ORIGINAL RESEARCH
Socio-demographic and clinical characteristics of patients with immunobullous dermatoses
Euzeli da Silva BrandãoI; Iraci dos SantosII; Regina Serrão LanzillottiIII
I
Nurse. PhD. Specialist in Nursing in Dermatology. Assistant Professor.
Universidade Federal Fluminense. Niterói, Rio de Janeiro, Brazil. E-mail: euzeli@terra.com.br
II
Nurse. PhD. Titled Professor at Universidade do Estado do Rio de Janeiro.
Brazil. E-mail: iraci.s@terra.com.br
III
Statistic. PhD in transport engineering. Assistant Professor. Universidade
do Estado do Rio de Janeiro. Brazil. E-mail:
reginalanzillotti@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2016.27415
ABSTRACT
Objective: to identify the socio-demographic and clinical characteristics of patients with immune bullous dermatoses. Method: in this interinstitutional, cross-sectional, quantitative study, carried out from June 2012 to April 2013, data were produced using the Dermatology Client Evaluation Protocol, validated by experts. Exploratory analysis of the variables included frequency distribution of categorical and continuous variables and contingency tables, with confidence intervals compatible with statistical inference for small samples by Student's-t probability distribution. Results: the 14 participants – 11 with pemphigus and three with bullous pemphigoid – were predominately female (11), and mean age was 58 years. Self-declared color/ethnicity was eight white and six brown, while five were from Rio de Janeiro, and rest from other states in Brazil. Pain was the predominant complaint for 11 of the 14 clients, six with pemphigus vulgaris. Conclusion: the socio-demographic and clinical characteristics identified attested to their importance with a view to comprehensive care.
Keywords: Nursing; nursing care, dermatology; pemphigus.
INTRODUCTION
Affected by skin lesions and/or mucous membranes usually extensive and widespread, the person who has an immunobullous dermatosis (ID) becomes vulnerable to risks, especially when they are in a hospital environment 1.
Despite significant and undisputed understanding of nursing as a profession that has its own specific functions and the importance of nursing care for the recovery of people with ID, it is observed precariousness of the publications and national and international research addressing this theme, including the sociodemographic and clinical characteristics 1,2.
Understanding that nursing professionals play a fundamental role in promoting comfort, in preventing complications and even in maintaining the life of this specific clientele, the lack of knowledge about the characteristics presented by it can make it unfeasible to care, increase stigma and suffering, contradicting a culture focused on the quality of care aimed at humanization1.
From these considerations, it is believed that this study can contribute to the qualification of nursing care with this clientele. Thus, the following research question has been formulated: what are the sociodemographic and clinical characteristics presented by people who are hospitalized with immunobullous dermatoses?
Therefore, we intend to reach the following objective: to identify sociodemographic and clinical characteristics of the patients who are hospitalized with immunobullous dermatoses.
LITERATURE REVIEW
The ID are chronic diseases with a primary and fundamental manifestation of the development of blisters and less frequently of vesicles on the skin and/or mucous membranes. These dermatoses are caused by the activation of the immune system against the body's own constituents; in this case, antibodies are produced against specific structures of the skin, considered autoantigens. These autoantigens may be located in the intraepidermal or subepidermal regions, being indispensable to the identification of their location for classification of the type of immunobullous dermatosis 3,4.
The pemphigus are the most common ID. Due to their intraepidermal location, bullous lesions are more superficial and consequently more sensitive, breaking more easily than those of subepidermal origin. There are different types of pemphigus: vulgar (PV), foliaceous, those which are drug induced, herpetiformis, paraneoplastic and immunoglobulin A (IgA), the first two being considered the main ones1,3. In all types of pemphigus, the pain is typical, and there might be complaints regarding pruritus. The lesions exude a characteristic foul odor that can become more intense in the presence of infection.
The subepidermal IDs are: bullous pemphigoid, pemphigoid of mucous membranes, gestational pemphigoid, dermatitis herpetiformis, linear IgA dermatosis and acquired epidermolysis bullosa3, the blisters are more resistant, pain and odor may be present, the latter mainly in the presence of infection.
METHODOLOGY
A quantitative, cross-sectional study carried out between June 2012 and April 2013 in three different institutions, characterizing the study as interinstitutional. In view of the proposal to work with people who have an unusual skin problem, the convenience sample of 14 participants is justified. Among them, 12 are from two university hospitals, located in the state of Rio de Janeiro, and two of them are from Hospital Adventista do Pênfigo/Campo Grande/Mato Grosso do Sul (HAP/MS).
The following inclusion criteria were established: hospitalized adults in the wards of the cited institutions with a diagnostic hypothesis or with a definitive diagnosis of active ID, independent of previous hospitalizations, gender, age group and use of systemic medication or not. Exclusion criteria: people in outpatient follow-up; hospitalized in units/or beds which are not specialized in dermatology; in psychiatric treatment, disoriented in time and space.
For the collection of sociodemographic and clinical data, the Dermatology Client Evaluation Protocol (DCEP) has been used, an instrument validated by dermatology specialist nurses5. Its application is compatible with the phases of the nursing process, becoming a source of data for nursing research in dermatology. Divided into 10 parts, the DCEP is composed of the following items: identification and sociodemographic data; history containing the clinical variables; the patient's knowledge regarding cutaneous disease, degree of discomfort and emotional and spiritual repercussions of the illness; physiological aspects; how patients see and feel about the disease; concerns about hospitalization and expectations regarding nursing; physical exam; survey of nursing diagnoses; record of interventions and reassessments5.
Thus, during the exploratory analysis of sociodemographic and clinical data, due to the reduced number of subjects, the variables contained in the DCEP were treated with the use of frequency distribution of categorical and continuous variables and contingency tables in order to evaluate the association of attributes.
If measured on continuous scale, the confidence intervals (CI) have been treated by statistical inference for small samples according to the TStudent probability distribution. The Bayes' Theorem, which deals with relationships involving conditional probabilities6 has been applied.
Therefore, it has been analyzed:
Variables in sociodemographic categorical and interval scale: gender, self-declared color/ethnicity, consensual union, schooling, profession, nationality, origin, religious belief, family constellation, place of residence.
Scaled variables in scale of reason, continuous variables: age, family income.
Clinical variables: main complaint, medical diagnosis, comorbidities, allergies, previous diseases, family diseases, previous hospitalization, drug therapy, alcohol and drug use, preventive examinations, cutaneous disease, physiological aspects (human needs) and characteristics of cutaneous affections, social, emotional and spiritual aspects.
The nursing process (NP) is a methodological tool because it allows to identify, understand, describe, explain and/or predict how the patient responds to health problems or their vital processes, and it determines which aspects of these responses require professional intervention 7. The data produced, according to the NP have been recorded in two forms: PACD5 and the Compromising Cutaneomucous Index of Patients with Vulgar Pemphigus (CCIPVP)8 which have already been validated and published. The CCIPVP scores four different items: Number of bubbles or eroded areas where there has been previously blister; Size of the bubbles or eroded areas; Nikolsky's sign; mucosal involvement and sepsis. The participants with the other IDs have not been evaluated by this index, since it was specifically intended for patients with pemphigus vulgaris (PV)8.Despite the application of all stages of the EP, this article is limited to the reference production of the socio-demographic and clinical data identified. This is a crop of doctoral thesis, whose project was approved by the Research Ethics Committee of the Hospital Universitário Pedro Ernesto da Universidade do Estado do Rio de Janeiro (HUPE/UERJ), as the verdict 3119/2011. It should be noted that the patients who agreed to participate in the research have signed an Informed Consent Form, in accordance with the Resolution No. 466/20129.
RESULTS AND DISCUSSION
Sociodemographic characteristics of the patients with ID
The 14 participants are Brazilian, with an average age of 58 years old, predominantly female - 11 people - and they are married, and/or have a partner. Nine of them are married and/or have a partner. Among the nine participants who have received a diagnosis of PV, the most prominent are those of the female gender, with the youngest being 27 years old and the oldest 64, and four of them are in the fifth decade of their lives. These results are consistent with the literature when citing that, although it may affect people of any age, this disease is more common in adults between the ages of 40 and 60 years old without, without a gender distinction 3,10.
It is noteworthy that the three patients with bullous pemphigoid (BP) are the oldest, being a white man of 71 years old and two women, an 81-year-old white woman and an 82-year-old "mixed-race" female. Ages and ethnicities are important, since the involvement of older people of both genders and of different ethnicities are characteristics of the BP3,4.
Among the self-declared color/ethnicity, there are eight white and six "mixed race" people. As for the religious belief, one person stands out for professing two religions (Kardecist and catholic), seven are catholic, five evangelicals, and a Kardecist.
Regarding the geographical characteristics of the origin, place of residence and specialized dermatology care clinics, five natives of Rio de Janeiro and the others from different states of Brazil stand out. Most of the participants are from different municipalities of the state of Rio de Janeiro, among them, nine live in neighborhoods that are relatively close to university hospitals.
However, due to the absence of a specialized inpatient unit in dermatology in Piabetá, Angra dos Reis and Volta Redonda, three of the patients took an inter-municipal trip to be attended. Still, two patients needed to make an interstate displacement from Mato Grosso and Distrito Federal to Mato Grosso do Sul. This fact, in addition to translating the difficulty of access to the specialized service, may make it impossible to contact family members during hospitalization, which may interfere with the process of coping with the disease and recovery.
Regarding the monthly income, seven people earn below two minimum wages, with an average number of three to four members in the family. Only three participants have income above 2 to 4 minimum wages, with an average number of four people in the family. It is an alarming fact, considering the chronical and serious aspect of the ID, the expenses with medicine and topical products, as well as the shift to specialized care.
Regarding schooling, training/occupation, there are eight people with a complete/incomplete elementary degree, who are predominant, being seven in activities considered of low complexity, such as waiter, manicure, hairdresser, cook, seamstress. It is worth mentioning the presence of two participants without any schooling and two of them with complete/upper course in progress.
The prevailing low schooling level of the participants should be taken into consideration regarding health orientation/education, considering the need for patients to understand their illness and self-care11-13, especially with regard to the continuity of treatment/care at home, since the use of complex medications such as steroids and immunosuppressive drugs are needed to maintain the disease control3,4. In addition, it is possible to alert them to the possible adverse effects of these drugs, such as hyperglycemia and arterial hypertension14,15, which require the active participation of the patient for control. These facts reveal the importance of the role of nurses in the orientation, identifying difficulties and creation of strategies along the health team in order to prevent injuries and recurrences1.
Clinical characteristics of patients with ID
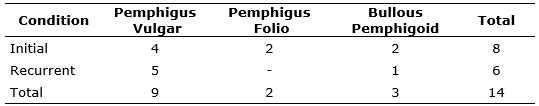
Eleven patients with pemphigus, including nine with PV and two with pemphigus foliaceus (PF), and three patients with BP participated in the study. The two patients with PF have been first affected, while from the three with PB, one had a recurrent condition and the other had an initial condition. See Table 1.
TABLE 1:
Distribution of patients by disease occurrence. Rio de Janeiro, 2014.
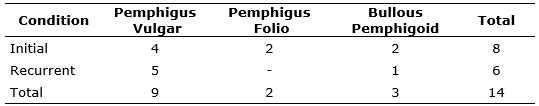
The predominance of patients with PV ratifies the literature3,4. It should be noted that of the nine clients with this modality, five showed relapsing conditions.
Regarding the CCIPVP8, from the nine participants with PV, six of them reached an expressive index, which was above 60. Nine participants showed lesions in the buccal mucosa, seven with PV, one with BP and another one with PF; and the last two characterized atypical facts.
In view of the characteristics of the skin lesions resulting from these dermatoses, pain complaints are usually present3 and require nursing actions that promote physical and emotional relief, considering skin involvement, and the relevance of body and lesion exposure1,2.
As for the evaluation of the CCIPVP8, among the nine participants with this disease, three of them presented CCIPVP equal to 60, followed by two with index equal to 80. The others have reached indices equal to 30, 35, 40 and 100, respectively.
It is predominant the number of hospitalizations for the first time due to cutaneous disease -11 people, six with PV, two with PF and three with BP. Three with PV reported two or more hospitalizations, a fact that highlights the difficulty of controlling of disease.
Three people reported the simultaneous presence of complications such as high blood pressure and diabetes after regular use of corticosteroid for the treatment of cutaneous disease, which is a common fact according to the literature3,4.
Regarding the history of systemic treatment for cutaneous disease, it is recorded that 10 out of the 14 patients had already used oral corticosteroids; eight of them with PV, reported the use of prednisone, a drug which is indicated for the control of this dermatosis3,4.
Despite the use of systemic corticosteroid by five participants before the hospitalization, the hospitalization occurred due to a lack of success in the evolution of the condition. In this regard, the importance of assessing the dose of medicine by the medical staff associated with the nursing care stands out. Among them, the specialized and personalized care, the cleaning and protection of the lesions, the guidelines on the disease and self-care, as well as the readiness to listen to the problems being voiced by the patient1,2,13.
Still regarding the use of medications to control the disease, only one patient with PV had already been used the immunosuppressant micofenolatomofetil, which acts on the enzyme inosine monophosphate dehydrogenase, responsible for the metabolism of purines. Due to the fact that lymphocytes use this metabolic pathway, their inhibition suppresses the proliferation of lymphocytes and the formation of autoantibodies 14.
Regarding the topical care, only one patient was on dressing with Vaseline gauze prior to the beginning of the research. However, the use was inadequate, due to insufficient amount of Vaseline and the technique used. It caused the adhesion of the bandage on the wound bed and, consequently, increase of the injured area1.
As for the history of diseases in the family, the presence of predisposing factors for the development of common complications such as diabetes and hypertension during the treatment with corticosteroids15 is of great concern.
In view of the causes of cutaneous illness pointed out by the study participants, it is necessary to favor the exposure of feelings and emotions, as well as the availability of the professional to listen to the verbalized problems and to offer guidance to the patients11-13.
Regarding the intake of alcoholic beverages, smoking and the use of illicit drugs, from the three male participants, only one had a medical diagnosis of PV, he stated to be a smoker, with consumption of one pack per day, for approximately 30 years now, as well as the habit of drinking beer every weekend. The other two participants denied the use of cigarettes, alcohol and illicit drugs. In the case of women, from the 11, four reported drinking wine socially, and all of them denied using cigarettes and illegal drugs.
Regarding the preventive tests for cancer, it prevailed those who did not observe such a control regularly. From the three participants with a medical diagnosis of BP, two of them do not undergo preventive examination regularly. The three male patients have stated that they have never performed the mentioned test.
The pain was the main complaint in 11 of the 14 participants, six of them with PV, followed by the complaint of exposure, cited by two patients also with PV. Only one patient with PV complained of pain accompanied by exposure.
In relation to previous diseases, one participant with a medical diagnosis of PF denied a history of other diseases. The remaining 13 mentioned the presence of one or more health problems, in addition to the cutaneous condition. It is an alert the fact that nine people have reported high blood pressure, four have diabetes and five have a history of allergies.
Regarding the history of the systemic treatment for cutaneous disease, it stands out that 10 patients had already used oral corticosteroid, eight of them diagnosed with PV. From the two remaining patients, one of them received a medical diagnosis of PF and was taking prednisolone before the admission and another who had BP, was taking prednisone. From the remaining four, one had BP and had used only topical corticosteroid, while two, one who had PF and another who had BP, denied previous treatment; one of them did not provide any information.
In this sense, from the six patients with initial Pemphigus condition, including four who had PV and two who had PF, five reported the use of systemic corticosteroid at the time of admission.
The topical application of corticosteroids was described by five clients, four of them being associated with systemic treatment. It should be highlighted that one of the participants made use of herbal baths (carobinha/aroeira), a fact that may have complicated even more the condition.
At the time of admission, from the nine patients who had PV, four had already used corticoid; out of these, only one used this drug exclusively, while the other three used other medications such as oral hypoglycemic and analgesic, as well as hormone replacement due to climacteric. Only one patient had already made use of the immunosuppressant micofenolatomofetil. Two other patients reported the use of painkillers (only). Regarding the patient who had PF, one of them used steroids and antibiotics, another one did not report use of any drugs. From the three participants who had BP, one of them used corticosteroid associated with antihypertensive drugs, analgesics and clonazepam. Another one used antihypertensive drugs and painkillers, and the third, associated the use of oral hypoglycemic drugs with other medications such as acetylsalicylic acid.
Regarding the history of diseases in the family, six patients have a family history of diabetes, three of neoplasms, and two of hypertension.
It was verified that the cause of the cutaneous illness is unknown for eight people, however, four alleged emotional causes like stress and preoccupation, besides situations like nervousness, anxiety, agitation, illness or death of beloved one, religious conflict, and preoccupation with the children, hassles, debts, and overwork. Although the literature does not point out studies that prove the relation between the mentioned causes and the cutaneous illness, it is important to value the testimony of the patient.
Among the concerns, predominate aspects related specifically to cutaneous disease, such as tests results/beginning of the treatment, seizure, discomfort, healing, recovery. One patient, from another state, mentioned the fear of evolving to death and no longer seeing her daughter. Another 27-year-old patient was concerned about being away from study/work, as well as learning more about the disease. Another patient that left her municipality to be hospitalized said that she misses her family. Three elderly people have denied worries.
Regarding the time of hospitalization, it has been observed the average of 36 days. The shorter stay time, eight days, was reached by the youngest patient, diagnosed with PV. The longest hospitalization time, 99 days, was recorded by an elderly woman who, despite the healing of the characteristic PV lesions, presented orthopedic problems, requiring physical therapy follow-up.
It is important to highlight that one of the patients who had PV, with CCIPVP = 30, requested discharge after four days of hospitalization, due to the absence of adaptation to the environment of the ward. According to her, because she has a health insurance, she preferred to receive the medication in a private institution, with a private room.
Regarding the causes of discomfort, it was verified that the pain was mentioned by 10 patients, six of them in isolation and the other four associated with other factors such as itching, presence of facial injuries and stigmatizing looks of the people.
Among the changes in life habits, one participant mentioned changes in all aspects; others have cited isolation, suspension of work and daily activities, limitation of movement, difficulty walking, sleeping, and one mentioned the cutaneous illness as the worst event in his life.
As for stigmatizing looks of society and discrimination, the confronting attitudes pointed to - avoiding the exposure of the body affected by injuries, using the change in clothing style; do not attend beaches/parties; stop working and having sexual relationships due to shame (self-shame and of others). Only one patient who had CCIPVP = 30 mentioned performing physical activity and going to the hairdresser.
Despite the mentioned changes in life habits, no patient mentioned changes in the relationship with the family. Only three female patients diagnosed with Pemphigus (a PF and two PV) reported changes in the relationship with friends.
Regarding the changes in the work environment, nine participants were retired and/or away from work. The others confirmed changes, and two noticed the change in the relationship with friends; among the reasons, there is misinformation about the disease and fear of contagion. It is worth noting that one participant did not provide any information, and the other who works at home as a seamstress denied any change with the customers.
Regarding the sexual relationship, six patients reported not practicing sexual activity independent of their cutaneous disease, a fact justified by them due to the age of the group, which is between 58 and 82 years old. Seven clients aged between 27 and 62 years old stated that skin and/or mucosal lesions caused by ID have made sex unfeasible due to fear of injury and worsening of the disease, especially in cases of lesions on the vaginal mucosa; besides the fact that they feel ugly and lack physical and emotional structure.
About the meaning of hospitalization, the predominant answers considered the event positive (10). For the rest, the admission meant suffering, bad feeling, difficulty of acceptance, mostly loneliness, due to having the family distant, cited by one of the patients who is from another state.
The discharge request by one of the participants with PV, due to lack of adaptation to the environment, ratifies the need for better structural conditions and customer protection against stigmatizing looks of society, including within the hospital environment13,16.
The change in body image usually causes serious psycho-affective repercussions, forcing them to move away from work activities. The strategies used by people to avoid the stigma, as, for example, studying at home regime, confirm the findings of others about patients with skin disorders in inpatient regimen16.
Regarding the positive meaning of hospitalization for 10 participants, the responses also corroborate study results, already cited on a support group with hospitalized patients with cutaneous conditions16.
CONCLUSION
Despite the limited number of patients, due to the fact that it is a group of rare diseases, a limitation of the study, the results presented are extremely relevant for the dissemination of sociodemographic and clinical characteristics of this specific clientele. They reveal the importance of nursing to promote comfort/well-being and prevention of aggravations, essential aspects for the integral care of patients. The scope of the objective formulated answered the question of the research showing the need for training nursing professionals to meet the entirety of the human being along with the health team.
REFERENCES
1.Brandão ES, Santos I. Evidences related to the care of people with pemphigus vulgaris: a challenge to nursing. Online Braz J Nurs [Internet]. 2013 [citado 2016 nov. 02]; 12(1):162-77. Disponível em: http://www.objnursing.uff.br/index.php/nursing/article/view/3674 . DOI http://dx.doi.org/10.5935/1676-4285.20133674.
2.Brandão ES, Santos I, Carvalho MR, Pereira SK. Nursing care evolution to the client with pemphigus: integrative literature review. Rev enferm UERJ. 2011;19(3):479-84.
3.Hanauer L, Azulay-Abulafia L, Azulay RD, Azulay DR, Azulay RD. Doenças vesicobolhosas. In: Azulay RD, Azulay DR, Azulay-Abulafia L. Dermatologia. Rio de Janeiro: Ed. Guanabara Koogan; 2013. p. 145-61.
4.Cunha PR, Barravieira SRCS. Dermatoses auto-imunes. An Bras Dermatologia. 2009;84(2):111-24.
5.Brandão ES, Santos I, Lanzillotti RS. Validation of an instrument to assess patients with
skin conditions. Acta Paul Enferm [Internet]. 2013 [cited 2016 Nov. 02]; 26(5):460-6. Available in: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002013000500009&lng=en . DOI http://dx.doi.org/10.1590/S0103-21002013000500009
6.Bussab WO, Morettin PA. Estatística básica. São Paulo: Editora Saraiva; 2002.
7.Garcia TR, Nóbrega MML. Processo de enfermagem e os sistemas de classificação dos elementos da prática profissional: instrumentos metodológicos e tecnológicos do cuidar. In: Santos I, Figueiredo NMA, Padilha MCS, Cupello AJ, Souza SROS, Machado WCA. Enfermagem assistencial no ambiente hospitalar: realidade-questões-soluções. São Paulo: Ed. Atheneu; 2004. p. 37-64.
8.Souza SR, Azulay-Abulafia L, Nascimento LV. Validation of the commitment index of skin and mucous membranes in pemphigus vulgaris for the clinical evaluation of patients with pemphigus vulgaris. An Bras Dermatol [Internet]. 2011 [citaded 2016 Nov 10]; 86(2):284-91. Disposable in: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962011000200012&lng=en&nrm=iso&tlng=en . DOI http://dx.doi.org/10.1590/S0365-05962011000200012 .
9.Ministério da Saúde (Br). Resolução 466 de 12 de dezembro de 2012. Diário Oficial da União, Brasília Distrito Federal, 13 jun.2013. Seção 1, p. 59.
10.Gonçalves GAP, Brito MMC, Salathiel AM, Ferraz TS, Alves D, Roselino AMF. Incidence of pemphigus vulgaris exceeds that of pemphigus foliaceus in a region where pemphigus foliaceous is endemic: analysis of a 21-year historical series. An Bras Dermatologia. 2011;86(6):109-12.
11.Santos I, Gauthier J, Caldas CP, Figueiredo NMA, Erdmann AL. Caring for the whole person: the contributions of aesthetics / sociopoetics perspectives to the field of nursing. Rev enferm UERJ. 2012;20(1): 4-9.
12.Brandão ES, Santos I. Admission forms in dermatology: a facilitating instrument for personal and integral nursing care. Rev Tend Enferm Prof. 2009;2(2):93-7.
13.Santos I, Brandão ES, Clos AC. Dermatology nursing: sensitive listening skills and technology for acting in skincare. Rev enferm UERJ. 2009;17(1):124-30.
14.Bressan AL, Silva RS, Fontenelle E, Gripp AC. Imunossupressores na dermatologia. An Bras
Dermatol [Internet]. 2010 [cited 2016 Nov 05]; 85(1):9-22. Available in: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S036505962010000100002&lng=en . DOI http://dx.doi.org/10.1590/S0365-05962010000100002 .
15.Azulay DR, Azulay-Abulafia L, Azulay RD. Drogas de grande valor em terapêutica dermatológica. In: Azulay RD, Azulay DR. Azulay-Abulafia L. Dermatologia. 5ª ed. Rio de Janeiro: Ed. Guanabara Koogan; 2013. p. 872-910.
16.Santos I, Jesus PBR, Brandão ES, Oliveira EB, Silva AV. Repercussions of skin conditions in people's lives: sócio-poitizing self-imagem and self-esteem. Rev enferm UERJ. 2014;2(2):157-62.