ORIGINAL RESEARCH
Nurses' role in radiation therapy services
Nauã Rodrigues de SouzaI; Magaly BushatskyII; Eudanusia Guilherme de FigueiredoIII; Jessica Thamires da Silva MeloIV; Carmina Silva dos SantosV; Isabel Cristina Ramos Vieira SantosVI
I
Nurse. Master student, Graduate Nursing Program, University of Pernambuco,
State University of Paraíba. Pernambuco, Brazil. E-mail: nauan_1@hotmail.com
II
Nurse. PhD in Nursing. Professor at the Nossa Senhora das Graças Faculty of
Nursing, University of Pernambuco. Pernambuco, Brazil. E-mail: magab@hotlink.com.br
III
Nurse. Specialist in Oncology at the Oswaldo Cruz University Hospital,
University of Pernambuco. Pernambuco, Brazil. E-mail: eudanusiagf@gmail.com
IV
Nurse. Resident in Traumatology and Orthopedics at the Getúlio Vargas
Hospital. Pernambuco, Brazil. E-mail: jes-melo@hotmail.com
V
Nurse. PhD in Nutrition. Professor at the Pernambuco Health College,
Pernambuco, Brazil. E-mail: carminassantos@gmail.com
VI
Nurse. PhD in Nursing. Professor of the Graduate Nursing Program,
University of Pernambuco, State University of Paraíba, Brazil. E-mail: tutornad@yahoo.com.br
DOI: http://dx.doi.org/10.12957/reuerj.2017.26130
ABSTRACT
Objective: to ascertain nurses' role in radiotherapy services. Method: in this quantitative, descriptive, cross-sectional study, data were collected by structured questionnaire from a sample of eight nurses, from June to July 2015, and analyzed using descriptive statistics. Results: it was found that nurses are not restricted to care alone, but supervise nursing staff, monitor the work process, prepare action plans, select materials and equipment, and schedule appointments. We also observed that nursing appointments were important in individualizing care and effecting patient treatment. Conclusion: for the radiotherapy service to function properly requires a trained nursing staff in a position to deal with the complexity and demands that this type of treatment.
Keywords: Nursing; neoplasms; radiotherapy; nursing care.
INTRODUCTION
According to estimates, more than 12 million cancer cases worldwide are diagnosed annually, causing more than seven million deaths. The World Health Organization (WHO) points out that, by the year 2030, we can expect 27 million incident cases and some 17 million deaths from this disease 1. Cancer represents an important cause of mortality is understood as a major public health problem. In Brazil, estimates for the 2016/17 biennium indicate the occurrence of 600 thousand new cases of cancer2.
Because this is a complex disease, its treatment requires a comprehensive approach, because tumor cells tend to be very aggressive and uncontrollable 3. Aiming at the cure or improvement in the standard of living of cancer patients, different therapeutic modalities have been made available, among them, radiotherapy, a resource that has improved the prognosis of many neoplasias. Radiotherapy consists in the use of electromagnetic or corpuscular ionizing energy to generate interaction in neoplastic cells. According to data, it is believed that about 50% of cancer patients may at some point be able to use radiotherapy at some stage of treatment4,5.
Although radiotherapy has effective results, it brings certain acute and chronic clinical manifestations, known as adverse effects, that can be noticed during and after its application. These effects are seen mainly in the skin, an organ that has cells with fast cycle cell division, a respectable factor for radiosensitivity and radiocurability. Thus the skin is the first tissue to reveal adverse reactions to ionizing radiation 3.
The reactions induced by this therapeutic modality are seen as an inevitable part of this treatment, and the nurse is the professional who must assist the patient in order to slow down the adverse skin signs and symptoms, as well as other alterations that may arise. This makes the nursing team fundamental in educational and preventive actions, active in the intervention in order to minimize the toxicities of radiation 3,6.
The Federal Nursing Council (COFEn), through the Resolution nº 211/1998, establishes the role of the nursing professional in radiotherapy, and affirms that nurses must be inserted in a broad manner in care, management and educational plans. In the case of radiotherapy, it is the responsibility of these professionals to plan, organize, supervise, perform and evaluate all nursing activities involving clients submitted to ionizing radiation, as well as to fully assist patients and their families, based on the Code of Ethics of Nursing professionals and current legislation, since this is a highly complex procedure7.
Based on the premise of the challenges of working with radiotherapeutic patients and their families, and considering the scarcity of studies related to the actions of nurses in this therapy, the present study aimed to know the role of nurses in radiotherapy reference services of two hospitals of the city of Recife.
LITERATURE REVIEW
Radiation therapy is defined as a treatment modality that employs a beam of ionizing radiation appropriate to destroy tumor cells by acting on their deoxyribonucleic acid (DNA), with the least acceptable change in surrounding normal cells. Used as a local therapeutic method for cancer, it is indicated to be applied exclusively or associated with other types of treatment such as chemotherapy and surgery, and can be curative, prophylactic, palliative or ablative5,6.
As the skin has rapid cell division cycle, it reacts to ionizing radiation in around 95% of patients. Radiodermatitis thus represents one of the most common adverse effects during radiotherapeutic treatment, with possibility of alopecia, mucositis and xerostomia. There is therefore a need for a qualified nurses to clarify patients on the guidelines to prevent such reactions and effectively treat them8,9.
The COFEn Resolution nº 389/2011 establishes that the assistance to cancer patients must be provided by specialized nursing professionals, who have deep scientific knowledge and technical skills to solve more complex clinical situations10.
Through this practice, the assistance should promote a relationship of trust, by offering quality and humanized care in order to soothe the effects caused by the treatment. Therefore, it is necessary that nurses acquire knowledge of all radiotherapy stages, conducting their activities safely, through critical reasoning and the best analysis of patient care 11.
METHODOLOGY
This is a descriptive, cross-sectional study with quantitative approach carried out in reference hospitals in Pernambuco.
The State of Pernambuco presents 11 reference oncology hospitals, but only five of them offer radiotherapy services, and only two have the participation of nurses12. Therefore, these two hospitals were chosen as the present study sites. The institutions will be referred as hospital 1 and hospital 2 henceforth; the first is a philanthropic entity and the second, a private and charitable organization, both located in the city of Recife.
Eight nurses who had been working in the radiotherapy services for at least six months in the selected institutions and who agreed to participate in the research and signed the Informed Consent Form (ICF) participated in the study.
The data collection instrument was a structured questionnaire, elaborated according to the National Institute of Cancer (INCA)4 and observation of the practice of nurses in radiotherapy services. The questionnaire had 40 closed questions and was divided into four sections: the first covered characteristics of the sociodemographic and professional academic profile of the nurses (gender, age, graduation, post-graduation, number of jobs, daily work hours, and time of action in radiotherapy); the second, third and fourth sections included specific actions, respectively: nursing supervision, consultation and intervention. Data collection was held between June and July 2015, with previous schedule of date and time for presentation of the research objectives, adapted to the availability of the professionals, and after their agreement by signing the ICF, and schedule of a new date for interviews.
Data were tabulated and analyzed by means of descriptive statistics, and presented as simple and absolute frequencies, to which the MS-Excel software version 2010 was used, and later interpreted and compared with the literature.
The research is in accordance with Resolution nº 466/12 of the National Health Council/Ministry of Health (NHC/MOH) and its project was approved by the Research Ethics Committee of the Oswaldo Cruz University Hospital/Cardiological Emergency Center of Pernambuco, CAAE n° 45920115.4.0000.5192.
RESULTS AND DISCUSSION
Data analysis was initially structured by the characterization of the profile of the nurses in the radiotherapy services, followed by the critic of the results related to specific activities - nursing supervision, consultation and intervention.
Characterization of the nurses' profile
The analysis of sociodemographic information pointed to a total of female participants. This fact comes from the predominance of the historical attribute of nursing, which has been a profession practiced almost only by women, since its beginning13. All nurses were less than 40 years old; of these, 5 (62.5%) were aged between 20-29 years and 3 (37.5%) between 30-39 years.
It was observed 100% of the professionals trained in private institutions, what is corroborated by another study14, and justified by the expansion of Higher Education in Brazil, especially in private institutions, a factor that clarifies this market disposition.
As for improvement training, 4 (50%) of the participants reported having specialization lato sensu completed in the area of oncology, and 4 (50%) declared that they are undergoing specialization courses. There was no mention of post-graduate studies at the master's or doctoral level ( stricto sensu).
A positive fact is the presence of interest in qualification at postgraduate level, in the lato sensu modality, taking into account that the national curricular guidelines in the higher institutions recommend the formation of the generalist nurses, not specifically addressing the teaching of oncology. This is a specialized field, and the training offered by the undergraduate courses for nurses is often insufficient15.
Regarding the number of jobs, the results show that 6 (75%) nurses had one job and two (25%) had two jobs. However, all of them perform professional functions within a workload of 40 hours per week. This is opposite to the requests for workload by the category, which is 30 hours per week for nurses. The health of these workers can be impaired due to the excessive hourly load, and the distance from the social and familiar life, making them vulnerable to stress16.
As indicators of experience on the theme studied, it was noticed that, in relation to the time of action in the sector, only 3 (37.5%) had more than two years of experience in radiotherapy services. The time working in the area may be indicative of experience and relative maturity, as reflects the knowledge and aptitude in a given period. Thus, clinical nursing experience is fundamental to the quality of care17.
The nurses' role in nursing supervision
The understanding of the nurses' role in different areas allows the elucidation of their professional role in care and the confirmation of their importance for the quality of the service. In the context of health activities, nurses perform functions related to caring, educating, coordinating, collaborating and supervising. These functions are performed, in most cases, in an integrated and simultaneous manner18.
According to Law nº 7,498/86 of June 25, 1986, the Federal Nursing Council is responsible for the planning, organization, coordination, execution and evaluation of nursing care services. This determines that the nursing supervisor has a managerial and supervisory role, and is responsible for coordinating the work unit, grouping the nursing team members and organizing the available resources to provide qualified and satisfactory care to patients, families and staff19.
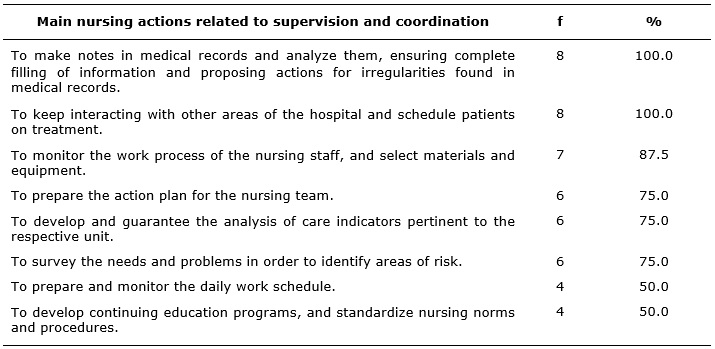
The main actions performed by nurses in the position of supervision in the radiotherapy sectors of the two hospitals surveyed are specified in Table 1.
TABLE 1: Main supervision actions performed by nurses in the radiotherapy sectors
in two referral hospitals. Recife – Pernambuco, 2015. 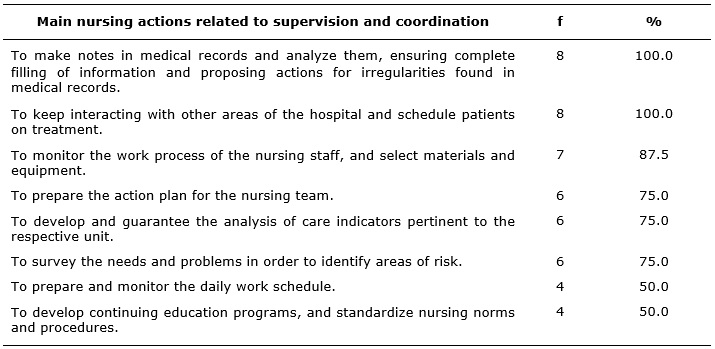
Among the competencies of nurses in radiotherapy established by COFEn Resolution nº 211/98, the function to record information and statistical data pertinent to nursing care stands out8. Table 1 shows that all interviewees comply with what is established by COFEn, whose main activities included: to make annotations in medical records, analyzing and ensuring their complete filling; propose actions for irregularities detected in medical records; and maintain interaction with the other hospital sectors, guaranteeing the quality of services, in a sectorized and global manner.
Also in this sphere, nurses evaluate the use of available resources and technologies, analyzing safety rules, effectiveness, the benefit/social impact relationship, highlighting the ethical aspects in the various situations, with the purpose of making decisions that benefit primarily the patient, the professionals and the work environment20. Thus, 7 (87.5%) respondents stated that they monitor the work process of the nursing staff and select materials and equipment so that efficient treatment is achieved.
It was verified, in the two analyzed institutions, that all interviewees have to schedule the patients undergoing treatment, a relevant activity in the administrative scope of the nurses' role. The coordination of the scheduling of patients under treatment is a dynamic action, with emphasis on the active search in order to understand the individual needs of clients 21.
An important practice, carried out by 6 (75%) nurses, is the development and assurance of the analysis of care indicators pertinent to the respective unit, as well as the investigation of needs and problems, in order to identify risk areas. The survey of performance indicators and the search for improvements through scientific technical updating and the use of radioprotection devices and technologies allows these professionals to perform with quality in various routine and/or emergency circumstances, situations that may cause physical or material harms to patients, and to the hospital unit7.
It was noticed that 6 (75%) nurses prepare the action plan for the nursing team and 4 (50%) have as duty to develop continuing education programs, to standardize nursing norms and procedures, and to prepare and monitor the daily work schedule. It is worth mentioning that training is a positive differential in the work methodology and in the results achieved by the nursing team. The actions developed by nurses reinforce what has been emphasized in the literature22.
Nursing consultation to radiotherapy patients
The nursing consultation is a activity exclusively carried out by nurses and has the aim of applying components of the scientific method to identify health/illness problems, intervene and put into practice nursing actions for health promotion and diseases/injury prevention, and for recovery of individuals, families and community. Thus, nurses must participate in therapeutic protocols, and develop, increase and transmit preventive and curative health measures through guidance to patients and their families 7,8.
The guidelines provided in the nursing consultation by nurses of this study are presented in the Table 2.
TABLE 2: Main guidelines provided by nurses in the nursing consultation to
radiotherapy patients in two referral hospitals. Recife – Pernambuco, 2015. 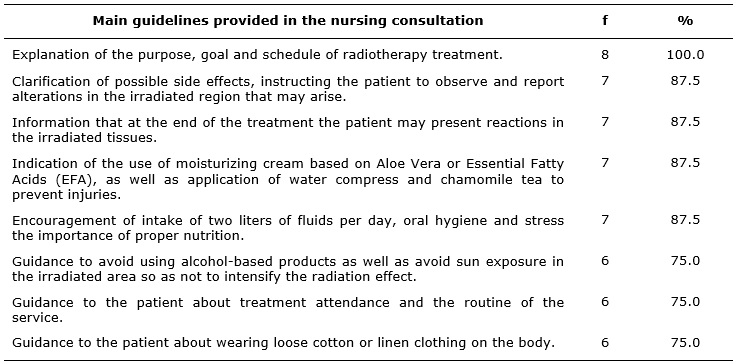
One of the main goals expressed by all nurses (100%) in the nursing consultation is to explain to the patient the purpose and objective of the treatment, as well as the entire schedule of the proposed radiotherapy treatment, and 6 (75%) of them stressed the guidance as to attendance to treatment and observation of the routine of the service as very important.
The nursing consultation stands out among the competencies of nurses acting in radiotherapy services, as this is the most practice exercised by these professionals. The effective exercise of this activity includes the evaluation of the history of each patient, the impact of the disease and the treatment on their lives and on the life of all involved. The planning of interventions needs to take into account, besides other factors, the social reality of individuals in this condition, so that information may be passed on in a clear and comprehensible way5.
It was observed that 7 (87.5%) nurses clarify the possible side effects during the consultation, advising on the importance of observing and communicating alterations that may arise in the irradiated area, and also informing that at the end of the treatment, reactions in the irradiated tissues are very likely. In view of the above, nurses provide care based on the specific conditions of each patient as well as offer them health education8.
One of the clinical manifestations of patients submitted to radiotherapy is the presence of skin reactions to radiation, called radiodermatitis. In order to minimize radiotoxicity, the nurses act according to the institutional protocol and provide guidance on preventive measures 3.
It was found that 7 (87.5%) nurses indicated the use of moisturizing creams based on Aloe Vera or Essential Fatty Acids (EFA), as well as the application of compresses of water and chamomile tea, in order to prevent the appearance of injuries. However, there was a divergence in the indication of the product in the two institutions surveyed. In hospital 1, EFA-based products are offered, while in hospital 2, Aloe Vera moisturizer is recommended, both after radiotherapy sessions. Chamomile compress was indicated in the two institutions. See Table 2.
Care protocols are intended to prevent the appearance or worsening of the degree of the radiodermatites, as well as to soothe the discomfort of the patient. The researched institutions recommend topical approaches through chamomile tea compress, Aloe Vera or EFA based moisturizers that can slow down skin reactions to radiation. However, these behaviors still lack support from scientific evidence provided by clinical research9.
Chamomile tea is used to minimize skin damage and shows good results due to its topical anti-inflammatory effect, among others. This study demonstrates that its phytotherapeutic use is notable, and this may be due to the cost-effectiveness relatioship, for its real efficacy, or even psychologic effect23.
Regarding the nursing consultation, 7 (87.5%) nurses encourage patients to ingest two liters of fluids per day, since 1,250 to 3,000 ml/day of water are required in adults, depending on age, sex, body surface and tissue mass. Thus, encouragement of water intake, for good hydration and efficacy/attenuation of the toxic effects of the treatment, is essential 24. Furthermore, nurses also guide on oral hygiene and reinforce the importance of proper nutrition.
Besides the emphasis given to care with the irradiated area, guidance is also given on what should be avoided or used during treatment: the use of alcohol-based products and sun exposure in the irradiated area is to be avoided, to prevent intensifying the effect of radiation; cotton or linen clothing, loose in the body, is to be used. These aspects are essential for achieving satisfactory results in therapy. This information was passed on by 6 (75%) nurses. Patient searches seek to obtain in the nursing consultation the maximum information about self-care and subsidies for therapeutic coping. In this way, it was verified that the nursing consultation in the radiotherapy sector provides a personalized care 6,25.
Nursing interventions
The systematization of nursing care (SNC) is a practice exclusive of nursing professionals and of fundamental importance for their work. It is divided into stages to plan, execute and evaluate the needs arising from the treatment provided to the patient. An important step of the SNC is the nursing intervention, through the care plan to be provided by the team, and that will also serve as a subsidy for the evaluation of the assistance that represents the last stage of this process26.
The results of the main nursing interventions performed in the radiotherapy sessions, according to the study sample, are shown in the Table 3.
TABLE 3: Main nursing interventions performed in the radiotherapy service of the
two researched reference hospitals. Recife – Pernambuco, 2015. (N=8) 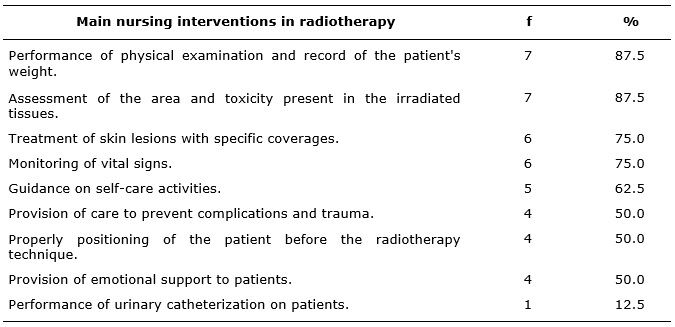
It is known that radiation therapy can cause harm to cancer patients; thus it is necessary take the complaints and clinical findings seriously during consultations, giving them proper attention, for effective treatment 4. A quality physical examination allows to collect concrete information and figures as the first intervention provided by the nursing team reported by 7 (87.5%) of the interviewees. This is preceded by verification of weighted mass, important data to be verified before treatment planning, in order to minimize adverse effects26.
Nurses integrating these services are required to be aware of the body area to be irradiated, taking into account the description of the patient, so as to improved action planning by identifying needs3.
In this perspective 7 (87.5%) professionals evaluate the irradiated area and toxicity, as well as 6 (75%) of them treat the skin lesions presented with specific coverages, according to Table 3. According to a study on the same theme, the intensity of the reaction may vary from mild erythema and pruritus, to dry or moist desquamation, and may cause tissue necrosis 3.
The other observed interventions were related to general guidelines and general care during and after the radiotherapy session: 6 (75%) nurses monitor vital signs and 4 (50%) provide care for prevention of complications and traumas, as well as the correct positioning of the patient before the procedure.
Regarding self-care, 5 (62.5%) stated that they were guiding this practice, which is extremely important for the patient at all stages of treatment. Yet, 4 (50%) of these professionals offer emotional support to the patient, demonstrating sensitivity to the importance of integral care. This attitude allows us to go beyond the biological scope, because health care also means recognizing clients and their families as unique human beings that are experiencing a difficult moment in their lives22,26-28.
The self-care advocated by Dorothea Orem has been defined as the planning of learning activities that aim to increase individual and collective knowledge and abilities in the face of perceived needs. It is the result of the guidance and attention to clients and family members regarding themselves and aims to provide accurate and concrete information about the treatment27. This action is exclusively developed by nurses and requires time, specific knowledge in the area and communication and assistance skills28.
CONCLUSION
Assistance to cancer patients has an evident complexity, since it requires the consideration of multiple aspects, such as: physical, psychological, social, cultural, spiritual and economic factors. The nursing teams of radiotherapy services have to be repared to deal with the treatment requirements and the individuality of each client.
In this study, it was possible to verify that the role of nurses is not restricted to care, but they rather perform administrative actions in the work process of the nursing staff, in the selection of materials and equipment, in scheduling consultations and planning of the systematized nursing care. These professionals also play a fundamental role in the nursing consultation, which promotes the individualization of the care and the effectiveness of the treatment for each patient.
We emphasize that, despite the limitations inherent to the reduced quantitative of the studied population, the results are in contrast with the current situation in relation to the increased survival and demand for radiotherapy, and the limited number of hospitals that provide a nursing team to aid this activity. Considering the importance of the actions provided by these professionals, complementary studies are needed on this widely known topic, on the role of nurses in radiotherapy services, besides the nursing consultation.
REFERENCES
1.Ministry of Health (Br). National Cancer Institute. 2012 Estimate: incidence of cancer in Brazil. Rio de Janeiro: INCA; 2011 [cited on Aug 12, 2016]. Available at: http://portal.saude.sp.gov.br/resources/ses/perfil/gestor/homepage/estimativas-de-incidencia-de-cancer-2012/estimativas_incidencia_cancer_2012.pdf .
2. Ministry of Health (Br). National Cancer Institute. 2016 Estimate: incidence of cancer; 2015 [cited on Aug 12, 2016]. Available at: http://www.inca.gov.br/estimativa/2016 .
3. National Cancer Institute (Br). Nursing actions for cancer control: a proposal of teaching-service integration. /. - 3rd Ed. atual. amp.; 2008 [cited on Aug 12, 2016] Available at: http://www.inca.gov.br/enfermagem/
4.Ministry of Health (Br). National Cancer Institute. Committee of standardizations. Radiotherapy and you. Brasília(DF):INCA; 2002.
5.Leite FMC, Ferreira FM, Cruz MSA, Lima EFA, Primo CC. Nursing diagnoses related to adverse effects of radiotherapy. Rev Min Enferm. 2013; [cited on Aug 12, 2016] 17 (4): 940-5. Available at: http://www.reme.org.br/artigo/details/897.
6.Araujo CRV, Rosas AMMTF. The role of the nursing team in the radiotherapy sector: a contribution to the multidisciplinary team. Rev Bras Cancerol. 2008; [cited on Aug 12, 2016] 54 (3): 231-7. Available at: http://www.inca.gov.br/rbc/n_54/v03/pdf/artigo_4_pag_231a237.pdf .
7.Federal Nursing Council (Br). Resolution nº 211/1998. It deals with the role of nursing professionals working with ionizing radiation. Rio de Janeiro: COFEN; 1998 [cited on Aug 12, 2016]. Available at: http://www.cofen.gov.br/resoluo-cofen-2111998_4258.html .
8.Andrade KBS, Francz AC, Grellmann MS, Belchior PC, Oliveira JA, Wassita DN. Nursing consultation: evaluation of self-care adherence of patients submitted to radiotherapy. Rev Enferm UERJ, 2014; [cited on Aug 12, 2016] 22(5): 622-8. Available at: http://www.facenf.uerj.br/v22n5/v22n5a07.pdf
9.Schneider F, Pedrolo E, Lind J, Schwanke AA, Danski MTR. Prevention and treatment of radiodermatitis: an integrative review. Cogitare Enferm. 2013; [cited on Aug 12, 2016] 18(3): 579-86. Available at: http://ojs.c3sl.ufpr.br/ojs/index.php/cogitare/article/view/33575 .
10.Federal Nursing Council (Br). Cofen Resolution nº 389/2011. It updates, within the scope of the Cofen System/Regional Nursing Councils, the procedures for registration of the postgraduate degree lato and stricto sensu granted to nurses and lists the specialties. Brasília (DF): [cited on Sep 10, 2016]. Available at: http://www.cofen.gov.br/resoluo-cofen-n-3892011_8036.html .
11.Egilegor JXH, Puyadena MIE, Etxabe JMU, Iraola CA. Implementation of the nursing process in a health area: models and evaluation structures used. Rev Latino-Am Nursing. 2014; [cited on Sep 10, 2016] 22(5): 772-7. Available at: http://www.scielo.br/pdf/rlae/v22n5/pt_0104-1169-rlae-22-05-00772.pdf
12. Ministry of Health (Br). National Cancer Institute (Br). Where to treat by SUS: Pernambuco. Brasília (DF): 2016; [cited on Sep 14, 2016]. Available at: http://www.inca.gov.br/wps/wcm/connect/cancer/site/tratamento/ondetratarsus/P .
13.Viana RAPP, Vargas MAO, Carmagnani MIS, Tanaka LH, Luz KR, Schmitt PH. Profile of intensive care nurses in different regions of Brazil. Texto contexto-enferm. 2014; [cited on Sep 10, 2016] 23(1): 151-9. Available at: http://www.scielo.br/scielo.php?pid=S010407072014000100151&script=sci_arttext&tlng=pt .
14.Brito AMR, Brito MJM, Gazzinelli MFC, Montenegro LC. Social representations of Undergraduate Nursing students about being a nurse. Rev Bras Enferm. 2011; [cited on Sep 10, 2016] 64(3): 527-35. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672011000300017 .
15.Amador DD, Gomes IP, Coutinho SED, Costa TNA, Collet N. Nurses' conceptions about the training in the care of children with cancer. Texto contexto-enferm. 2011; [cited on Sep 10, 2016] 20(1): 94-101. Available at: http://www.scielo.br/scielo.php?pid=S0104-07072011000100011&script=sci_abstract&tlng=pt
16.França FM, Ferrari R, Ferrari DC, Alves ED. Burnout and work aspects in the nursing team of two medium-sized hospitals. Rev Latino-Am Nursing. 2012; [cited on Sep 10, 2016] 20(5): [09 telas]. Available in: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692012000500019
17. McHugh MD, Lake E. T, Understanding clinical expertise: nurse education, experience, and the hospital context. Res Nurs Health. 2010; [cited on Sep 10, 2016] 33(4): 276-87. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2998339/pdf/nihms239174.pdf .
18.Santos FC, Camelo SHHH, Laus AM, Andrian LL. Nurses who work in hospital oncology units: profile and professional qualification. Enferm Global. 2015; [cited on Sep 10, 2016] 14(2). Available at: http://revistas.um.es/eglobal/article/viewFile/190061/174211 .
19.Federal Nursing Council (Br). Law nº 7498 of June 25, 1986. It rules on the regulation of nursing exercise and other measures. Rio de Janeiro: COFEn; 1986 [cited on Sep 10, 2016]. Available at: http://novo.portalcofen.gov.br/lei-n-749886-de-25-de-junho-de-1986_4161.html .
20.Nascimento ACEC, Pinto ALR, Pereira CRA, Souza FEP, Vieira ZRS, Andrade GDB e et al. The importance of nursing supervision in health institutions. Saúde e Pesquisa. 2013; [cited on Sep 14, 2016] 6(2): 339-43. Available at: http://periodicos.unicesumar.edu.br/index.php/saudpesq/article/view/2908
21.Carvalho E, Bollela VR. Electronic patient scheduling (EPS) as a management tool for outpatient services of a tertiary health referral service. Gestão e Saúde. 2015; [cited on Sep 14, 2016] 6(2): 1446-62. Available at: http://periodicos.unb.br/index.php/rgs/article/view/22479
22.Almeida ML, Peres AM. Knowledge, skills and attitudes about the management of nursing graduates of a Brazilian public university. Invest Educ Enferm. 2012; [cited on Sep 14, 2016] 30(1): 66-76. Available at: http://bases.bireme.br/cgi-bin/wxislind.exe/iah/online/?IsisScript=iah/iah.xis&src=google&base=LILACS&lang=p&nextAction=lnk&exprSearch=638909&indexSearch=ID .
23.Reis PED, Carvalho EC, Bueno PCP, Bastos JK. Clinical application of chamomilla recutita in phlebitis: curve study. Rev Latino-Am Nursing. 2011; [cited on Sep 14, 2016] 19(1): [08 telas]. Available at: http://www.scielo.br/scielo.php?pid=S0104-11692011000100002&script=sci_arttext&tlng=pt .
24.Cuppari L. Clinical nutrition in adults. 2nd ed. São Paulo: Manole; 2005.
25.Medina AM, Leal AF, Zavaglia GO, Muniz RM, Guimarães SRL, Faes ADR. The nursing consultation as a strategy for cancer patient care in radiotherapy treatment. Science, Care and Health. 2008; [cited on Sep 14, 2016] 7(2): 1-4. Available at: http://eduem.uem.br/ojs/index.php/CiencCuidSaude/article/viewFile/6727/pdf
26.Alvim ALS. The Nursing Process and its five stages. Enferm Foco. 2013; [cited on Sep 18, 2016] 4(2): 140-141. Available at: http://revista.portalcofen.gov.br/index.php/enfermagem/article/viewFile/531/214
27.Silva JMC, Valente Ribeiro PPS. Self-care strategies of people with cancer submitted to chemotherapy/radiotherapy and their relation to comfort. Enferm Global. 2015; [cited on Sep 18, 2016] 14(1): 372-83. Available at: http://revistas.um.es/eglobal/article/viewFile/206591/169991
28.Santos I, Jesus PBR, Brandão ES, Oliveira EB, Silva AV. Repercussions of cutaneous involvement in people's lives: sociopoetizing self-image and self-esteem. Rev enferm UERJ. 2014; [cited on Sep 18, 2016] 22(2):157-62. Available at: http://www.facenf.uerj.br/v22n2/v22n2a02.pdf