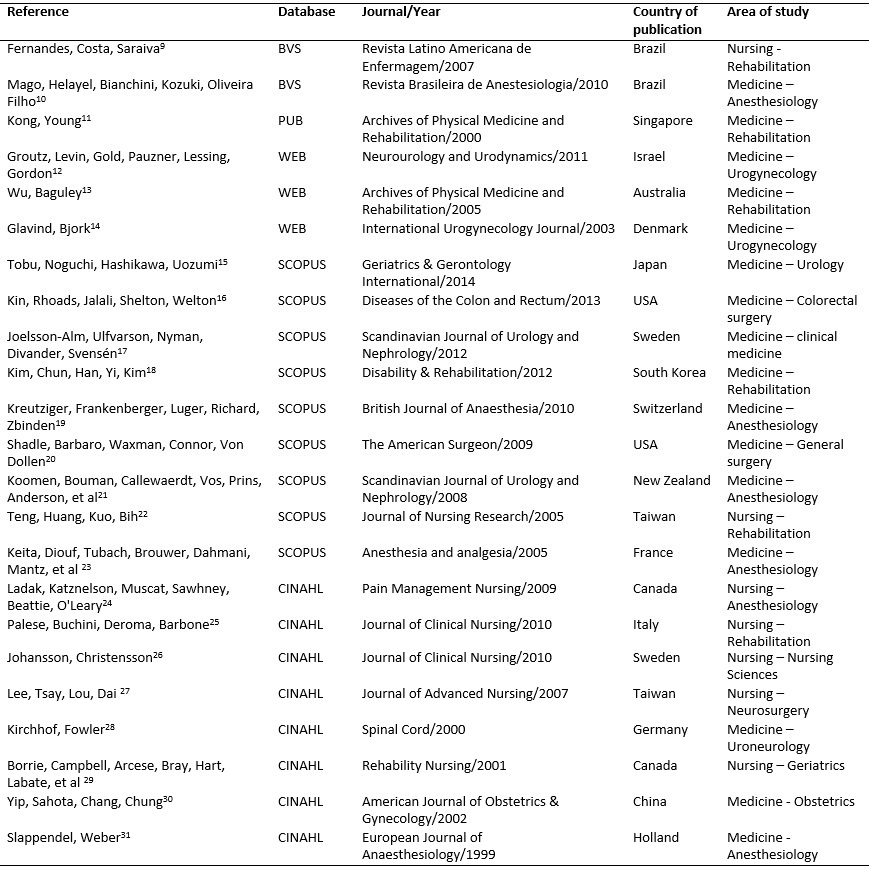
FIGURE 1: Description of studies according to number of reference/authors, database, journal/year, country of publication and area of study.
REVIEW ARTICLE
Scientific evidence of urinary retention diagnostic practices: scoping review
Beatriz Maria JorgeI; Alessandra MazzoII; Anamaria Alves NapoleãoIII; Anaísa BianchiniIV
I
Nurse. Ph.D. from the Ribeirão Preto College of Nursing, University of São
Paulo. Brazil. E-mail: beatrizjorge@usp.br
II
Nurse. Associate Professor I, Ribeirão Preto College of Nursing, University
of São Paulo. Brazil. E-mail: amazzo@eerp.usp.br
III
Nurse. Ph.D. Associate Professor, Federal University of São Carlos. Brazil.
E-mail: aa.napoleao@gmail.com
IV
Nurse. Master's student, Ribeirão Preto College of Nursing, University of
São Paulo. Brazil. E-mail: anaisa.bianchi@usp.br
DOI: https://doi.org/10.12957/reuerj.2018.25840
ABSTRACT
Objective: to identify scientific evidence on urinary retention diagnostic practices. Method: this scoping review searched the Latin American & Caribbean Health Sciences Literature, Web of Science, National Library of Medicine, Cumulative Index to Nursing and Allied Health Literature, The Cochrane Library and SCOPUS databases. Of the 2482 references found, 23 were selected. Results: the 23 articles were grouped by patient clinic (surgery, rehabilitation or obstetrics) and by urinary retention diagnostic practices (intermittent urinary catheterization, by portable bladder ultrasound, combination of portable bladder ultrasound and urinary catheterization and/or non-invasive measures). Conclusion: diagnosis of urinary retention is an issue that has been discussed for some time. However, there is still no consensus, and in practice it is often performed ineffectively.
Descriptors: Nursing; urinary retention; evaluation; diagnosis.
INTRODUCTION
Urinary retention (UR) diagnoses are a common part of nursing care practice. It is defined as the inability to empty the bladder completely or partially1.
The signs and symptoms of acute UR are sudden inability to urinate, bladder distention, and intense lower abdominal pain and discomfort. Chronic UR can be asymptomatic. In this case, the distended bladder does not contract effectively and patients are unaware that it is not completely voided2.
To diagnose UR, clinical data must be gathered through patient interviews and a physical examination of the bladder. During patient assessment, professionals must consider all the elements that determine the diagnosis. A diagnosis of UR involves assessing the patient's history of patterns of urination, inspecting the abdomen, palpating the distended lower abdomen; measuring and recording the amount of residual urine in the time intervals between voiding; assessing the quantity, frequency and aspects of the urine; and determining the balance between consumption and production, in which ingestion higher than production can indicate UR3.
However, a UR diagnosis also depends on the incorporation of clinical parameters that are difficult to assess in a physical examination and that associates unfavorable factors such as the use of medications and nervous system alterations. The physical exam of the urinary bladder includes inspection, palpation and percussion of the supra-pubic area; however, physical examination techniques do not often provide professionals with the necessary sensitivity to obtain a precise measure of the urinary volume retained in the organ. When the urinary bladder is full and can be palpated at the level of the umbilical scar, it contains approximately 500 mL of urine, but if it extends beyond this region, the retained urinary volume may reach up to 1000 mL2.
When patients are conscious and have UR, they can verbalize their pain and discomfort. However, patients with Alzheimer's disease, psychiatric disorders, comatose, under anesthesia, spinal cord injuries, under the effect of other drugs, and/or nervous system disorders may be incapable of communicating or feeling the signs and symptoms of UR3.
The effectiveness of the UR diagnosis is also affected by the examiner's subjectivity, which can lead professionals to either over or underestimate the volume of urine in the bladder. This leads to wrongful diagnoses of either presence or absence of UR and frequently, to unnecessary urinary catheterization, which leads to risk of trauma and urinary tract infection (UTI)4.
Lack of a proper theoretical framework and adequate standardization makes nursing care of UR patients prone to malpractice, negligence, and recklessness. This results in harm to patients, legal and ethical problems for professionals, and the disparaging of the professional class by society5.
Thus, to help qualify nursing care through a literature review, the aim of the present study was to identify scientific evidence about UR diagnostic practices.
METHODOLOGY
This was a scoping review carried out according to the methodology set forth by the Joanna Briggs Institute (JBI)6. To create the research question, the PICO mnemonic system was used, namely: population, intervention, comparator and outcomes7, P – patients with UR; I – assessment of UR; C – patients without UR, O – diagnosis of UR; which resulted in the following guiding question: What are the practices employed to diagnose patients with urinary retention?
The literature search was based on the following Portuguese and English descriptors and their synonyms according to the Health Sciences Descriptors (DeCS) and Medical Subject Headings (MeSH): patients (pacientes), urinary retention (retenção urinária), evaluation (avaliação) and diagnosis (diagnóstico). The databases searched were: the Latin American and Caribbean Health Science Literature (LILACS), the Web of Science, the National Library of Medicine (PubMed), the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Cochrane Library, and SCOPUS.
The authors included studies conducted with UR patients; that addressed the diagnosis of UR; with a quantitative and/or qualitative design, and which answered the research questions, regardless of the area of knowledge it was associated with. Secondary studies; nonscientific articles; information on websites and public service announcements and duplicate studies found in different databases were excluded.
The search yielded 2,482 studies, and after reading through the titles and abstracts, 47 were selected for a full reading, and of these 14 duplicates were excluded. Of the 33 articles selected for full-text analysis, 11 were excluded for not answering the research question and one study was included after assessing the references. Thus, 23 studies were selected.
Next, the data from the articles was extracted with the help of an instrument created by the researchers, as per JBI recommendations 8, which identifies the studies' publication database, journal, authors, country, year, area of study, objective, methodological design, sample details, main results, and conclusions. The studies were grouped and the results presented in the figures and the discussion.
RESULTS AND DISCUSSION
Of the 23 (100%) articles that made up the sample9-31, 2 (8.7%) were published in Portuguese and 21 (91.3%) in English. Furthermore, 7 (30.4%) were published in nursing journals, whereas 16 (69.6%) were published in medical journals.
Figure 1 presents the bibliographic characteristics of the examined articles.
FIGURE
1:
Description of studies according to number of reference/authors, database,
journal/year, country of publication and area of study.
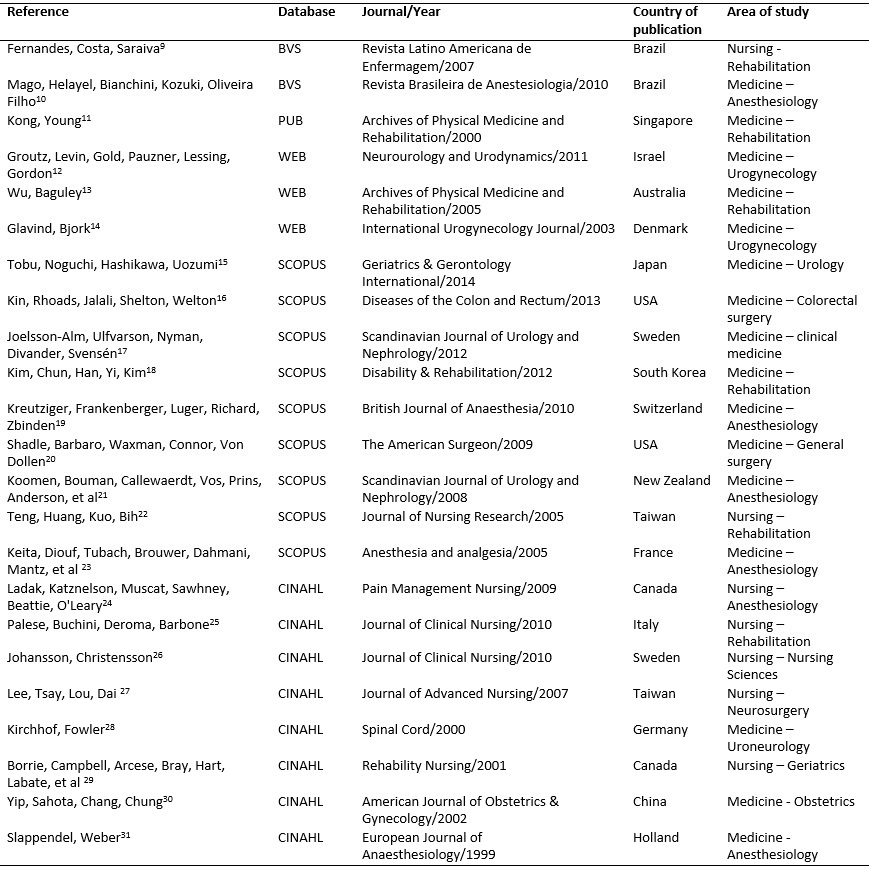
The articles are described regarding number and type of participants, UR diagnostic practice and main results and conclusions, as shown in Figure 2.
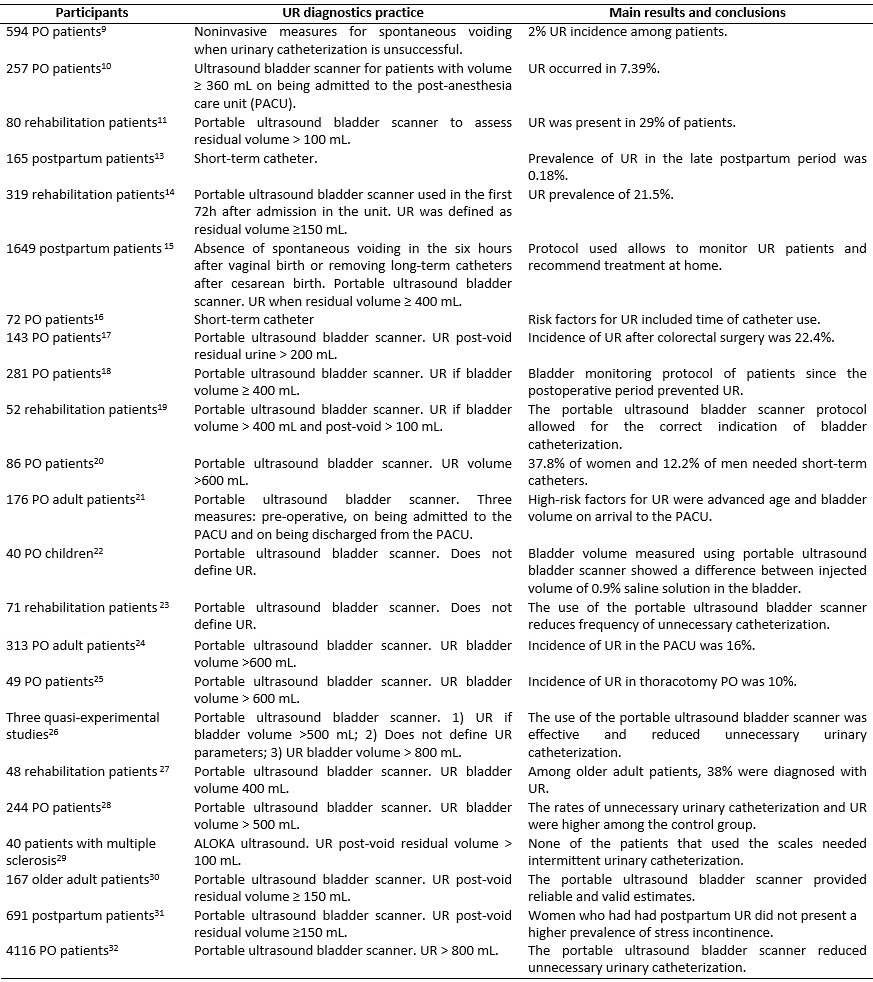
FIGURE 2:
Description of articles according to number and type of participants, UR
diagnostic practice and main results and conclusions. 2016.
Nursing care for UR can be found in different clinics and is a routine practice among nursing teams. To ensure safety and quality, it requires a precise diagnosis and appropriate interventions13.
In the present review, among the 23 (100%) studies analyzed, most were published in English, in medical journals, with emphasis on the fields of anesthetic and rehabilitation clinical practice and in countries from the American, European and Asian continents, as shown in Figure 1. Although the UR diagnosis32 is part of the systematization of nursing care, it has been poorly discussed and disseminated in the profession, especially in Brazil.
Evidence-based practice is an approach that helps improve the quality of healthcare and intensifies clinical judgment. However, to be used effectively, healthcare professionals must obtain, interpret and integrate already published results with the patient's clinical data. When care is based on this approach, interventions are more effective and the results provide improved care33.
In the studies analyzed, UR was present among postoperative (PO) adult patients; postpartum women (acute and subacute), and also among general rehabilitation, ischemic cerebral vascular accident rehabilitation, multiple sclerosis and older adults, as shown in Figure 2. To diagnose UR among these populations, only urine volume was considered. There was no consensus among most of the authors about the amount of urine retained in the bladder to qualify a diagnosis of UR.
According to the studies in the selected sample, UR in adult PO patients is usually associated with the use of regional anesthesia, such as heavy isobaric bupivacaine with morphine, lidocaine without vasoconstrictor, and ropivacaine; medications commonly used in orthopedic surgeries34 . Of the 23 (100%) studies, 13 (56.5%) were about UR in the orthopedic9,10,15,17,19,23,31, chest9,10,24, abdominal10,16,23, gynecological10, head and throat 10, vascular23, urological23 and neurological postoperative period9,27. In these patients, the parameters for UR diagnosis were difficulty in urinating and different amounts of urinary retention. The bladder volume considered to diagnose UR ranged from > 200 mL to > 800 mL of urine, or, more specifically, > 200 mL16, ≥ 360 mL10, ≥ 400 mL26,18, > 500 mL25,27, > 600 mL19,23,24 and > 800 mL 25,31.
Among postpartum women, UR can be associated with the birth itself, because of analgesia, edema and/or trauma to the bladder, edema, and trauma to the tissue surrounding the urinary meatus and/or because of decreased sensitivity to the pressure exerted by urine30. Postpartum UR can affect any woman who gives birth. Delayed postpartum UR diagnosis or treatment can lead to complications such as recurrent urinary tract infections, upper urinary tract damage, and permanent voiding difficulties. However, the lack of UR protocols and assessment has been mentioned as one of the main problems relative to the treatment of postpartum UR35.
Among the studies that addressed UR associated with obstetric clinical practices, a UR diagnosis was established with a residual urine volume ≥ 400 mL, associated with lack of spontaneous micturition six hours after vaginal birth or after removing long-term catheters in the case of cesareans14. In cases in which spontaneous urination was observed, there was still post-urination UR. In these patients, a UR diagnosis was defined with a residual volume ≥ 150 mL30.
Still according to the studies analyzed in this sample, the incidence of UR in adult patients undergoing rehabilitation processes was prevalent in association with neurological disorders, which affect the urinary excretory system. The urinary disorders resulting from neurological injuries are related to changes in the function of the detrusor muscle and external sphincter, causing post-void residual urine. The treatment goal of neurogenic urinary disorders is to protect the upper urinary tract and improve patient quality of life, and treatments are administered according to the different patterns of urinary disorders36.
Among the studies on rehabilitation, only one mentioned lack of spontaneous voiding and residual urine volume > 400 mL18. The other studies on the topic diagnosed postvoid residual urine with volumes > 100 mL11,18,28 and/or ≥ 150 mL13, 29.
In rehabilitation clinical practice, such small amounts of residual urine (>100 mL to ≥ 150 mL) used to diagnose post-void UR make the physical exam a challenge. Thus, it is a consensus for this type of practice to diagnose post-void UR using portable ultrasound bladder scanners11,13,18,22,26,28,29.
Still on this matter, an observational study conducted at a rehabilitation clinic found that clinical indicators alone were not enough to diagnose post-void UR in 20% of patients. The study also concluded that routine clinical practice, based on the identification of signs and symptoms and physical examinations, without the use of the portable ultrasound bladder scanner, resulted in a significant rate of post-void UR underdiagnosis13.
The portable ultrasound bladder scanner has been used as a non-invasive and convenient method to measure bladder volume. Its use is relatively quick, safe, painless, requires little patient cooperation and does not require specially trained professionals. It reduces stress and possible physical problems for patients. Its use is becoming routine in primary care and its benefits include less urinary catheterization and greater patient comfort and satisfaction37.
To provide quality and differentiated humanized nursing care when determining a UR diagnosis, portable ultrasound bladder scanners should be used to complement the patient's clinical examination. The use of technology must be associated with clinical assessment measures such as anamnesis (listening to the patient's complaint), and bladder inspection, palpation, and percussion.
Other ways of diagnosing UR mentioned in the studies were noninvasive and unreliable measures used with PO patients such as warm compresses applied to the suprapubic region, orthostatic positioning, and the use of running water sounds9 to induce spontaneous voiding. Invasive measures were also mentioned, such as short-term catheters for relief in obstetric practice12.
The use of short-term catheters is an invasive procedure that is associated with increased risk for UTI and trauma to the urethra. It should be conducted only when necessary, as a form of treatment and not for UR diagnosis38. All of the analyzed studies mentioned the use of the catheter as the intervention of choice for UR treatment.
With the evolution of the nursing process, the systematization of care and the attribution of nursing diagnoses require that nurses have more in-depth knowledge about basic human needs, grounded on clinical judgment and decision making39. Accurate diagnoses reflect the actual conditions of patients. It is essential to achieve accuracy in the interpretation of human responses, as it underpins the selection of interventions, which contribute to obtaining expected outcomes. When interpretations have little accuracy, errors of omission can occur, leading to patient harm40.
Achieving safer care with minimal harm requires that professionals identify, analyze and manage risks related to safety events, as they are responsible for adequately planning and conducting interventions with the goal of preserving patient safety. In other words, it is essential that more studies about UR nursing care be developed and applied.
CONCLUSION
The results of this scoping review show that UR is a topic that has captured the interest of health professionals in recent years.
There was no consensus as to UR diagnosis parameters, however, most of the evidence found in this study suggest that in postoperative, obstetrics and rehabilitation clinical practice, among patients who do not void spontaneously, UR volume is ≥400 mL and for post-void UR ≥150 mL.
Conducting an assertive UR diagnosis without the help of a portable ultrasound bladder scanner is subjective. Nonetheless, clinical practice must never be replaced and underestimated by the use of technologies.
A limitation of this study includes the use of only five electronic databases for the literature search. This may have led to the exclusion of many other existing studies. In light of the results, the authors suggest further research on the topic, especially to establish protocols to aid the clinical practice of UR diagnosis.
REFERENCES
1.Queiroz e Silva FA, Simões FA. Semiologia urológica. In: Zerati Filho M, Nardozza Júnior A, Reis RB. Urologia fundamental. São Paulo: Planmark; 2010. p. 37-46.
2.Newman DK, Willson MM. Review of intermittent catheterization and current best practices. Urol Nurs. 2011; 31(1):12-28.
3.Timby BK, Smith NE. Enfermagem médico-cirúrgica. São Paulo : Manole, 2005.
4.Van Os AF, Van der Linden PJ. Reliability of an automatic ultrasound system in the post partum period in measuring urinary retention. Acta Obstet. Gynecol. Scand. 2006; 85(5):604-7.
5.Pimenta CAM, Pastana ICASS, Sichieri K, Gonçalves MRCB, Gomes PC, Solha RKT, et al. Guia para a construção de protocolos assistenciais de enfermagem. COREN-SP. São Paulo: COREN-SP; 2015.
6.Joanna Briggs Institute (JBI). The Joanna Briggs Institute Reviewers' Manual 2015: methodology for JBI scoping reviews. New York (USA): JBI; 2015.
7.da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO strategy for the research question construction and evidence search. Rev latam enfermagem. (Online) 2007; 15(3):508-11.
8.Joanna Briggs Institute (JBI). Joanna Briggs Reviewers' Manual 2014, New York (USA): JBI;2014.
9.Fernandes MCBC, Costa VV, Saraiva RA. Postoperative urinary retention: evaluation of patients using opioids analgesic. Rev. latinoam. enferm. (Online). 2007;15(2):318-22.
10.Mago AJD, Helayel PE, Bianchini E, Kozuki H, Oliveira Filho GR. Prevalência e fatores preditivos de retenção urinária diagnosticada por ultrassonografia no período pós-anestésico imediato. Rev. Bras. Anestesiol. 2010; 60(4):387-90. doi: http://dx.doi.org/10.1590/S0034-70942010000400005.
11.Kong KH, Young S. Incidence and outcome of poststroke urinary retention: a prospective study. Arch Phys.Med. Rehabil. 2000; 81(11):1464-7.
12.Groutz A, Levin I, Gold R, Pauzner D, Lessing JB, Gordon D. Protracted postpartum urinary retention: the importance of early diagnosis and timely intervention. Neurourol. Urodyn. 2011; 30(1):83-6. doi: 10.1002/nau.20926.
13.Wu J, Baguley IJ. Urinary retention in a general rehabilitation unit: prevalence, clinical outcome, and the role of screening. Arch. Phys. Med. Rehabil. 2005; 86(9):1772-7.
14.Glavind K, Bjørk J. Incidence and treatment of urinary retention postpartum. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2003; 14(2):119-21.
15.Tobu S, Noguchi M, Hashikawa T, Uozumi J. Risk factors of postoperative urinary retention after hip surgery for femoral neck fracture in elderly women. Geriatr Gerontol Int. 2014; 14(3):636-9. doi: 10.1111/ggi.12150.
16.Kin C, Rhoads KF, Jalali M, Shelton AA, Welton ML. Predictors of postoperative urinary retention after colorectal surgery. Dis Colon Rectum. 2013; 56(6):738-46.
17.Joelsson-Alm E, Ulfvarson J, Nyman CR, Divander MB, Svensén C. Preoperative ultrasound monitoring can reduce postoperative bladder distension: a randomized study. Scand. J. Urol. Nephrol. 2012; 46(2):84-90.
18.Kim HJ, Chun MH, Han EY, Yi JH, Kim DK. The utility of a bladder scan protocol using a portable ultrasonographic device in subacute stroke patients. Disabil. Rehabil. 2012; 34(6):486-90.
19.Kreutziger J, Frankenberger B, Luger TJ, Richard S, Zbinden S. Urinary retention after spinal anaesthesia with hyperbaric prilocaine 2% in an ambulatory setting. Br. J. Anaesth. 2010; 104(5):582-6.
20.Shadle B, Barbaro C, Waxman K, Connor S, Von Dollen K. Predictors of postoperative urinary retention. Am. Surg. 2009; 75(10):922-4.
21.Koomen E, Bouman E, Callewaerdt P, Vos GD, Prins MH, Anderson BJ, et al. Evaluation of a non-invasive bladder volume measurement in children. Scand. J. Urol. Nephrol. 2008; 42(5):444-8. doi: 10.1080/00365590802054600.
22.Teng CH, Huang YH, Kuo BJ, Bih LI. Application of portable ultrasound scanners in the measurement of post-void residual urine. J. Nurs. Res. 2005; 13(3):216-24.
23.Keita H, Diouf E, Tubach F, Brouwer T, Dahmani S, Mantz J, et al. Predictive factors of early postoperative urinary retention in the postanesthesia care unit. Anesth. Analg. 2005; 101(2):592-6.
24.Ladak SS, Katznelson R, Muscat M, Sawhney M, Beattie WS, O'Leary G. Incidence of urinary retention in patients with thoracic patient-controlled epidural analgesia (TPCEA) undergoing thoracotomy. Pain Manag. Nurs. 2009; 10(2):94-8.
25.Palese A, Buchini S, Deroma L, Barbone F. The effectiveness of the ultrasound bladder scanner in reducing urinary tract infections: a meta-analysis. J. Clin. Nurs. 2010; 19(21-22):2970-9. doi: 10.1111/j.1365-2702.2010.03281.x
26.Johansson RM, Christensson L. Urinary retention in older patients in connection with hip fracture surgery. J. Clin. Nurs. 2010; 19(15-16):2110-6.
27.Lee YY, Tsay WL, Lou MF, Dai YT. The effectiveness of implementing a bladder ultrasound programme in neurosurgical units. J. Adv. Nurs. 2007; 57(2):192-200.
28.Kirchhof K, Fowler CJ. The value of the Kurtzke Functional Systems Scales in predicting incomplete bladder emptying. Spinal Cord. 2000; 38(7):409-13.
29.Borrie MJ, Campbell K, Arcese ZA, Bray J, Hart P, Labate T, et al. Urinary retention in patients in a geriatric rehabilitation unit: prevalence, risk factors, and validity of bladder scan evaluation. Rehabil.Nurs. 2001; 26(5):187-91.
30.Yip SK, Sahota D, Chang AM, Chung TK. Four-year follow- up of women who were diagnosed to have postpartum urinary retention. Am. J. Obstet. Gynecol. 2002; 187(3):648-52.
31.Slappendel R, Weber EW. Non-invasive measurement of bladder volume as an indication for bladder catheterization after orthopaedic surgery and its effect on urinary tract infections. Eur. J. Anaesthesiol. 1999; 16(8):503-6.
32.North American Nursing Diagnosis Association International. Diagnósticos de enfermagem da NANDA: definições e classificação 2005-2017. Porto Alegre (RS): Artmed; 2015.
33.Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & contexto enferm. 2008; 17(4):758-64.
34.Tanaka PP, Souza RO, Salvalaggio MFO, Tanaka MAA. Estudo Comparativo entre a bupivacaína a 0,5% e a mistura enantiomérica de bupivacaína (S75-R25) a 0,5% em anestesia peridural em pacientes submetidos a cirurgia ortopédica de membros inferiores. Rev. Bras. Anestesiol. 2003; 53(3):331-7.
35.Leach S. 'Have you had a wee yet?' Postpartum urinary retention. Pract Midwife. 2011; 14(1):23-5.
36.Rocha FET, Gomes CM. Bexiga neurogênica. In: Zerati Filho M, Nardozza Júnior A, Reis RB. Urologia Fundamental. São Paulo: Planmark; 2010. p. 239-50.
37.Nusee Z, Ibrahim N, Rus RM, Ismail H. Is portable three-dimensional ultrasound a valid technique for measurement of postpartum urinary bladder volume? Taiwan J. Obstet. Gynecol. 2014; 53(1):12-6. doi: 10.1016/j.tjog.2013.01.028.
38.Knoll BM, Wright D, Ellingson L, Kraemer L, Patire R, Kuskowski MA, et al. Reduction of inappropriate urinary catheter use at a Veterans Affairs hospital through a multifaceted quality improvement project. Clin. Infect. Dis. 2011; 52(11):1283-90. doi: 10.1093/cid/cir188.
39.Magalhães AM, Chiochetta FV. Diagnósticos de enfermagem para pacientes portadores de bexiga neurogênica. Rev. gaúch. enferm. 2002; 23(1):6-18.
40.Matos FGOA, Cruz DALM. Construção de instrumento para avaliar a acurácia diagnóstica. Rev. Esc. Enferm. USP. 2009; 43(Esp):1088-97.