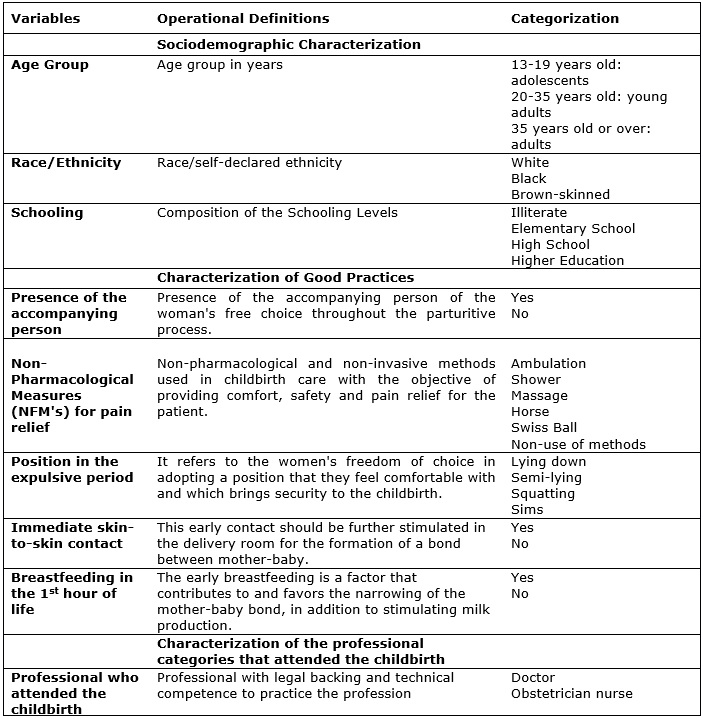
FIGURE 1: Operational definitions and categorization of study variables.
ORIGINAL RESEARCH
Good Partices in obstetric care and its interface with humanization of assistance
Larisse Ferreira Benevides de AndradeI; Quessia Paz RodriguesII; Rita de Cássia Velozo da SilvaIII
I
Nurse. Post-graduation in Nursing in Neonatal and Pediatric Intensive
Care Unit, "Atualiza Cursos". Bahia. Brazil. E-mail:
larisse_ferreira@hotmail.com
II
Nurse. PhD Student at the Federal University of Bahia. Professor at the
Ruy Barbosa Faculty/Devry Brazil. Salvador, Bahia. Brazil. E-mail: qprodrigues@gmail.com
III
Nurse. PhD Student at the Porto University, Portugal. Salvador, Bahia.
Brazil. E-mail: rvelozo2009@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2017.26442
ABSTRACT
Objective: to analyze good practices adopted in caring for the woman and the newborn in a public hospital from Bahia supported by Brazilian Rede Cegonha. Method: it is a descriptive and retrospective study with a quantitative approach, based on secondary data. The documental research used the medical records of 337 women, on September 2015. The study was approved by the Research Ethics Committee of the hospital (registered as number 1185928 / 2015). Results: the predominant women in the study were 20 to 35 years old, afrodecendents, with high school education and in the first parturition. It was identified the use of the following good practices: the presence of companion (79,2%), non-pharmacological methods of pain relief (23,1%), immediate skin-to-skin contact (51,6%) and breastfeeding in the delivery room (38%). Most of parturition (95,3%) were assisted by doctors. Conclusion: among the good practices analyzed, only the presence of companion and skin to skin contact occurred with the majority of women. The others had low adherence. It is necessary the commitment from the organization and the team in order to make good practices effectively adopted.
Keywords: Humanized delivery; nursing care; obstetric nursing; obstetric.
INTRODUCTION
The social vulnerability of women and children to some risk situations is a determinant factor for their morbidity and mortality, with emphasis on maternal and neonatal deaths. The hegemony of the biomedical model in obstetric and neonatal care and the uncritical use of technical knowledge can contribute to an increased risk and make any attempt to change ineffective.1
The institutionalization of the childbirth has transformed the parturition process into a hospital-centered event, seen as a pathological condition, promoted by the intense medicalization, unnecessary surgical interventions and moving away from the women's domain during the process. On the other hand, new approaches to childbirth have emerged with a humanistic approach centered on women and their particularities.2,3
The obstetric care in Brazil is still focused on the biomedical model, which has contributed to the increase of invasive and interventional procedures during labor, and consequently, reflecting the high rates of maternal and perinatal morbidity and mortality.4 Despite all the discussion about the care provided to the woman and to the newborn, it is still observed the predominance of the adoption and incorporation of medical obstetric practices.5 According to studies, medications such as oxytocin have been used in most of the vaginal deliveries, while the cesarean section has become the most common route of birth.6 The routine use of oxytocin causes side effects, such as uterine hyper stimulation and increased pain.7
Good conditions of professional and institutional care for the delivery can reduce the occurrence of maternal death. The professional care provided to the pregnant and/or parturient women is a key element in obtaining good results, both maternal and perinatal.8
The current World Health Organization (WHO) and Ministry of Health (MS) in Brazil recommendations for the management of labor include supply of liquids, encouragement to adopt upright positions, freedom of movement and use of non-pharmacological methods for pain relief, aiming at the maternal comfort and better progression of labor.9
Considering that the pregnancy and birth are physiological events in a woman's life, it is the responsibility of all he professionals involved in this care to provide an environment of humanism and security, encouraging and empowering her throughout the process. Thus, this study aimed at analyzing the good practices adopted in the care of the women and newborn in a public maternity in Bahia, supported by the Stork Network ("Rede Cegonha"). These practices have proven efficacy in the management of the parturition process, reducing the labor time, increasing the mother-baby bond, reducing the need for interventions, and allowing the delivery to take place physiologically and naturally as it should be.
LITERATURE REVIEW
Providing humanized care, based on the principles and strategies of the National Humanization Policy (NHP) should be a way to achieve improvements in the quality of care10. Aiming at reducing unnecessary cesarean rates, as well as promoting more humanized obstetric care, the Ministry of Health regulated several ordinances, such as the set of ordinances that instituted the Humanization Program in Prenatal and Birth (HPPB).
The HPPB looks for the rescue of integrated, qualified and humanized obstetric care. It is based on the precepts that the Humanization of Obstetric and Neonatal Care is necessary for the adequate follow up of the childbirth and the puerperium.11
With the proposal of a strategy, the Stork Network was launched in March 2011, instituted by Administrative Rule MS/GM No. 1459/2011, aiming at organizing a network of care that guarantees women the right to reproductive planning and humanized care for pregnancy, childbirth and the puerperium, as well as children the right to a safe birth and a healthy growth and development.12
Thus, the Stork Network proposes qualification of the care provided at the childbirth and birth, guaranteeing sufficiency, expansion of the care services to pregnant women, quality of the services provided, with a change in the management model and care. This change aims to transform the maternity facilities, ensuring a better environment in the obstetrical centers, in addition to qualifying the care by stimulating good care practices to the childbirth and birth.12
METHODOLOGY
A descriptive and retrospective study, with a quantitative approach, based on secondary data. A total of 337 records of women who went through a normal birth in a public maternity hospital in Bahia, inserted in a teaching hospital of the state health system in the city of Salvador.
The data source used was of the secondary type, from the maternity and birth care monitoring records that were filled out in the period from May to July 2015, and the Live Birth Declarations (BD) from the same period.
The monitoring records are filled out by the nursing team, more precisely by the nurses in the delivery room, and are subsequently attached to the Labor Monitoring Book. In the maternity ward of this study, the BD is also filled out by the nurse in the delivery room.
The data collection was carried out in September 2015, and was divided into two parts: in the beginning, the data were collected at the time of birth monitoring; and at the end of this phase, the collection of the BDs was started.
The study adopted four direct quantitative variables: number of previous pregnancies, number of previous normal deliveries, number of previous cesarean deliveries, and number of previous abortions. The age group was classified according to the groups - adolescents, young people and adults. The qualitative variables totaled nine, being distributed and categorized as described in Figure 1.
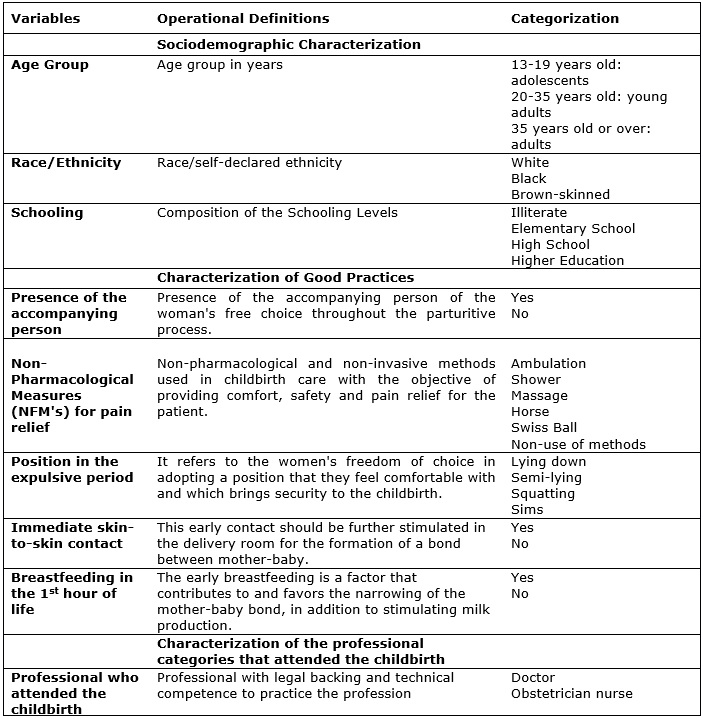
FIGURE 1: Operational definitions and categorization of study variables.
For the data processing, the statistical software Statistical Package for Social Sciences (SPSS) v.20 was used, extracting the absolute and relative frequency. Thus, the database was built, in which all the variables were considered.
According to the protocol established by the National Health Council and the recommendations of the Resolution No. 466/1213, the project was registered in the Brazil Platform, after authorization of the direction of the hospital, field of study. The project was approved by the Research Ethics Committee of the hospital organization, with a consolidated opinion No. 1,185,928/2015.
RESULTS
The sociodemographic profile and the four quantitative variables related to the obstetric profile of the women in the study are presented in Table 1.
TABLE 1: Sociodemographic and Obstetric Characterization of the Women in the Study. Salvador, 2015. N(337)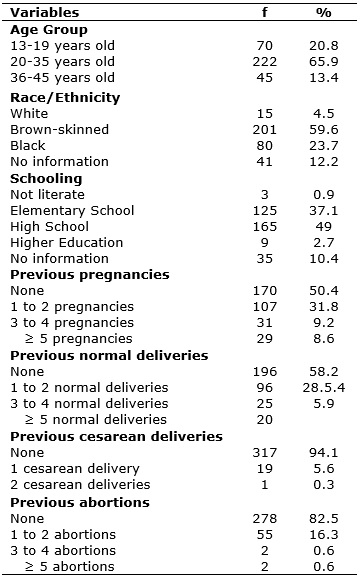
It is observed that more than half of the women in the study (65.9%) were between 20-35 years old. It is highlight that 20.8% of the women were in the 13-19 age group. The predominant race/ethnicity was black (brown-skinned and black), resulting in 83.3% of the women, being the white ethnicity composed by a minority - 4.5%. It should be highlighted that 12.2% of the records analyzed did not contain a race/ethnicity registry, as shown in Table 1.
There was a difference in the adherence of two good practices when compared to race/ethnicity. The first, regarding the presence of a companion, only 6.6% of the white women were not followed up, whereas among black women, the non-adherence reached 25.7%. The second, regarding the skin-to-skin contact, 28.5% of the white women did not have this contact, while that absence among black women reached the majority - 69%.
Regarding schooling, approximately half of the women studied until High School, 37.1% attended or were enrolled in Elementary School and only 2.7% attended Higher Education. There was no information on this variable in 10.4% of the records.
Regarding the obstetric profile, 50.4% of the women were primigravidae. Among the multigravida women, 31.8% had one to two pregnancies, 9.2% from three to four pregnancies, and 8.6% from five pregnancies. Regarding the type of delivery, 5.9% had a cesarean delivery, and 41.8% had a normal delivery, according to Table 1.
Regarding the occurrence of previous abortions, 16.3% of the women reported from one to two episodes, 0.6% suffered from three to four episodes, and 0.6% had five or more episodes, according to Table 1.
The data related to the good care practices to the childbirth and birth that are adopted by the study maternity are presented in Table 2.
TABLE 2: Characterization of the Good Practices adopted by the women of the study. Salvador, 2015. N(337)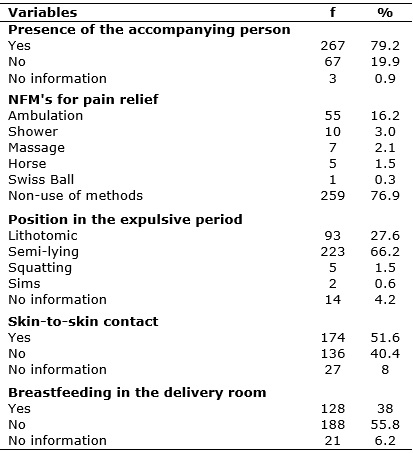
It is observed that most of the women had the freedom to choose to have their companion at the time of admission (79.2%), compared to 19.9% who were not accompanied. Regarding the use of non-pharmacological methods (NPM's) for pain relief, the study pointed to only 23.1% of use. The methods applied were: ambulation (16.2%), shower (3%), massage (2.1%), horse (1.5%) and Swiss ball (0.3%), as shown in Table 2.
The most adopted position by the women in the expulsive period was the semi-lying (66.2%), followed by the lithotomy position (27.6%). The squatting and Simms positions had 1.5% and 0.6%, respectively, according to Table 2.
Immediate skin-to-skin contact with the baby was made possible for 51.6% of the women. It should be highlighted that 7% of the records did not contain this information. As for the early breastfeeding, still in the delivery room, 55.8% did not breastfeed their babies in the first hour of life, while 38% adopted this practice. It is worth mentioning that 6.2% of the files that did not contain this information.
DISCUSSION
Sociodemographic and obstetric profile
Studies indicate that the age of the woman interferes in the maternal mortality, and those above 35 years old are considered as high risk, and other authors argue that the age should be associated with factors such as socioeconomic conditions14. In this study, the predominant age group is young adults, between 20-35 years old, which corresponds to the favorable age for gestation.
There was a higher percentage of women who had complete/incomplete high school. The instruction can ensure, even if indirectly, an increase in the possibilities to know and have access to safe and adequate information on the use of contraceptive methods, although it does not guarantee its use.
Also, most of the women in this study were black and brown-skinned, reaffirming the profile of users of the Unified Health System (SUS - Sistema Único de Saúde). In a study carried out in Recife, Brazil, whose objective was to characterize the racial inequalities in the mortality of black and white adult women, the risk of death of black women in relation to white women, due to pregnancy, childbirth and puerperium, was twice as high and, in the age group of 20 to 29 years old, four times greater. These findings reinforce the need to improve health surveillance and knowledge about racial inequalities in health.15
Good practices during childbirth and birth
Pregnancy should be treated as an expression of health, and birth as a physiological and natural process. Unnecessary interventions should be avoided, since there is a large quantity of evidences demonstrating that facilitating the natural process of birth to occur in accordance with its normal characteristics can lead to better maternal and perinatal outcomes. Unless deviations from the normality occur, verified through the maternal and fetal periodic controls, with continuous risk assessment, no intervention in this process is justified.1
The Survey Born in Brazil (Pesquisa Nascer no Brasil), considered the incidence of good obstetrical practices among women of low and high obstetric risk, since the incidence of interventions during labor and delivery was extremely high in both groups.9
From this perspective, the good practices listed for this study (presence of accompanying person, non-pharmacological methods for pain relief, freedom of choice of position, immediate skin-to-skin contact, and breastfeeding in the delivery room) presented varied use, and are analyzed next.
Presence of an accompanying person
In this study, 79.2% of the women were accompanied for some time during hospitalization. This result stands out when compared to the Survey Born in Brazil, in which 75% of the women had some type of companion during hospitalization.16 In addition, the National Health Survey, conducted in 2013, which shows that during the vaginal delivery only 58% of the women were accompanied by someone.17 Although the percentage found in this study was higher than others, this practice needs to be increasingly encouraged and supported by health institutions.
The satisfaction of the woman in the childbirth is strongly related to the presence of an accompanying person and the warm environment that is offered to her. This good practice is ensured by the Law No. 11,108, which guarantees the parturients the right to have an accompanying person during labor, delivery and immediate postpartum, within the SUS scope. 18
However, the insertion of this new character in the childbirth scenario leads to difficulties, especially when it comes to the partner, due to the lack of knowledge of his rights as a partner and father.19
It is known that there are obstacles that still prevent their full accomplishment, such as structural inadequacy and lack of resources, since the presence of the companion can generate costs. However, this should not be used as a barrier or impediment to the adherence to this practice. It is necessary that the health institutions adapt and offer a structure capable of accommodating the companions, guaranteeing and respecting this right of the woman. In this context, studies show that the parturients require continuous support during childbirth, and when this support comes from a family member or someone close to them, the women feel safer and happier. This is a way of qualifying and humanizing the care provided.20
Non-pharmacological methods for pain relief
Regarding non-pharmacological methods for pain relief, these should be offered to parturients since their admission to the unit for the better conduction of labor, and better perinatal outcomes. Its use is beneficial, since it offers alternatives and comfort measures, improving the delivery care.
The methods adopted by the maternity under study were ambulation, shower, massage, horse and Swiss ball. The Survey Born in Brazil shows a result of 26.7% regarding the use of non-pharmacological procedures9. In this study, only 23.1% of the women used one of these methods during their hospitalization. This result was below the expected, since its use is recommended by the WHO and it is an institution linked to the Stork Network.
According to a study carried out in São Paulo in 2009, which aimed to assess in an isolated and combined way the use of the sprinkler bath and perianal exercises using the Swiss ball, the results indicated that the associated application of such methods during the dilation phase are related to the reduced parturient pain and the promotion of maternal comfort.21
Free choice of position at the delivery time
Researchers assessed the use of good practices during labor and delivery in women at normal risk, and it has been found that during delivery, the lithonomic position reached more than 90% of the parturients.9 In this study, it was verified that the majority, 66.2%, of the women adopted the semi-lying position, despite the benefits that the vertical positions provide for the woman and the fetus.
In Western countries, it is observed that, according to cultural issues, there is a predilection for pregnant women to remain in a horizontal position most of the labor time. It is worth mentioning that the permanence in this position diminishes the effectiveness of the uterine contractions, considering that the compression of large blood vessels by the uterus occurs, which makes difficult the gas exchanges between the mother and the fetus. In addition, it contributes to a longer duration of delivery, often leading to obstetric interventions that cause pain and discomfort. 22
This reinforces the need to guide women in terms of free choice of birth position and benefits for better obstetric outcomes. Women need to have access to the correct information about the different positions they can adopt at birth, not just complying with norms and routines already established by the institution. Allowing the lithotomic position to be part of a rigid and immutable hospital routine is contrary to the humanization of care.
Immediate skin-to-skin contact
Another good practice that should be stimulated is the skin-to-skin contact right after birth. The skin-to-skin contact at birth was made possible for 51.6% of women. Health professionals need to be sensitized about the importance of establishing this contact, allowing the mother and the baby to enjoy the benefits brought by it.
This contact has several benefits: it helps in the adaptation to the extra uterine life, provides the early breastfeeding, controls the temperature, promotes an adequate sensory stimulation, and favors the father-mother-child bonding.23 It is presented as a safe, inexpensive and tested practice in benefits for the short and long term, both for mothers and children.24
For more than two decades, authors have already stated that, in the care model of humanized childbirth, the early contact between mother and child assumes a significant importance. This contact should be prioritized still in the delivery room, which contributes to the formation of bonds. 25 A convergent-care research carried out in a maternity hospital in the South Region of Brazil in 2009 showed that one of the interviewed women mentioned that they had received information about the skin-to-skin contact between mothers and children through friends and relatives, two women received information when they participated in groups of pregnant women, and three women were informed at the time of admission to the obstetric center.26
Thus, the importance of a qualified prenatal care is again highlighted. The nurse should guide the pregnant women about the benefits of good practices and their contributions to a good delivery and postpartum management. It is necessary that the woman gets to the maternity with the previous knowledge about these benefits, empowered and with greater autonomy.
Breastfeeding in the 1st hour of life
Regarding breastfeeding in the first hour of life, the majority of the puerperae, 55.8%, were not stimulated. It is important to highlight that no woman in this study have had any pathology that contraindicated breastfeeding. Thus, the percentage of non-adherence to this practice was relatively high. This result is compatible with the Survey Born in Brazil (2012), in which only 40.9% of the newborns were breastfed in the first hour of life.9
According to a Survey of Prevalence of Breastfeeding in Brazilian Municipalities, carried out in 2008, the prevalence of children under 1 year old who were breastfed in the first hour of life in the city of Salvador corresponded to 58.50%.27
Several authors assessed the good practices adopted and identified the variations in care for healthy newborns at term, in the delivery room and in the first hour of life; they found that, although the skin-to-skin contact was registered by almost 28% throughout Brazil, the proportions of breastfeeding in the delivery room were low, varying from 11.5% to 22.4% among the regions of the country. The South Region showed the highest rates of breastfeeding in the delivery room (22.4%).28
In addition, the Northeast is the region of the country with the largest contingent of hospitals with obstetric beds of the SUS, accredited by the Children Friendly Hospital (Hospital Amigo da Criança) initiative, and associated with the non-provision of the maternal breast in the delivery room. Only 41.3% of the healthy newborns in the Northeast were breastfed in the first hour of life, i.e., in addition to not breastfeeding in the delivery room, the newborn was also deprived of the breast in his first hour life.28
Although it is not part of the routine of many institutions, the incentive to breastfeeding is part of the good care practices to childbirth and birth and must be carried out. There are several benefits from breastfeeding to the baby, including the ease of eliminating meconium, protecting the gastrointestinal tract from infections, promoting the bond, decreasing the risk of jaundice, and reducing infant mortality rates.29
CONCLUSION
Among the good practices analyzed in the delivery and childbirth care, only the presence of an accompanying person and skin-to-skin contact occurred with the majority of women. The other good practices presented low adherence. It requires greater commitment from the institution and teams so that the good practices are effectively adopted and that the role of women in childbirth is respected.
The study is limited to the method used, since it only describes the facts registered in hospital documents, as well as presents the reality of obstetric care of only one maternity unit linked to the Stork Network. In addition, the sub-notification of health records also makes it impossible to fully visualize the local reality.
It is necessary to expand these good practices in maternity hospitals and to investigate the difficulties of their implementation, in order to identify and outline strategies to transpose them. However, it is expected that the results of this study may contribute to reveal the adoption of good practices and, along with other researches, subsidize the public policies to improve the obstetric care in the country.
It is also important for health professionals, especially nurses, to be made aware of the correct completion of health records, since the sub-notification limits the calculation of actual data.
Considering that the obstetric nursing has gained visibility in recent decades and its professionals have been trained and qualified to care for the natural childbirth, based on scientific evidence and in a humanized way, it is necessary for the nurse to value the complaints, expressions and feelings of the women, as this will enable the elaboration of a care plan that meets their particularities, guaranteeing comprehensive and quality care.
The humanized care should be centered on multiprofessional care, with a focus on ensuring the well-being of the women and newborn, taking into account social, cultural and racial aspects.
Every multiprofessional team must be aware of the importance to adhere to these good practices, since they ensure respect for the specifics of the users and effectively contributes to the qualification of care.
REFERENCES
1. Andrade MAC, Lima JBMC. O Modelo Obstétrico e Neonatal que defendemos e com o qual trabalhamos. In: Ministério da Saúde. Humanização do parto e do nascimento. Brasília (DF): Ministério da Saúde; 2014.P.19-47.
2. Nagahama EEI, Santiago SM. Práticas de atenção ao parto e os desafios para humanização do cuidado em dois hospitais vinculados ao Sistema Único de Saúde em município da Região Sul do Brasil. Cad. Saúde Pública. (Online) 2008; 24 (8): 1859-68.
3. Teles LMR, Américo CF, Pitombeira, HCS, Freitas LV, Damasceno, AKC. Parto acompanhado na perspectiva de quem o vivencia. Rev. enferm. UFPE on line. 2010; [citado em 20 maio 2016] 4(2): 498-503. Disponível em: file:///C:/Users/Alexandre/Downloads/6182-11112-1-PB%20(1).pdf
4. Moura FMJSP, Crizostomo CD, Nery IS, Mendonça RCM, Araujo OD, Rocha SS. A humanização e a assistência de enfermagem ao parto normal. Rev. bras. enferm. (Online) 2007; 60(4): 452-55.
5. Vargens OMC, Reis CSC, Nogueira MFH, Prata JA, Silva CM, Progianti JM. Tecnologias não-invasivas de cuidado de enfermagem obstétrica: repercussões sobre a vitalidade do recém-nascido. Rev. enferm. UERJ. 2017; 25:1-7.
6. Carvalho EMP, Göttems LBD, Pires MRGM. Adesão às boas práticas na atenção ao parto normal: construção e validação de instrumento. Rev.Esc. Enferm. USP. 2015; 49(6):890-98. 7.Vieira MJO, Santos AAP, Silva JMO, Sanches METL. Assistência de enfermagem obstétrica baseada em boas práticas: do acolhimento ao parto. Rev. eletrônica enferm. (Online). 2016; [citado em 15 dez 2016]; Disponível em: http://dx.doi.org/10.5216/ree.v18.36714
8. Cecatti JG, Calderón IMP. Intervenções benéficas durante o parto para a prevenção da mortalidade materna. Rev. Bras. Ginecol. Obstet. 2005; 27 (6): 357-65.
9. Leal MC, Pereira, APE, Domingues RMSM, Theme MMF, Dias MAB, Pereira MN, Bastos MH, Gama SGN. Intervenções obstétricas durante o trabalho de parto e parto em mulheres brasileiras de risco habitual. Cad. Saúde Pública. (Online)2014; 30 (1): 17-32.
10. Ministério da Saúde (Br). Secretaria Executiva. Humaniza SUS. Política Nacional de Humanização. Brasília (DF): Ministério da Saúde, 2004.
11. Ministério da Saúde (Br). Secretaria Executiva. Programa Humanização do parto Humanização no pré-natal e nascimento, Brasília: Ministério da saúde, 2002.
12. Ministério da Saúde (Br). Portaria MS/GM nº 1.459, 24 de junho de 2011. Institui no âmbito do Sistema Único de Saúde –SUS- a Rede Cegonha. 2011 [citado em 13 set 2016]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011.html
13. Ministério da Saúde (Br). Conselho Nacional de Saúde. Resolução nº 466, de 12 de dezembro de 2012. Aprova as diretrizes e normas regulamentadoras de pesquisa envolvendo seres humanos. [acesso em: 13 setembro 2015]. Disponível em: http://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf
14. Soares VMN, Schor N, Tavares CM. Vidas arriscadas: uma reflexão sobre a relação entre o número de gestações e mortalidade materna. Rev. Bras. Crescimento Desenvolv. Hum. 2008; 18 (3): 254-63.
15. Santos SM, Guimarães MJB, Araujo TVB. Desigualdades raciais na mortalidade de mulheres adultas no Recife, 2001 a 2003. Saude Soc . 2007; 16 (2): 87-102.
16. Diniz, CSG, Orsi E, Domingues RMSM, Torres JA, Dias MAB, Schneck CA, Lansky S, Teixeira NZF, Rance S, Sandall J. Implementação da presença de acompanhantes durante a internação para o parto: dados da Pesquisa Nacional Nascer no Brasil. Cad. Saúde Pública. (Online) 2014; 30 (1): 140-53.
17. Intituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde 2013: Ciclos de vida: Brasil e grandes regiões/ IBGE, Coordenação de Trabalho e Rendimento. 2015; 36-44. [citado em 18 out 2016] Disponível em: http://biblioteca.ibge.gov.br/visualizacao/livros/liv94522.pdf
18. Governo Federal (Br). Lei nº 11.108 de 7 de Abril de 2005. Do subsistema de acompanhamento durante o trabalho de parto, parto e pós-parto imediato. Brasília, (DF); Senado Federal; 2005. [citado em 03 abr 2016]. Disponível em: http://www3.dataprev.gov.br/sislex/paginas/42/2005/11108.htm
19. Carvalho IS, Carvalho CFS, Enders BC, Brito RS. A participação do homem durante o nascimento do filho: vídeos do Youtube. Rev. enferm. UERJ, 2017; 25:1-7.
20. Dodou HD, Rodrigues DP, Guerreiro EM, Guedes MVC, Lago PN, Mesquita NS. A contribuição do acompanhante para a humanização do parto e nascimento: percepções de puérperas. Esc. Anna Nery Rev. Enferm. 2014; 18(2): 262-9.
21. Miquelutti MA. Avaliação da posição vertical durante o trabalho de parto em nulíparas [dissertação de mestrado] Campinas (SP): Universidade Estadual de Campinas; 2006.
22. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Atenção à saúde do recém- nascido: guia para os profissionais de saúde. Brasília (DF): Ministério da Saúde, 2011. 23.Klaus MH, Kennell JH. Pais/bebê a formação do apego. Porto Alegre (RS) Ed Artes Médicas; 1993.
24. Sampaio ARR, Bousquat A, Barros C. Contato pele a pele ao nascer: um desafio para a promoção do aleitamento materno em maternidade pública no Nordeste brasileiro com o título de Hospital Amigo da Criança. Epidemiol. Serv. Saude. 2016; 25(2):281-90.
25. Matos TA, Souza MS, Santos EKA, Velho MB, Seibert ERC, Martins NM, et al. Contato precoce pele a pele entre mãe e filho: significado para mães e contribuições para a enfermagem. Rev. bras. enferm. (Online)2010; 63: 998-1004.
26. Ministério da Saúde (Br). Secretaria de Atenção à Saúde. Pesquisa de Prevalência de Aleitamento Materno em Municípios Brasileiros. Brasília (DF): Ministério da Saúde; 2010. 27.Moreira MEL, Gama SGN, Pereira APE, Silva AAM, Lansky S, Pinheiro RS, Gonçalves AC, Leal MC. Práticas de atenção hospitalar ao recém-nascido saudável no Brasil. Cad. Saúde Pública. (Online) 2014; 30: 128-39.
28. Modes PSSA, Gaíva MAM, Patricio LFO. Assistência ao recém-nascido no nascimento: a caminho da humanização? Rev. bras. enferm. (Online) 2010; 9(1).
29. Bueno KCVN. A importância do aleitamento materno exclusivo até os seis meses de idade para a promoção de saúde da mãe e do bebê. Belo Horizonte (MG): Universidade Federal de Minas Gerais. 2013; 1-28.