(*) Adjusted for age, ethnicity, schooling and living conditions.
ORIGINAL RESEARCH
Health Belief Model and cervical cancer screening: assessing vulnerabilities
Ricardo de Mattos Russo RafaelI, Anna Tereza Miranda Soares de MouraII
I
Nurse. PhD in Science. Professor at the State University of Rio de Janeiro
and Estácio de Sá University. Rio de janeiro Brazil. E-mail:
prof.ricardomattos@gmail.com
II
Doctor. PhD in Public Health. Professor at the State University of Rio de
Janeiro and Estácio de Sá University. Rio de janeiro Brazil. E-mail:
annaterezam.smoura@gmail.com
DOI: http://dx.doi.org/10.12957/reuerj.2017.26436
ABSTRACT
Objective: to evaluate the risk factors for inadequate cervical cancer screening using the Health Belief Model. Method: This case-control study involved interviews of 640 Family Health Strategy users, between 2012 and 2013. Data were collected using a multidimensional, structured instrument and subsequently subjected to multivariate analysis. The study was approved by the ethics committee (protocol number 01724512.6.0000.5259). Results: one important risk factor for screening was the perception of barriers (OR 16.7; 95% CI: 9.2/30.1), the effect of which was modified by two dimensions: susceptibility and severity (OR: 22.5; 95% CI: 11.4/44.5). Conclusion: the results underscore the need for evaluation of client demands to incorporate subjective aspects relating to users' perceptions of, and feelings towards, cancer screening, especially in order to understand the factors that increase absenteeism from this practice.
Keywords: Uterine cervical neoplasms; vaginal smears; health services accessibility; primary health care.
INTRODUCTION
Changes in living standards in recent decades have contributed to the acceleration of the demographic and epidemiological transition in several countries. The heavy burden of infectious diseases was replaced by non-infectious diseases and illnesses, which became the first causes of mortality rates1. Cancer is part of this group of diseases; it is estimated that by 2025, more than 20 million new cases will be registered worldwide, accounting for about 70.0% of deaths in developing countries2. In Brazil the estimates are similar, pointing to the occurrence of 600 thousand new cases in the biennium 2016-17. It is worth mentioning that cervix cancer continues to represent an important disease among the female population, occupying the first position in incidence and mortality3.
Advances in the knowledge on the subject have made it possible to identify cervical cancer characteristics related to prevention, early detection and treatment, increasing the possibilities of cure and favorable prognosis. The combination of actions aimed at prevention of human papillomavirus (HPV) infections and systematic tracking of cancer precursor lesions has been pointed out as the main measure to control the disease in Brazil. There is a broad theoretical framework that points to the lower probability of developing the disease when oncotic colpocytology examination is performed every three years in women between 25 and 64 years of age, and when cervical lesions within one year after two negative and subsequent tests are absent4.
Based on this recommendation, the Ministry of Health has increased women's access to screening techniques over the years, especially through the Family Health Strategy (FHS) and other Primary Health Care (PHC) organs. It is believed that the work dynamics of this level of attention may favor health surveillance practices and the formulation of strategies capable of adapting the diverse actions of the teams to the needs of the population5,6.
Despite the improvement in the conditions of access to oncotic colpocytology, many women are still excluded from the early capture process, with inadequate interval of examination, that is, with screening intervals of more than three years4. Problems related to the structure of the health services and team work process, besides the understanding of the disease and its forms of prevention, may be contributing to this inadequacy. Factors related to the formation of self-care habits may also interfere with individual health practices, increasing the barriers to access7.
Several are the theoretical models that support the understanding of the motivation to adhere to adequate screening, mainly through explanations regarding the health network availability and sociodemographic aspects of women. In this perspective, the Health Belief Model proposes that the incorporation of preventive behaviors against illnesses is based on individual perceptions in four different dimensions. The first two address the perception of susceptibility to illness and of the severity of the disease, that is, to which extent the subjects perceive the possibility of becoming ill and their understanding of the impact of the event on their lives. The other dimensions refer to perceptions about the benefits and barriers of adopting a preventive behavior8,9.
Bearing in mind that the interaction between these dimensions may influence the use of health services, especially the colpocytological examination, this study had as objective to evaluate the risk factors for the inadequacy of cervical cancer screening based on the Health Belief Model.
LITERATURE REVIEW
There has been an increasing production of studies aiming to understand the low coverage of cervical cancer screening in some regions of the country, with at least two constructs involved in this process: people's perception of access and the use of health services. Access is understood as a varied and complex set of factors responsible for the degree of ease or difficulty that people have to obtain care, and may result from the characteristics of individuals and/or of the service itself, the existence of materials and qualified professionals, the offer of exams, among others10.
In turn, use is closely related to the interaction between people and the various organizational characteristics, either by elements of access, the dynamics of the teams' performance and even the empathy built between users and professionals. In this case, a person's decision to use a health service will be mediated by cultural, political and health perceptions of the social group to which he or she belongs, building the individual perception about preventive health behaviors11.
Among the various theoretical models that study the phenomena of access and utilization of services, particularly led by preventive health behaviors, there is the Belief Model proposed by North American social psychologists in the 1950s12. The Model takes as basis the beliefs and perceptions of people regarding health risks, understanding that the decision whether or not to adopt a preventive behavior will be mediated by four perceived dimensions: gravity, susceptibility, benefits and barriers9.
The perception about gravity develops from the feelings towards the disease that is the target of the preventive behavior, as potential generator of pain, disability and death, and their impacts on daily life - family, social and work relations. Susceptibility - also called vulnerability - is the dimension that responsible by the extent to which people perceive their potential illness, that is, how much they see the probability of getting sick at some point of their life. The last two dimensions are responsible for the sometimes unconscious balance of costs and effectiveness, benefits and barriers/difficulties aimed at adopting preventive practices - directly and indirectly related to access and use of health services8,9.
METHODOLOGY
This is a case-control study anchored in the project Barriers in the access for cervical cancer screening: a study on the relationships of intimate violence and abusive use of alcohol in Family Health users , which was developed in the municipality of Nova Iguaçu, metropolitan region of the State of Rio de Janeiro13. We selected the central region, which concentrates most of the social equipment and which has five basic health units, totaling 10 teams. The smallest unit, with only one team, was selected for the pilot study, leaving the territory of the other nine destined for fieldwork and data collection (population registered: 26,025 inhabitants).
The source-population of the study comprised the group of women aged between 25 and 64 years, the target age group of the programs for the control of cervical cancer4. The inclusion criteria were: to be resident in the FHS area and to have an intimate relationship for one year, necessary to evaluate the occurrence of violence between partners, one of the interests of the Project base of this study. Women with a previous diagnosis of uterine cancer and other gynecological diseases requiring periodic control were excluded.
Women who had inadequate screening - those who did not undergo colposcopy in the three years prior to data collection - were considered as cases. Women who attended the health unit during the data collection period and who had undergone at least one examination in the last three years were classified as controls. The sample size was calculated considering odds ratio (OR) 2.0, 95% confidence interval (95% CI), power of 80.0% and a ratio of one case to three controls, with a final sample of 640 women, 40 cases and 120 controls for each selected unit. Opportunistic recruitment was used as sample composition strategy, applying the selection criteria as the women accessed the health units.
The interviews were conducted by four nursing professionals under the supervision of the authors. Interviewers received training on standardization of interviews, and received a manual containing pertinent information on the data collection instrument. The interviews took place in the period from November 2012 to June 2013 in a private place within the health units and before the women entered the doctor's office and other services. First, the eligibility forms were applied and then the collection instruments. The mean interview time was 40 minutes, resulting in four daily interviews per interviewer.
A structured and multidimensional instrument was used. Sociodemographic characterization included age, color/ethnicity, schooling, marital status, all present in the National Household Sample Survey (NHSS)14. The economic classification of the sample was made based on the criteria proposed by the Brazilian Association of Research Companies (BARC), stratifying classes A/B, C and D/E15. Housing conditions were assessed by the specific score, considering the number of people in the household, the type of material predominant on the house floor, sewage system and garbage collection16.
The evaluation of access and use of screening services was based on the Health Belief Model, using the Champion's Health Belief Model Scale (CHBMS), validated and adapted for use in cancer research in Brazil, and recently used in studies aimed at the screening of cervical cancer8,9,17-19. The instrument has 29 items subdivided into four scales that evaluate the respondent's perception of: susceptibility to illness, severity of the disease, benefits and barriers to preventive practices. The scale was considered positive in case of response to at least one item by the participant. The affection of the dependent variable occurred through the question: Have you done any preventive examination (Papanicolau examination) in the last 3 years?
The database was built in the Epidata 3.1 software using a double entry technique in 20% of the applied instruments. Data analysis and statistical analysis were performed using the Stata SE 13 software. The socio-demographic characteristics and the four Belief Model dimensions were analyzed using the dependent variable, calculating the prevalence, gross OR and 95% CI. Items that presented p-values below the cut-off point (p-value 0.25) were included in the multivariate model, which used a non-conditional logistic regression technique and calculated the adjusted ORs. The Likelihood Ratio Test was used to evaluate the p-values, classifying them as statistically significant when the result was ≤ 0.05 and borderline when in the range of 0.05 to 0.1.
Finally, a conditional logistic regression model was performed to evaluate the interactions with possible effect modifier variables. It should be noted that the regression model was forced into the variables that belonged to the Belief Model and presented p-values below the cut-off point. This measure aimed to ensure the testing of all items involved in the postulates of this study.
Free and Informed Consent Terms were signed by all respondents and the study was approved by the Research Ethics Committee under number 01724512.6.0000.5259. All participants were instructed on the screening of cervical cancer and, when necessary, it was possible to schedule gynecological consultations.
RESULTS AND DISCUSSION
The study sample showed a predominance of women aged over 40 years - 383 (59.8%), white and brown - 359 (35.1%), with less than eight years of schooling - 370 (57.8%), married - 355 (55.5%), belonging to economic class C - 493 (70.7%) and living in poor housing conditions - 539 (84.3%). The bivariate analysis between the sociodemographic characteristics showed a statistically significant association between the inadequacy of the screening test and age group (p-value < 0.001) and schooling (p-value = 0.002). It should be noted that the variables ethnicity (p-value = 0.202) and housing conditions (p-value = 0.195) were included in the final regression model because they presented p-values below the cutoff point, as reported in the methodology.
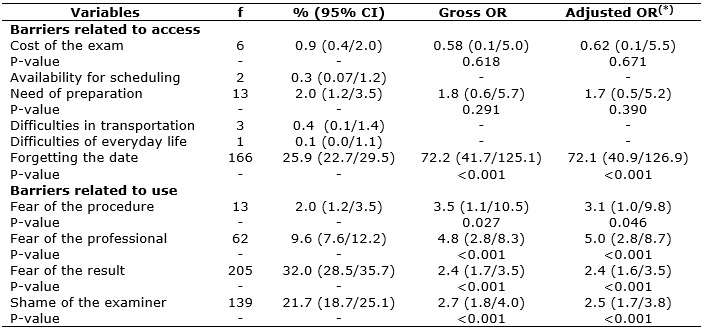
The analysis of the factors hindering the colpocytological examination is presented in Table 1. Among the items assessed as access barriers, forgetfulness presented an adjusted OR of 72.1 (95% CI: 40.9/126.9, p-value < 0.001). All variables associated with the use of services that were related to fear or shame presented statistical significance.
TABLE 1:
Distribution, bivariate analysis and adjusted model of independent
variables (barriers related to access and use of the examination) and
inadequacy of cervical cancer screening among Family Health Strategy
(*)
Adjusted for age, ethnicity, schooling and living conditions.
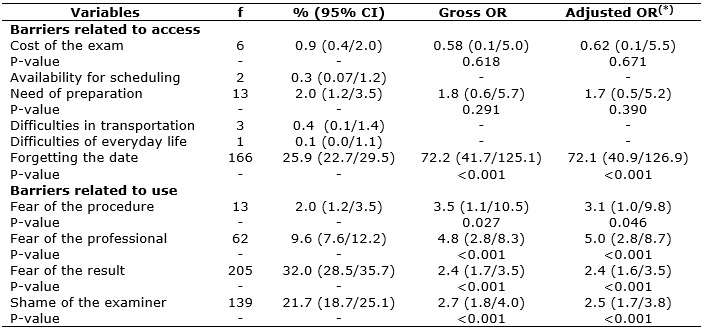
The prevalence and the respective ORs for the dimensions of the Health Belief Model are shown in Table 2. A statistically significant relationship was found in the dimensions of perceived barriers and benefits, representing, respectively, a risk factor (OR 16.1; 95% CI: 9.0/28.7, p-value < 0.001) and protective factor (OR 0.1, 95% CI: 0.04/0.1, p-value < 0.001). There were no significant changes in the magnitude of the ORs after adjustment, rejecting the presence of confounding variables in almost all the variables tested.
TABLE 2:
Distribution, bivariate analysis and adjusted model of independent
variables (dimensions of the Health Belief Model) and inadequacy of
cervical cancer screening in Family Health Strategy users. Nova Iguaçu/RJ,
Brazil, 2013. (N = 640)

(*)
Adjusted for age, ethnicity, schooling and living conditions.
The results of the final model using conditional logistic regression are shown in Table 3. The absence of perception of susceptibility raises the risks imputed by the barriers, which increases with the positivity in the scale of gravity. The perception of benefits of the exam presented lower OR value, when compared to models 1 and 2.
TABLE 3
- Conditional regression model between the perception about the barriers to
use and access of health services and the other dimensions of the Health
Belief Model among women covered by the Family Health Strategy. Nova
Iguaçu/RJ, Brazil, 2013. (N = 640)
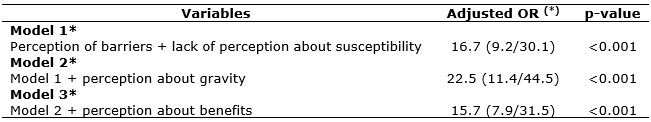
(*)
Adjusted for age, ethnicity, schooling and living conditions.
Studies on factors that prevent or hinder the realization of cervical cancer screening are not recent and are often considered in the Brazilian and world literature20,21. There is also growing production of knowledge about the mediators of use and access to health services18,22. However, the risk relationships between the Health Belief Model dimensions and the inadequacy of the examinations - in this case, inadequate screening of cervical cancer - represents a novelty to Brazil, an aspect clarified by the methodological option of this study.
The barriers to the examination were presented in two main groups: those related to access to and to the use of services. The first group is represented by a variety of factors that refer to the ease - or difficulty - that the users experience to obtain care22. Although the term access can be defined more broadly than the one investigated in this research, the Health Belief Model focuses its evaluation on issues that have a certain subjectivity in the users' perception, such as the cost, the need for preparation and the difficulties with scheduling and transportation9,17.
The expressive magnitude of forgetting the scheduled date (OR 72.1) calls for the need to reflect on the offer of colpocytological examination. The literature indicates that regions where cervical cancer screening programs are predominantly opportunistic have high rates of incidence of this disease4,21. It seems that the captation occurring exclusively during the users' attendance to the unit is not ideal, because the life dynamics of assumed by many women - with overlapping household tasks, family care and work activities – may increase the chances of their forgetting the appointment. The presence of the women in the unit does not guarantee a protected moment for their self-care. They are often involved with the health of their whole family. The schedules of exams on these occasions do not ensure that the women will come back at the scheduled date, and thus they will be at greater chance of becoming ill.
In addition to the structural barriers hindering the examinations, individual and psycho-emotional aspects can also make it difficult to use services22, despite the facilitated access proposed by the FHS. The findings showed a greater risk between the barriers related to the use of services and the (in) adequacy of cervical cancer screening, with emphasis on feelings of fear and shame. Fear of the procedure (OR: 3.1), the professional (OR: 5.0), the result of the test (OR: 2.4), and shame (OR: 2.5) have already been identified as risk factors for inadequacy of screening in other studies on the theme23-26.
Although negative feelings related to preventive behaviors such as in the case of colpocytological examinations are experienced in a particular and individual manner, you can also be influenced by the culture present in the different social groups frequented by women. There are many ways to experience fear - from the procedure to the result itself - and this may be associated with the negative experiences that circulate in the female universe, enhancing the risks of inadequate screening. Furthermore, fear of cancer and its repercussions also bring ideas of long-term and painful treatments, altered self-image, and even death, contributing to negative impressions about the possible diagnosis18,27.
Discussions about gender need to be contemplated. They can permeate these emotions, since idealized female behaviors are based on predominantly patriarchal social constructs, imposing mechanisms of control over the sexuality of women and their bodies. It is possible that these feelings be gradually naturalized, stabilized and transformed into barriers that impede the use of preventive practices and health care. Thus, the fear and shame reported by some women may be related to obstacles and conflicts related to the manipulation of their body by another person, especially when the professional is male28. The FHS provides a reference team for assigned territories, which does not appear to be sufficient. To assume a flexible posture that guarantee the choice of the examiner by the user would be essential for the promotion of true autonomy, with consequent improvement of conditions to use and access. The territory, understood as essentially dynamic, must permeate the interdisciplinary debate within the teams, used to produce health and transform the everyday life, and not to serve as a possible barrier to access and use of services29.
The results show that the combination of levels of perception of the users about susceptibility and gravity can also increase the risks implied by the barriers, further favoring the inadequacy of screening. The lower perception about their own vulnerability is a risk factor for access and use, since women do not see themselves at risk of becoming ill, even without the periodic examinations. Negative feelings about the perception of the seriousness of the disease also seem to prevent or hinder the search for health services, acting as an important risk factor. This is in line with the identifed barriers related to fear of the results of the examination22.
On the other hand, understanding the benefits of adopting preventive behaviors tends to reduce these risks (OR 0.1); women eventually mobilize their available resources to avoid becoming ill. Even when this perception is associated with bad experiences related to the examination, the risk of inadequacy was lower (OR 15.7). In this perspective, the development of strategies anchored in the participation of the community can also help in the construction of strategies to improve the coverage, such as flexibility of schedules and adequacy of the dynamics of teams' functioning20,22.
The adoption of educational practices that may allow reflections on the Health Belief Model dimensions would also be an alternative to reduce the perceived barriers, increasing the possibilities for users to adopt preventive behaviors30. The qualification of the dynamics of health teams may minimize the negative feelings studied here, considering that this level of attention has important attributes that enable improved access to users, such as the first contact and the longitudinality and coordination of care, typical of this level of attention.
CONCLUSION
The pioneering character of a study that focuses on the constructs presented here has the responsibility of collaborating with the production of novel knowledge for the area. The methodological design presents gaps that deserve to be addressed in future works; importantly, the interpretation of the results is carried out in light of these limitations. The first limitation is related to the allocation of respondents in the case and control groups, which took place through selection of users in the health units. We believed that the magnitude of the risks will prove to be even greater, especially those regarding barriers to access, when participants be located through home surveys.
Another limitation is associated with the selection of women who had intimate relationships for at least one year, which excludes single women or women without a single partner, who may present other specific characteristics that were not contemplated in this investigation. Finally, the instrument used, which is the only one culturally adapted to Brazil, does not present specific validation for investigation of phenomena related to cervical cancer, although it has already been used in two large studies in the area.
In any case, it was possible to understand how the Health Belief Model relates to the (in)adequacy of the cervical cancer screening. The main risk factors to access/use of the screening services were identified, namely: forgetfulness of the scheduled date, shame of the examiner, and fears related to the professional, the procedure and the result of the examination. Allying this knowledge with the interaction promoted by the perception about susceptibility, gravity of the disease and benefits of the screening may qualify the programming of health services, especially in cases of missing users.
We could observe that the set of variables investigated deserves to be expanded to include other factors involved in the possible causality of inadequate screening. Further works with designs allowing the investigation of these causal relationships, helping to overcome the gaps presented here are encouraged. Research with different subgroups of women also seems to be necessary for a better understanding of interactions with this outcome.
REFERENCES
1.Araújo ID. Epidemiological polarization in Brazil. Epidemiol Serv Saúde [Internet]. 2012 [cited on May 5, 2016]; 21(4): 533-8. Available at: http://scielo.iec.pa.gov.br/scielo.php?script=sci_arttext&pid=S1679-49742012000400002
2.Stewart EW, Wild CP, editors. World Cancer Report 2014. Lyon: International Agency for Research on Cancer; 2014.
3.Cancer Nacional Institute [Internet]. Estimate 2016: incidence of cancer in Brazil. Rio de Janeiro: INCA; 2016. [cited on May 5, 2016]. Available at: http://www.inca.gov.br/bvscontrolecancer/publicacoes/edicao/Estimativa_2016.pdf
4.Cancer Nacional Institute [Internet]. Brazilian guidelines for the screening of cervical cancer. Rio de Janeiro: INCA; 2011. [cited on Jun 10, 2015]. Available at: http://www1.inca.gov.br/inca/Arquivos/Diretrizes_rastreamento_cancer_colo_utero.pdf
5. Ministry of Health [Internet]. National Policy of Primary Care. Brasília (DF): Department of Primary Care; 2012. [cited on Mar 3, 2013]. Available at: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf
6.Rafael RMR, Moura ATMS. Exposure to cervical cancer risk factors in the Family Health Strategy of Nova Iguaçu, Rio de Janeiro, Brazil. Cad saúde colet. [Internet]. 2012 [cited on Jun 10, 2016]; 20(4): 499-505. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-462X2012000400014
7.Silva MAS, Teixeira EMB, Ferrari RAP, Cestari MEW, Cadelli AAM. Factors related to non adherence to the Pap smear examination. Rev Rene [Internet]. 2015 [cited on Mar 3, 2016]; 16(4): 532-9. Available at: http://www.revistarene.ufc.br/revista/index.php/revista/article/viewFile/2025/pdf
8.Coleta M. Scales for measurement of health beliefs: construction and validation. Psychological Evaluation [Internet]. 2003 [cited on June 10, 2016]; 2(2): 111-22. Available at: http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1677-04712003000200003
9.Rosenstock IM. The health belief model and preventive health behavior. Health educ monographs. 1974;2(4):354-87.
10.Anchez RM, Ciconelli RM. Concepts of access to health. Rev Panam Salud Publica [Internet]. 2012 [cited on Nov 21, 2016]; 31(3): 260-8. Available at: http://www.scielosp.org/pdf/rpsp/v31n3/12.pdf
11.Assis MMA, Jesus WLA. Access to health services: approaches, concepts, policies and analysis model. Cien Saude Colet [Internet]. 2012 [cited on Nov 20, 2016]; 17(11): 2865-75. Available at: http://www.scielo.br/pdf/csc/v17n11/v17n11a02.pdf
12.Barletta JB, Gennari MS, Cipolotti R. The cognitive-behavioral perspective of the psychosocial aspects that interfere in the quality of the doctor-patient relationship. Psicol rev. (Belo Horizonte) [Intenet]. 2011 [cited on Nov 21, 2016]; 17(3): 396-413. Available at: http://pepsic.bvsalud.org/pdf/per/v17n3/v17n3a05.pdf
13.City Hall of Nova Iguaçu [Internet]. PMNI, 2011 [cited on Apr 25, 2011]. Available at: http://www.novaiguacu.rj.gov.br/
14.Brazilian Institute of Geography and Statistics. National Household Sample Survey: survey questionnaire. Rio de Janeiro: IBGE; 2011.
15.Brazilian Association of Research Companies [Internet]. Criteria of Economic Classification Brazil. São Paulo: ABEP, 2015; [cited on Jun 10, 2016]. Available at: http://www.abep.org/codigos-e-guias-da-abep
16. Reichenheim ME, Harpham T. Intra-community profile of nutritional deficiency: a study of under-5 children in a low-income community in Rio de Janeiro. Rev Saúde Pública [Internet].1990 [cited on Oct 3, 2010]; 24:69-79. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89101990000100011
17.Santos E. Health Belief Model in relatives of colorectal cancer patients. São Paulo: Post-Graduation Program in Sciences of Fundação Antônio Prudente; 2008.
18.Rafael RMR, Moura ATMS. Barriers to oncotic colposcopy: a household survey in the area of Family Health coverage of Nova Iguaçu, Rio de Janeiro, Brazil. Cad Saúde Pública [Internet]. 2010 [cited on Jun 10, 2016]; 26(5): 1045-50. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2010000500026
19.Rodrigues DE, Moreira KFA, Oliveira TS. Barriers to prevention of cervical cancer in the city of Porto Velho, Rondônia, Brazil. Invest educ enferm [Internet]. 2016 [cited on Nov 19, 2016]; 34(1): 59-67. Available at: http://www.scielo.org.co/pdf/iee/v34n1/v34n1a07.pdf
20.Giordano VR, Thuler LCS, Azevedo e Silva G. Adherence to screening for cervical cancer among women from communities assisted by the Baixada Fluminense Family Health Strategy, Rio de Janeiro, Brazil. Rev Bras Ginecol Obstet [Internet]. 2014 [cited on Nov 05, 2015]; 36(5): 198-204. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-72032014000500198
21.Tranberg M, Larsen MB, Mikkelsen EM, Svanholm H, Andersen B. Impact of opportunistic testing in a systematic cervical cancer screening program: a nationwide registry study. BMC Public Health [Internet]. 2015 [cited on Feb 17, 2016]; 15: 681. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4508820/
22.Ma GX, Gao W, Fang CY, Feng Z, Ge S, Nguven JA. Health Beliefs Associated with Cervical Cancer Screening Among Vietnamese Americans. J Womens Health (Larchmt) [Internet]. 2013 [cited on Aug 26, 2015]; 22(3): 276-88. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601630/
23.Travassos C, Martins M.. A review on the concepts of access and use of health services. Cad Saúde Pública [Internet]. 2004 [cited on Jul 31, 2011]; 20(suppl.2): 190-8. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2004000800014
24.Correio KDL, Ramos AIG, Santos RLG, Bushatsky M, Correio MBSCB. Control of cervical cancer: actions developed by nurses in light of the discourse of the collective subject. J Res: Fundam Care Online [Internet]. 2015 (cited on June 10, 2016); 7(2): 2425-39. Available at: http://www.seer.unirio.br/index.php/cuidadofundamental/article/view/3780/pdf_1557
25.Pimentel AV, Panobianco MS, Almeida AM, Oliveira ISB. Perception of vulnerability among women with advanced cervical cancer diagnosis. Text context - enferm. [Internet]. 2011 [cited on Sep 19, 2012]; 20(2): 255-62. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-07072011000200006
26.Nascimento LC, Nery IS, Silva AO. Women's daily knowledge about the prevention of cervical cancer. Rev Enferm UERJ [Internet]. 2012 [cited on Nov 19, 2016]; 20(4): 476-8. Available at: http://www.e-publicacoes.uerj.br/index.php/enfermagemuerj/article/view/4813/3537
27.Aguilar RP, Soares DA. Barriers to the Papanicolau examination: perspectives of users and professionals of the Family Health Strategy of the city of Vitória da Conquista-BA. Physis Revista de Saúde Coletiva [Internet]. 2015 [cited on May 4, 2016]; 25(2): 359-79. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-73312015000200359&lng=en&nrm=iso&tlng=pt
28.Rico AM, Iriart JAB. "There are women, there is preventive care": meanings of the preventive practices of cervical cancer among women from Salvador, Bahia, Brazil. Cad Saúde Pública [Internet]. 2013 [cited on Apr 30, 2014]; 29(9): 1763-73. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2013000900016
29.Silva AB, Pinho LB. Territory and mental health: conceptual contributions of geography to the psychosocial field. Rev Enferm UERJ [Internet]. 2015 [cited on June 7, 2017]; 23(3): 420-4. Available at: http://www.facenf.uerj.br/v23n3/v23n3a21.pdf
30.Hanaa AAY, Hend AS. Effect of self learning package based on Health Belief Model in cervical cancer prevention among female university students. J of Nursing and Health Science [Internet]. 2014 [cited on Jun 10, 2016]; 3(6): 77-88. Available at: http://iosrjournals.org/iosr-jnhs/papers/vol3-issue6/Version-4/N03647788.pdf