. In order
to better understand HCRI and PCH measures, patients cited strategies such
as Internet searches, conversations with other patients and attention to
parallel educational activities among teachers and students within the care
environment20.
Theme 5: Perception of inadequate professional attitudes
Some patients rely on practices developed by professionals in health
services18-20, believing that they will do what must be done and
that they are well trained12,18. However, instead of
professional behaviors, inadequate attitude were perceived13:
inadequate support and follow-up14,17, flaws in hygiene and
asepsis during care16, adoption of different behaviors depending
on the situation17 or when there was a hurry12.
Non-adherence of physicians to PCH measures caused confusion about correct
practices20.
Topic 6: Aspects that influence involvement in care
Some patients regard health recovery as a priority and/or believe that it
is the responsibility of the team to prevent infections and that they do
not have a role to play in PCH12,20. Other patients link
infections with factors such as: severity of the disease, type of hospital
and doubt about being heard8.
Although they denied their contribution, in one study the patients
discussed activities such as washing their hands regularly, maintaining
personal hygiene, participating in infection surveillance activities,
reporting inappropriate PCH measures, following rules, and maintaining
clean and organized their bed and space20. Furthermore, they
were willing to learn more about infection17,19 and to
collaborate by following guidelines12. Guidance to families and
visitors was considered a necessary practice in hospital routines 16 promoting greater participation in PCH measures related to
health care12.
The studies showed that most patients feel comfortable asking questions
about HCRI for the team. They believe they have the right to ask
professionals to wash their hands or cover their mouths when
sneezing/coughing, although they recognize a difficulty in approaching
professionals of the opposite gender, elderly people and physicians 12-18. Other patients revealed that they would never question
the behavior of the professionals because of shame or fear of being
reprimanded, to avoid offending the professional or dreading consequences 8,12,18,20. Young professionals, mainly nurses, are perceived as
more accessible and interested in interacting12.
DISCUSSION
The central role of patients in their own health care safety has been
highlighted in worldwide campaigns6, but studies dealing with
patients' perceptions about their possible contribution to PCH are rare. A
considerable part of the studies discusses bacterial multiresistance and/or
experiences of isolation13-17.
Access to information emerged in researches as a relevant problem for
patients, either due to lack of educational resources or due to the
professional-patient relationship that seemed to alienate the involved
persons. The themes "HCRI" and "safety measures for PCH" were complex to
understand, and obscured by the conditions in which the patients were.
Thus, the challenge is to find ways to change this reality, it is essential
that every party be involved to promote safety culture and reduce HCRI 12. The implementation of interventionist actions, changing the
paradigm of the passive role attributed to patients into active
participation in the health care process, in favor of best practices, is an
urgent need.
The texts portrayed the feelings of people affected by HCRI, namely, fear,
shame, guilt and discrimination interpreted as insecurity before the
unknown and associated, in part, with the impossibility of knowing the
mechanisms of transmission and where, how and when they were contaminated14,17. Keeping patients alienated in relation to their health
condition can generate distortions in the social representation they have
of themselves and of the environment in which they are inserted,
interfering in their understanding of the problem and of their actions16. In this sense, studies found that health professionals had
less contact and spent less time with patients who were in isolation15,21.
The professional-patient relationship was considered offensive when the
professional identified the patient as acarrier of multiresistant microorganism or contagious person17. Inappropriate interactions can
influence the patients' experiences with health care because they feel
stigmatized, feel uncomfortable to talk to professionals and they do this
contact only if absolutely necessary14. It is believed that good
communication improves patients' knowledge and trust in the team and
approximates them18,22. It is therefore important that
professionals have not only knowledge about infections and PCH practices,
but also empathic abilities to act respectfully and meet the patients'
expectations17. Having sensibility to identify the patients'
limitations/needs is essential to develop flexibility and educational
interventions to help them19.
The goal should be to allow patients to understand the infection, both for
the sake of their well-being and to increase their understanding of the
risk of transmission/contagion. It is imperative to manage HCRI so as to
avoid dissemination of the infectious agent, but also to control behaviors
and attitudes of professionals that contribute to the stigmatization of
patients17.
Patients' perceptions must be channeled appropriately within the
organization. Their participation should be welcomed both in deciding and
evaluating changes in health systems and information with the aim of
improving reliability and safety, bringing direct benefits to all8,18.
This study verified that a significant part of the patients of the
researches did not receive any sort of information about HCRI and they
often considered it difficult to obtain it from HP. Some patients even
regard HCRI as unavoidable, which was possibly endorsed by professionals 18. They mentioned dirt, lack of hygiene, fomites and
procedures, among others, as potential factors that contribute to the
transmission of microorganisms (MO)12,16,18. The use of PPE does
not always have its role understood, and transmits the idea of a
discriminatory measure and incites doubts among patients17,20.
The patients' own perceptions and attitudes regarding hygiene were
considered as responsible for the transmission of MO, more so than other
actors involved, such as the professionals12.
In view of the incontrovertible deficiency of provision of information to
patients revealed in the research, it is clear that patients were left to
understand the infections' nature and their means of transmission based on
the interpretation of their experiences12,18. Despite the
evident superficiality of the information on PCH measures, the patients
recognized inadequate behaviors adopted by professionals during care12,13,16,17,20 causing doubts about correct practices20,23.
The low adherence of health professionals to guidelines on precautions for
PCH is a known problem and a constant challenge24. It should be
emphasized that professionals should be committed to knowing patients with
infection, particularly those with multiresistant MO, and PCH measures,
factors that will bring safety to the team, patients and families,
minimizing negative feelings and outcomes. Equally important is the
responsibility of each professional to strictly observe the adoption of
best practices at all momentos during care provision13,16.
The authority of the health care team is striking and some patients feel
uncomfortable to question the decisions or actions of their caregivers for
fear of being labeled a "difficult patients" and/or offending a
practitioner with their concerns about safety and health care18.
The professional hierarchy and patient-employee relationships are
especially important in determining patients safety and attitudes12,25. Patients also face cultural marginalization, being
ignored or challenged when they express doubts about the practice or when
they verbalize their preferences. The ability of patients and their
families to contribute to safety is strongly shaped by the relationship
with team members.
It was mentioned that the use of audiovisual methods had a transformative
impact for the understanding of PCH20. In practice, hospitals
need to consider introducing mechanisms to fill the identified gaps and
minimize barriers to patients' participation in order to maximize the
benefits of infection prevention, which can be obtained with training
programs.
It is known that health education for patients reduces mortality rates and
promotes improvements in quality of life in different contexts26,27. The particularity of training patients should be the
respect for the unique and valuable perspectives of the patients. These
programs must seek to break up with the paradigm where only health
professionals play a role in the prevention of HCRI and emphasize that the
patients are the only persons present in all phases of their care, having
an active role to play in favor of their safety. In addition, it is
suggested to monitor the progress, using indicators of the need for
patients' involvement, to be developed and implemented12.
CONCLUSION
The involvement and participation of patients in the measures of prevention
and control of HCRI represent a path to be followed with the goal to
advance safety in health care. It was identified that the patients'
perceptions are usually negative and indicate factors that make it
difficult to reach the goal and they include the provision of insufficient
or inadequate information, the difficulty to understand PCH, the
predominance of unfavorable feelings and experiences and the behavior of
HP. These factors contribute to the patients' passive participation in
their own safety.
The gap between the understanding of PCH by patients and their involvement
in the process indicates the need for strong actions to favor effective
communication, better health-patient professional relationships and ease of
access to timely provision of information that will enable and encourage
interaction and contribute to safer care.
It is understood, therefore, that this review gathered evidence on how
patients perceive PCH and report their experiences, reinterpreting the
technical knowledge. The results are important because they added useful
and relevant information that provide the conditions for HP to reflect on
the emerging aspects that form the basis for researches exploring
methodologies with potential to promote changes so as to actively integrate
patients in order to reduce health care risks.
REFERENCES
1.Centers for Disease Control and Prevention. Types of
Healthcare-Associated Infections [site de Internet]. Atlanta: CDC; 2014
[cited in March 7, 2016]. Available from:
http://www.cdc.gov/HAI/infectionTypes.html
2.Pittet D, Allegranzi B, Storr J, BagheriNejad S, Dziekan G,Leotsakos A,et
al.Infection control as a major World Health Organization priority for
developing countries. J. Hosp. Infect.
2008; 68(4): 285-92.
3.Allegranzi B, BagheriNejad S, Combescure C, Graafmans W, Attar H,
Donaldson L, et al. Burden of endemic health-care-associated infection in
developing countries: systematic review and meta-analysis. Lancet. 2011;
377(9761):228-41.
4.Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al.
Hospital organisation, management, and structure for prevention of
health-care-associated infection: a systematic review and expert consensus.
Lancet Infect Dis. 2015;15(2):212–24.
5.Flanagan ME, Welsh CA, Kiess C, Hoke S, Doebbeling BN. Agency for
Healthcare Research and Quality Hospital-Acquired Infections Collaborative.
A national collaborative for reducing health care-associated infections:
Current initiatives, challenges, and opportunities. Am. J. Infect. Control.
2011; 39(8): 685-9.
6.World Health Organization. Patients for patient safety what's new?
[site de Internet]. Geneva: WHO; 2016 [cited in March 10, 2016]. Available
from:
http://www.who.int/patientsafety/patients_for_patient/en/
7. Ministry of Health (BR). Ordinance nº 529 of April 1, 2013. Establishes
the National Patient Safety Program (PNSP) [Internet site]. Brasília: MS;
2013 [cited in March 10, 2016]. Available from:
http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html
8.Ahmad R, Iwami M, Castro-Sánchez E, Husson F, Taiyari K, Zingg W, et al.
Defining the user role in infection control. Journal of Hospital Infection
2016; 92:321-7.
9.Flemming K, Briggs M. Electronic Searching to locate qualitative
research: evaluation of three strategies. J. Adv. Nurs. 2007; 57(1):95-100.
10.Green J, Britten N. Qualitative research and evidence based medicine.
BMJ. 1998; 316(7139):1230-2.
11.Thomas J, Harden A. Methods for thematic synthesis of qualitative
research in systematic reviews. London: ESRC National
Centre for Research Methods.2008; (NCRM Working Paper Series;
10/07). doi: 10.1186/1471-2288-8-45.
12.Seale H, Travaglia JF, Chughtai AA, Phillipson L, Novytska Y, Kaur R. 'I
don't want to cause any trouble': the attitudes of hospital patients
towards patient empowerment strategies to reduce healthcare-acquired
infections. J. Infect. Prevent. 2015; 16(4): 167-73.
13.Skyman E, Sjöström HT, Hellström L. Patients' experiences of being
infected with MRSA at a hospital and subsequently source isolated. Scand J.
Caring. Sci. 2010; 24(1):101-7.
14. Lindberg
M, Carlsson
M, Skytt
B. MRSA-colonized persons' and healthcare personnel's experiences of
patient–professional interactions in and responsibilities for infection
prevention in Sweden. J. Infect. Public. Health. 2014; 7(5):427-35.
15.Lupión-Mendoza C, Antúnez-Domínguez MJ, González-Fernández C,
Romero-Brioso C, Rodriguez-Bano J. Effects of isolation on patients and
staff. Am. J. Infect. Control. 2015;43(4):397-9.
16.Santos HG, Santos CIL, Lopes DFM, Belei R. Bacterial multiresistance:
the experience of patients hospitalized in a school hospital in the city of
Londrina-PR. Cienc. Cuid. Saude. 2010;9(1):74-80.
17.Lindberg M, Carlsson M, Högman M, Skytt B. Suffering from
meticillin-resistant Staphylococcus aureus: experiences and
understandings of colonization. J. Hosp. Infect. 2009; 73(3):271-7.
18.Burnett E, Lee K, Rushmer R, Ellis M, Noble M, Davey P.
Healthcare-associated infection and the patient experience: a qualitative
study using patient interviews. J. Hosp. Infect. 2010; 74(1):42-7.
19.Hill JN, Evans CT, Cameron KA, Rogers TJ, Risa K, Kellie S, et al.
Patient and provider perspectives on methicillin-resistant Staphylococcus aureus: a qualitative assessment of knowledge,
beliefs, and behavior. J. Spinal Cord. Med. 2013;36(2):82-90.
20.Wyer M, Jackson D, Iedema R, Hor SY, Gilbert GL, Jorm C, et al.
Involving patients in understanding hospital infection control using visual
methods. J. Clin. Nurs. 2015; 24(11-12):1718-29.
21.Abad C, Fearday A, Safdar N. Adverse effects of isolation in
hospitalized patients: a systematic review. J. Hosp. Infect. 2010;
76(2):97-102.
22.Rees J, Davies H, Birchall C, Price J. Psychological effects of
isolation nursing (2): patient satisfaction. Nurs. Stand. 2000;14(29):32-6.
23.Pittet D, Panesar SS, Wilson K, Longtin Y, Morris T, Allan V, et al.
Involving the patient to ask about hospital hand hygiene: a National
Patient Safety Agency feasibility study. J. Hosp. Infect. 2011;
77(4):299–303.
24.Backman C, Marck PB, Krogman N, Taylor G, Sales A, Bonten MJ, et al.
Barriers and bridges to infection prevention and control: results of a
qualitative case study of a Netherlands' surgical unit. BMJ Open. 2012;
2:e000511. doi:10.1136/bmjopen-2011-00051.
25.Doherty C, Stavropoulou C. Patients' willingness and ability to
participate actively in the reduction of clinical errors: a systematic
literature review. Soc. Sci. Med. 2012; 75(2):257–63.
26.Vasconcelos SC, Frazão IS, Vasconcelos EMR, Cavalcanti AMTS, Monteiro
EMLM, Ramos VP. Self-care demands in a therapeutic group: health education
with users of psychoactive substances. Rev. enferm. UERJ. 2013;
21(1):79-83.
27.Gonçalves FG, Albuquerque DC. Health education of patients with heart
failure. Rev. enferm. UERJ. 2014; 22(3):422-8.